TİROGLOSAL DUKTUS KİSTİ İÇİNDE PAPİLLER KARSİNOMA, İKİ OLGU SUNUMU
2GATA Haydarpaşa Eğitim Hastanesi, Patoloji, İSTANBUL, Türkiye
Özet
Papiller karsinomanın tiroglosal duktus kisti içinde yerleşimi nadirdir. Sistrunk ameliyatı uyguladıgımız iki tiroglosal duktus kistili olgumuzda, patolojik olarak papiller karsinoma tanısı konuldu. Cerrahi sınırlarda tümöre rastlanmadı ve kapsüler invazyon yoktu. Postoperatif yapılan tiroid sintigrafileri normaldi ve bilgisayarlı tomografide servikal lenfadenopatiye rastlanmadı. Olgulardan biri 5 diğerinin 2 yıllık takibinde patolojik bulgu saptanmadı. Tiroglosal duktus kisti içinde yerleşimli papiller karsinomada başlangıç tedavisi olarak sistrunk ameliyatı yeterlidir. İleri cerrahi tedavi tiroid nodülü ya da boyunda lenf nodu olmasına bağlıdır. Postoperatif radyoaktif iyot ablasyon tedavisi rekürrens ve metastaz görülen olgularda düşünülmelidir.Giriş
A persistent thyroglossal duct is estimated to be found in 7 % of the general population [1-3]. Thyroglossal duct remnants are the most common midline neck masses in childhood, representing more than 75% of such masses [4]. They are usually located in the midline cervical region at the level of the hyoid bone.The incidence of malignant transformation in a thyroglossal duct cyst (TDC) varies from 0.7 to 1% [5]. Approximately 225 cases of malignant tumors in TDCs have been reported to date since the first case was identified by Bretano in 1911. We report an additional two cases of carcinoma in a TDC.
Sistrunk procedure is accepted as the operation of choice for thyroglossal duct cysts, with the lowest known recurrence rate [6]. However, there is still controversy about the sufficiency of this procedure for the treatment of papillary carcinoma in TDC.
Olgu Sunumu
CASE REPORT 1A 25 year-old woman presented with a neck mass that had been present for 3 months. Clinical examination revealed a smooth, mobile 1x1 cm nodule located just superior to the thyroid cartilage. The mass had upward movement with swallowing. The thyroid gland was normal by palpation and no neck lymph nodes were found. No abnormalities were noted on the skin.
Cervical ultrasound showed a hypoechoic, midline 1x2 cm cervical lesion that was compatible with the findings of a TDC. Axial computed tomography (CT) scans of the neck at the level of hyoid bone demonstrated a cystic mass with central calcification and enhancing solid areas. There was no cervical lymphadenopathy.
A Sistrunk procedure was performed and a 2.0 x 1.5 x 2.0 cm encapsulated cystic mass was excised. Histopathological examination of the specimen revealed a cystic structure surrounded by a thick fibrous capsule and lined with benign thyroid follicules within the cyst wall. The inner surface showed papillary projections into the lumen consistent with papillary carcinoma. There was no capsule invasion and the margins were negative (Figure 1).
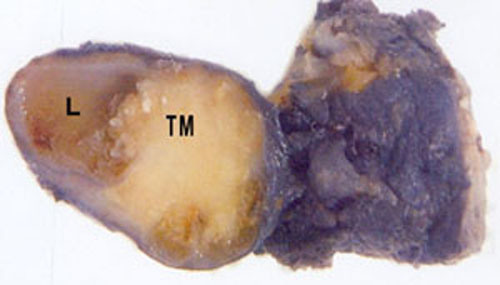 Büyütmek İçin Tıklayın |
Figure 1: Macroscopic view of the resected specimen. L: Lumen TM: Papillary carcinoma. |
The patient tolerated the procedure well. Postoperative thyroid scintigraphy was normal and the thyroglobulin level was 2.3 ng/ ml. Thyroid stimulating hormone (TSH) suppression was not applied postoperatively. The patient has been followed up for two years with no further evidence of disease.
CASE REPORT 2
A 40 year-old woman presented with one year history of a painless, enlarging submental mass. Clinical examination revealed a 3.0 cm elastic mobile mass at the midline in the submental region. This mass moved vertically on protrusion of the tongue. The rest of the head and neck exam was unremarkable.
Axial CT scan of the neck revealed a heterogeneous cystic mass measuring 3.0 x 2.0cm. There was no cervical adenopathy and the thyroid was normal.
The patient underwent a Sistrunk procedure and a 3.0 x 2.0 x 2.0 cm encapsulated cystic mass with a smooth outer surface was excised. Histopathological examination revealed a cystic sealed with stratified and cubic epithelium (Figure 2). Papillary ingrowths consistent with papillary carcinoma were noted within the lumen of the cyst. Psammoma bodies were also seen. There was no capsule invasion and the margins were negative.
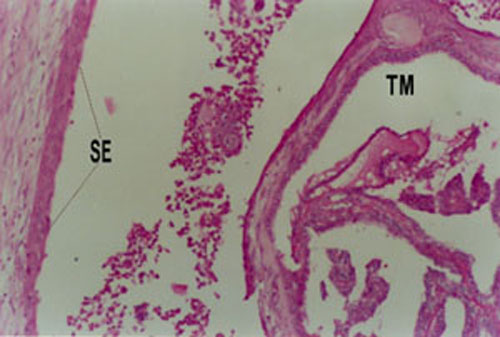 Büyütmek İçin Tıklayın |
Figure 2: Photomicrograph of the thyroglossal duct cyst capsule surfaced by squamous epithelial cells (SE) and papillary carcinoma within the cyst (TM), (H&E; x200). |
The patient tolerated the procedure well. Postoperative thyroid scintigraphy was normal and the thyroglobulin level was 5.1 ng/ ml. TSH suppression was not applied postoperatively. The patient has been followed up for five years with no further evidence of disease.
Tartışma
The thyroid anlage develops during 3-4 week of gestation from the floor of the primitive pharynx at the site of the foramen cecum. From this point, it descends from the bottom of the pharynx to the level of first tracheal cartilage by 7-8 weeks. The thyroglossal duct which is formed during migration usually disappears during 9-10 week of gestation. Occasionally, remnants of this duct may persist and give rise to thyroglossal cyst, sinus or ectopic thyroid.62% of TDCs harbor ectopic rests of thyroid tissue[7]. Rarely, these rests may be the only thyroid tissue in the body. Neoplasms may arise from these rests or the lining epithelium of the cyst[1]. The most common histological types of TDC carcinoma are papillary carcinoma (81.7%), mixed papillary-follicular carcinoma (6.9%) and squamous cell carcinoma (5.2%) (8). Papillary carcinoma is the most common histologic subtype with a slight female preponderance (Female:Male=3:2)(9). Allard [10] reported an age range from 6 years to 81 years for TDC carcinoma, with an average of 39.2 years. Papillary carcinoma of the thyroid presents in the fourth and fifth decades with a male-female ratio of 1:3 [11].
Papillary carcinoma of a TDC usually presents as an asymptomatic mass. Uncommonly, dysphagia, voice change and draining cutaneous sinuses may bring the patient to medical attention[12]. Neoplasia must be suspected in cases of TDC with recent changes in the clinical course[5]. Sudden enlargement may be predictive of hemorrhage within lumen as well as painful growth may be indicative of an infection. However, if TDCs are hard, fixed, irregular or have undergone size change with palpable lymph nodes, carcinoma should be suspected[8]. Imaging studies do not allow for full preoperative diagnosis and fine needle aspiration (FNA) yields a correct result in only 66% of the cases[13]. The diagnosis of TDC carcinoma is generally made postoperatively by histopathological examination of the resected tissues.
Calcifications within the cyst wall is a characteristic feature of papillary carcinoma[14]. Cyst wall invasion is seen in 21% of patients[15]. Regional lymph node metastasis has been reported in 7.7% to 12.9% of the malignant cases[2]. In our cases the histological examination of the resected specimens did not reveal any calcification.
The Sistrunk operatioon is generally considered adequate for treatment of TDC malignancies [3]. However, if abnormalities are detected in the thyroid gland by palpation or ultrasound, then a thyroidectomy must be considered, since the reported incidence of primary thyroid carcinoma concomitant with TDC carcinoma is between 11 and 33%[5]. Total or subtotal thyroidectomy has been recommended if there is cystic wall invasion by the carcinoma, or if the thyroglossal duct cyst carcinoma is greater than 1.0 cm, because larger lesions are more likely to behave aggressively[16]. Evidence of local invasion or cervical metastasis as indicated by preoperative imaging or surgical findings warrants total thyroidectomy and cervical lymph node dissection in addition to complete wide excision of the TDC carcinoma[17]. In such cases, thyroid scintigraphy and radioiodine ablation should be considered for a possible aberrant thyroid tissue[14].
The incidence of papillary carcinoma arising in a TDC is rare. CT, ultrasound, scintigraphy and FNA are helpful tests for diagnosis and staging of neoplasms occuring within TDC. Surgical excision by the Sistrunk procedure is an adequate treatment. However one must consider the possibility of concomitant thyroid gland malignancy and examine lymph node metastasis. In case of any suspicion of malignancy, thyroidectomy and/or postoperative radioiodine ablation are indicated to eliminate persistent disease. Long-term followup is necessary.
Kaynaklar
1) Datar S, Patanakar T, Armao D, Mukherji SK. Papillary carcinoma in a giant thyroglossal duct cyst. Clinical Imaging. 2000;24(2):75-77. [ Özet ]
2) Chu YC, Han JY, Han HS, Kim JM, Min SK, Kim YM. Primary papillary carcinoma arising in a thyroglossal duct cyst. Yonsei Medical Journal. 2000;43(3):381-384. [ Özet ]
3) Walton BR, Koch KE. Presentation and management of a thyroglossal duct cyst with a papillary carcinoma. South Med J. 1997;90(7):758-761. [ Özet ]
4) Tunkel DE, Domenech EE. Radioisotope scanning of the thyroid gland prior to thyroglossal duct cyst excision. Arch Otolaryngol Head Neck Surg. 1998;124:597-599. [ Özet ]
5) Martins AS, Melo GM, Tincani AJ, Lage HT, Matos PS. Papillary carcinoma in a thyroglossal duct: case report. Sao Paulo Med J. 1999;117(6):248-50. [ Özet ]
6) Ghaneim A, Atkins P. The management of thyroglossal duct cysts. Int J Clin Pract. 1997;51:512-513. [ Özet ]
7) Kennedy TL, Whitaker M, Wadih G. Thyroglossal cyst carcinoma: a rational approach to management. Laryngoscope. 1998;108:1154-1158. [ Özet ]
8) Naghavi SE, Jalali MM. Papillary carcinoma of thyroglossal duct cyst. Med Sci Monit. 2003;9(7):67-70. [ Özet ]
9) Weiss SD, Orlich CC. Primary papillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg. 1991;78:87-89. [ Özet ]
10) Allard RHB. The thyroglossal cyst. Head Neck Surg. 1982;5:134-146. PMID: 7169333
11) Schwartz MR. Pathology of the Thyroid and Parathyroid Glands. The Otolaryngologic Clinics of North America. 1990;23(2):192. [ Özet ]
12) Yoo KS, Chengazi VU, O'Mara RE. Thyroglossal duct cyst with papillary carcinoma in an 11-year-old girl. J Pediatr Surg. 1998;33:745-746. [ Özet ]
13) Bardales RH, Suhrland MJ, Korourian S, et al. Cytologic findings in thyroglossal duct carcinoma. Am J Clin Pathol. 1996;106:615-9. [ Özet ]
14) Baysungur SV, Okur E, Halezeroğlu S, Atasalihli A. Papillary carcinoma arising on cervico-mediastinal thyroglossal duct cyst resected via transcervical and partial upper sternotomy incision. Eur J Cardiothorac Surg. 2002;22(5):842-4. [ Özet ]
15) Weiss SD, Orlich CC. Primary papillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg. 1991;78:87-89. [ Özet ]
16) Heshmati HM, Fatourechi V, Heerden JA, et al. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc. 1997;72:315-9. [ Özet ]
17) Pribitkin EA, Friedman O. Papillary carcinoma in a thyroglossal duct remnant. Arch Otolaryngol Head Neck Surg. 2002;128(4):461-2; discussion 463-4. [ Özet ]




