PAPILLARY CARCINOMA WITH ABUNDANT CALCIFICATION WITHIN A THYROGLOSSAL DUCT CYST
2Kocaeli Üniversitesi Tıp Fakültesi, Radyoloji, Kocaeli, Türkiye
3Kocaeli Üniversitesi Tıp Fakültesi, Patoloji, Kocaeli, Türkiye
Summary
Primary carcinoma of thyroglossal duct cyst is a rare disease entity. The most common computed tomography (CT) appearance is a solid enhancing nodule with foci of calcification. The authors present a case of papillary carcinoma arising from a thyroglossal duct cyst, ultrasonography (US) and CT appearance of which was unusual as the tumor nodule was almost totally calcified.Introduction
TDC is the most common congenital midline neck mass. Between 3rd and 7th weeks of embryogenesis, the thyroid gland descends through the thyroglossal duct in the midline to reach its final position anterior to the thyroid cartilage. The thyroglossal duct then involutes and disappears by the 10th week [1,2]. Failure of involution of the duct results in a cystic mass developing from epithelial remnants of the duct as a result of accumulation of inflammatory debris and secretions [2,3]. TDC is located in the midline or slightly to one side, mostly between the thyroid gland and the hyoid bone. But it may also be located suprahyoid, suprasternal or intralingual [1].Carcinoma arising from a TDC is rare (1%) [1,3,4]. It is more common in females, mostly in adults. Mean age at presentation is 38 years [4]. The youngest reported case is an 11 year old girl [5].
The authors present a case of papillary carcinoma arising from a TDC, ultrasonography (US) and CT appearance of which was unusual as the tumor nodule was almost totally calcified.
Case Presentation
A 33 year-old woman presented with a painless anterior neck swelling 3 years ago, of which fine needle aspiration revealed dense inflammation with occasional dysplastic epithelial cells. She refused excision of the mass. Three years later the patient reapplied with the same complaint with a rapid increase in size lately. Physical examination revealed a solid, mobile, non-tender anterior neck mass of 3 x 3 cm., located between the hyoid bone and thyroid cartilage (Figure 1.a,b). There was no cervical lymphadenopathy.
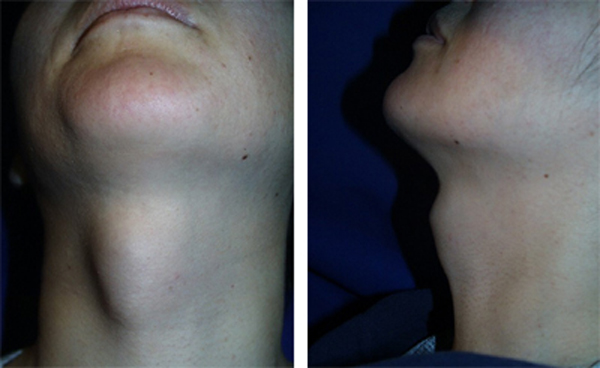 Büyütmek İçin Tıklayın |
Figure 1: a,b Midline neck mass is seen. |
US examination revealed a right paramedian multilocular cystic mass with a large focus of calcification. The mass showed thick septations, but no prominent solid component (Figure 2). On CT the cyst walls and septae showed slight enhancement (Figure 3.a,b). US and scintigraphy of the thyroid gland, and laboratory tests were normal. Fine needle aspiration of the mass was suspicious for malignancy.
 Büyütmek İçin Tıklayın |
Figure 2: US shows a multilocular cystic mass with thick septations. Note the near-totally calcified tumor nodule with heavy acoustic shadowing. |
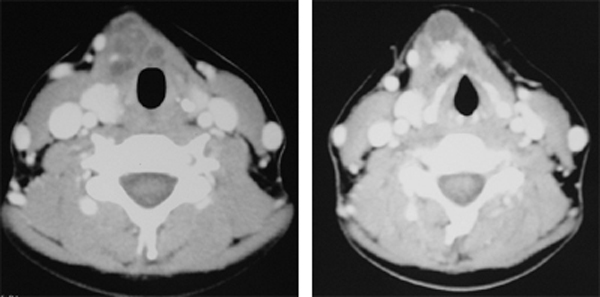 Büyütmek İçin Tıklayın |
Figure 3: a,b Axial contrast enhanced CT shows enhancement of the cyst walls and septae (a). Note the tumor nodule was almost totally calcified (b). |
The patient underwent Sistrunk operation. There was no sign of local invasion. The resected specimen was tan-brown soft tissue 5.5x3x2.5 cm in dimension with hyoid bone attached to it. On sections, an irregular cystic area approximately one cm in diameter with gritty areas was detected. Surrounding fibrous tissue was unremarkable. Histopathologically, cystic area consisted of papillary structures lined by epithelial cells having eosinophilic cytoplasm and ground glass nuclei with grooves and inclusions. The hyalinized cores and the tips of the papillary structures had prominent calcium deposition either in form of psammoma bodies or irregular non-lamellated calcifications (Figure 4. a) The surrounding areas had occasional benign thyroid follicles and prominent inflammatory fibrous stroma without any calcification (Figure 4. b).Additionally, there was a reactive lymph node measuring 0.7 cm within the resected specimen. Based on the pathological findings the case was diagnosed as thyroid papillary carcinoma arising within a thyroglossal duct cyst. The patient received no further treatment. During the first 36-months of follow-up, there was no evidence of local and regional or distant metastasis.
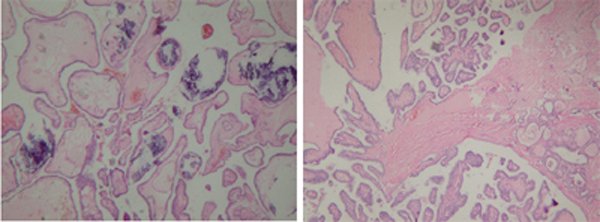 Büyütmek İçin Tıklayın |
Figure 4: a,b Histologic sections shows a papillary tumor with prominent calcification (a, H&E x200). The tumor extends into the cystic cavity. The surrounding tissue consisted benign thyroid follicles and fibrous inflammatory stroma (b, H&E x100). |
Discussion
Papillary carcinoma is the most frequent (92%) histologic type among tumors arising from a TDC [6]. It is still controversial if this is a primary carcinoma of TDC or metastasis from occult thyroid cancer [1,4].TDC is easily recognized clinically, however clinical differentiation of malignant transformation is difficult. Dysphagia, dysphonia, palpable cervical lymph nodes, sudden enlargement of the cyst should raise suspicion of malignancy [1,2,7]. Radiologic imaging and fine needle aspiration biopsy help in case of suspicious malignancy, but malignant transformation is usually occult until histopathologic examination [1-4,7]. Therefore each TDC should be evaluated with fine needle aspiration biopsy and prior to the resection of a symptomatic TDC, the thyroid gland should be examined carefully, because in 10-40 % of patients malignant foci are also found in the thyroid [7].
Carcinoma arising in TDC has different CT appearances. There may only be a cystic mass with a thin enhancing wall, with no sings of malignancy. More commonly, it presents with a solid dense or enhancing mural nodule, calcification, irregular margins and a thick wall [1,8,9]. A solid nodule is highly suspicious of malignancy, but it has also been reported to represent chronic inflammation, fibrosis and reactive papillary structures [3]. High density fluid content of a TDC does not necessarily represent malignancy, but rather proteinaceous content, internal cellular debris, or chronic inflammation [3,10].
The shape and the location of the calcification is not helpful in determining the malignant potential. In a report of 6 patients with papillary thyroid carcinoma within the TDC, 2 had irregular calcifications throughout the mass and two had foci of calcification on a mural nodule [9]. Samara et al [1] reported peripheral speckled calcification in a solid nodule which was shown to represent psammomatous calcifications of a papillary thyroid carcinoma. In our case the tumor nodule was almost totally calcified. Kervancioglu et al [3] reported calcification in the wall and within the cyst in a case of TDC with chronic inflammatory changes without malignant transformation.
Tretment is surgical excision. The widely accepted procedure of choice is Sistrunk operation [1,6]. Sistrunk procedure is en bloc excision of the cyst, the middle part of the hyoid bone and soft tissues along the course of the thyroglossal duct to the level of the foramen caecum [1,8]. Before Sistrunk operation it must be confirmed that 1. the tumor is confined to the walls of the cyst, 2. there is no clinical and scintigraphic evidence of thyroid gland malignancy, 3. there is no metastatic cervical lymph nodes [1,6,8]. Sistrunk procedure reduces the risk of recurrence of the cyst and may reduce the risk of recurrence of the tumor as the duct may provide a route for spread of the tumor [11]. However there is still no clear consensus whether (near-)total thyroidectomy and postoperative radioactive iodine therapy together with suppressive doses of thyroid hormone should follow Sistrunk procedure [12].
Reference
1) Samara C, Bechrakis I, Kavadias S, Papadopoulos A, Maniatis V, Strigaris K. Thyroglossal duct cyst carcinoma: case report and review of the literature, with emphasis on CT findings. Neuroradiology 2001;43:647-9. [ Özet ]
2) Van Vuuren PAC, Balm AJM, Gregor RT, Hilgers FJM, Loftus BM,Delprat CC, et al. Carcinoma arising in thyroglossal remnants. Clin Otolaryngol 1994;19:509-15. [ Özet ]
3) Kervancioglu R, Bayram MM, Özkur A, Bakir K. A thyroglossal duct cyst with calcification. Neuroradiology 2000;42:923-5. [ Özet ]
4) Weiss SD, Orlich CC. Primary papillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg 1991;78:87-9. [ Özet ]
5) Yoo KS, Chengazi VU, Omara RE. Thyroglossal duct cyst with papillary carcinoma in an 11-year-old girl. J Pediatr Surg 1998;33:745-6. [ Özet ]
6) Patel SG, Escrig M, Shaha AR, Singh B, Shah JP. Management of well-differentiated thyroid carcinoma presenting within a thyroglossal duct cyst. J Surg Oncol 2002;79:134-41. [ Özet ]
7) Martin PM, Burguna GM, Echevarria IC, Martinez PD. Papillary carcinoma arising in a thyroglossal duct cyst:report of two cases. J Oral Maxillofac Surg 1993;51:89-93. 8) Wigley TL, Chonkich GD, Wat BY. Papillary carcinoma arising in a thyroglossal duct cyst: Otolaryngol Head Neck Surg 1997; 116: 386-8. [ Özet ]
9) Branstetter BF, Weissman JL, Kennedy TL, Whitaker M. The CT appearance of thyroglossal duct cyst carcinoma. AJNR 2000; 21:1547-50. [ Özet ]
10) Ahuja AT, King AD, King W, Metreweli C. Thyroglossal duct cysts:sonographic appearances in adults. AJNR 1999;20:579-82. [ Özet ]
11) Mulhall KJ, OHanlon DM, Mortimer G, Quill DS. Papillary carcinoma arising in a thyroglossal duct remnant-a review of thyroglossal surgery in a regional centre in the west of Ireland. Ir J Med Sci 1998;167:212-5. [ Özet ]
12) Dedivitis RA, Guimaraes AV. Papillary thyroid carcinoma in thyroglossal duct cyst. Int Surg 2000; 85:198-201. [ Özet ]




