PLATELET TO LYMPHOCYTE RATIO MAY BE HELPFUL TO PREDICT POST-TONSILLECTOMY BLEEDING IN OSAS PATIENTS
2İzmir Ekol Hastanesi, KBB, İzmir, Turkey
Summary
Objective: We aimed to investigate hematological parameters of adult patients who had undergone tonsillectomy due to chronic/recurrent tonsillitis or upper airway obstruction and determine the parameters that might help predict post-tonsillectomy bleeding.Materials and Methods: One hundred and twenty-eight adult patients who had undergone tonsillectomy between January 2014 and March 2020 were included in this retrospective study.
Demographic information, indications for surgery, postoperative complications, hemoglobin level, counts of neutrophil, lymphocyte, and platelet as well as Neutrophil to Lymphocyte Ratio (NLR) and Platelet to Lymphocyte Ratio (PLR) values of each patient were recorded.
Results: Of the patients, 45.3% (n: 58) had undergone tonsillectomy owing to chronic/recurrent tonsillitis (CRT) and 54.7% (n: 70) owing to obstructive sleep apnea syndrome (OSAS). Hemoglobin level and lymphocyte count were significantly higher in the OSAS group while the CRT group had greater NLR and PLR values (p<0.001, p=0.006, p=0.027, and p<0,001 respectively). Post-operative bleeding occurred in 11.7% of the patients (n:15). In the OSAS group, PLR was significantly higher in the patients who had postoperative bleeding compared to those who did not (124.6±30.0 and 103.2±33.0 respectively, p=0.033). In adult patients who underwent tonsillectomy because of OSAS, a PLR value higher than 121.7 is predictive of bleeding with 70% sensitivity and 79% specificity.
Conclusion: Higher PLR and NLR values may be beneficial to diagnosing CRT. A high preoperative PLR value may help predict post-tonsillectomy bleeding in OSAS patients.
Introduction
Tonsillectomy is one of the most common surgical procedures for otolaryngologists. In the pre-antibiotic era, tonsillectomy was used as a primary treatment option for tonsillitis and its complications.[1] As the administration of antibiotics has vastly reduced the number of tonsillectomies performed for infectious conditions, upper airway obstruction has become the main indication to perform a tonsillectomy in pediatric patients.[2] On the other hand, chronic tonsillitis is still the chief indication in adult patients, followed by obstruction and tumor suspicion.[3,4]Although considered a simple procedure, tonsillectomy has some serious life-threatening complications.[4] Bleeding is one of the most fearsome complications of tonsillectomy and occurs in 5% of the patients.[3] Bleeding often ends up with reoperation and causes prolonged hospital stay.[3,4] Preoperative assessment of post-tonsillectomy hemorrhage risk may be beneficial so as to be precautious and inform patients. Although some previous studies showed that adulthood, male gender, and tonsillectomy due to chronic tonsillitis are associated with an increased risk of bleeding, it is not likely yet to predict post-tonsillectomy hemorrhage.[5,6]
A complete blood count (CBC) is routinely performed before tonsillectomy. NLR and PLR could easily be calculated from a peripheral blood sample without any additional expense and have been frequently used as inflammatory markers in various research (e.g., nasal polyposis, head and neck malignities) in the field of otorhinolaryngology.[7-11] In this study, we aimed to investigate hematological parameters of adult patients who had undergone tonsillectomy due to CRT or upper airway obstruction and determine the parameters that might help predict post-tonsillectomy bleeding.
Methods
This retrospective study was conducted under the ethical principles stated in the Declaration of Helsinki and approved by the local ethical committee of Gazi University with decision number 01.03.2021-205. Adult patients who had undergone tonsillectomy between January 2014 and March 2020 were included in the study. All the surgical procedures were performed by the same surgeons with bipolar diathermy tonsillectomy technique. Since CRT and OSAS comprised the majority of indications, patients who had undergone tonsillectomy because of other indications such as tumor or tumor suspicion were excluded. Patients under any medication that could predispose them to bleeding and patients with medical conditions that might lead to systemic inflammation were also excluded.None of the surgeries were performed during active infection. A hundred and twenty-eight patients who met the criteria were included in the study. Medical records of the patients were obtained from their files and the electronic hospital information system. Demographic information, date, indications for surgery, postoperative complications, hemoglobin level, counts of neutrophil, lymphocyte, and platelet as well as PLR and NLR values of each patient were recorded. Hematologic parameters were compared between CRT and OSAS groups and between patients who had post-operative bleeding and who did not.
Statistical analysis was performed with IBM SPSS v22 software (IBM Corporation, Armonk, NY, USA). The Shapiro-Wilk test was used to assess normality. Mann Whitney U test was used for non-parametric numerical data and the chi-square test for nominal data. Hematologic parameters were analyzed through the ROC curve method to determine a cut-off value that could predict complications. Spearman correlation was used to evaluate relationships between ordinal variables. A "p" value less than 0.05 was considered statistically significant in all the statistical analyses.
Results
One hundred and twenty-eight patients were included in the study. Of the patients, 45.3% (n: 58) had undergone tonsillectomy due to CRT and 54.7% (n: 70) due to OSAS. All the patients who had undergone tonsillectomy over OSAS had an apnea-hypopnea index (AHI) score greater than 5 [mean 25.91±11.98, min-max (11.6-82.7)]. In the OSAS group, a lateral pharyngoplasty was also implemented for all the patients. The mean age of the patients in CRT and OSAS groups were 29.5±9.3 and 37.5±9.1 respectively and the difference was statistically significant (p=0.000). In the CRT group, 43.1% of the patients (n:25) were male and 56.9% (n:33) were female while 82.9% of the patients (n:58) were male and 17.1% (n=12) were female in the OSAS group. The proportion of male patients in the OSAS group was significantly higher than that of the CRT group (p=0.000).Of all the patients, 11.7% (n:15) had post-operative bleeding whereby all the cases occurred in the tonsillar bed within 7.9±2.9 days on average following tonsillectomy (min: 5, max: 14 days). In the CRT group, 8.6% of the patients (n:5) had postoperative bleeding and three of them needed a second operation to control it whereas 14.3% of the patients (n:10) in the OSAS group suffered from post-operative bleeding and five of them underwent an additional operation to manage it. None of the patients required a blood transfusion. The difference between the groups in terms of postoperative bleeding rates was not statistically significant (p=0.323). Thirty-two patients were operated on in spring, 23 in summer, 40 in fall, and 33 in winter. Bleeding rates according to seasons were 12.5% (n=4), 13% (n=3), 10% (n=4), and 12.1% (n=4) respectively. There was no statistically significant difference (p=0.870).
A comparison of hematologic parameters between CRT and OSAS groups was shown in Table 1. Hemoglobin level and lymphocyte count were significantly higher in the OSAS group while the CRT group had greater NLR and PLR values.
Table 1: Comparison of hematologic parameters between groups
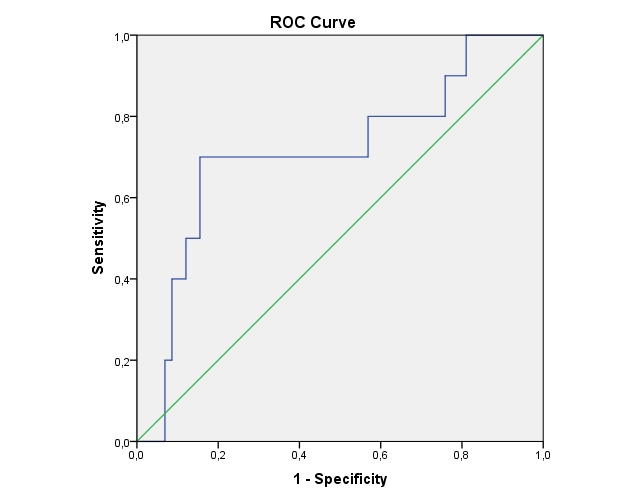
In the CRT group, age, sex, and hematologic parameters did not differ between patients who had postoperative bleeding and who did not. However, in the OSAS group, patients who suffered from postoperative bleeding had significantly higher hemoglobin level and PLR value compared to those who did not (Table 2). ROC curve analysis demonstrated that a PLR value higher than 121.7 is predictive of bleeding with 70% sensitivity and 79% specificity (Area under curve=0.71, 95% CI, 0.52-0.90) in the OSAS group (Figure 1). A comparison of hematologic parameters between patients who had postoperative bleeding and who did not in the CRT group was presented in Table 3.
 Büyütmek İçin Tıklayın |
Figure 1: ROC curve of PLR in OSAS patients who had post-tonsillectomy bleeding. The area under the curve is 0.71 (95% CI, 0.52-0.90 p<0,05) |
The AHI scores did not show a statistically significant correlation with PLR and NLR values (p=0.202). Moreover, there was no significant relationship between the AHI score and postoperative bleeding (p=0.056).
Discussion
Tonsillectomy remains one of the most widespread operations performed in ear, nose, and throat (ENT) practice. For adult patients, CRT is the main indication for tonsillectomy followed by obstruction and tumor suspicion.[3,4] In thisinves study, however, OSAS was the major indication for tonsillectomy followed by CRT. This finding is consistent with the fact that one of the senior authors of this research mostly performs surgery over OSAS.Due to the high frequency of tonsillectomy, post-tonsillectomy complications are also seen relatively frequently. Bleeding is one of the most serious complications of tonsillectomy and may be life-threatening. Post-tonsillectomy bleeding occurs in around 5% of all adult tonsillectomies but in some series, it may go up to 16.5%.[12,13] In this study, overall postoperative bleeding rate was 11.7% but only half of them needed a second operation to control the bleeding. Hoddeson et al.[3] reported that tonsillectomy due to recurrent tonsillitis has a greater risk of bleeding compared to tonsillectomy due to obstruction (6% and 4% respectively). Ikoma et al.[6] also found a higher postoperative bleeding rate in the CRT group compared to patients who underwent tonsillectomy due to obstruction (16.4% and 4.4% respectively). In this study, patients who had undergone tonsillectomy over OSAS had a higher rate of bleeding compared to the CRT group (14.3% and 8.6% respectively). Although postoperative bleeding occurred in the tonsillar bed in both groups, lateral pharyngoplasty might be the reason why the bleeding rate was greater in the OSAS group since unlike the patients in the CRT group, all the patients in the OSAS group had undergone lateral pharyngoplasty. Further studies may be beneficial so as to investigate the effect of lateral pharyngoplasty on post-tonsillectomy bleeding.
CBC and coagulation parameters were routinely obtained from all the patients who had undergone tonsillectomy preoperatively. NLR and PLR could easily be calculated from CBC results and have been frequently used in recent literature to show the inflammatory status of the subjects for various diseases.[8,14,15]
In this study, the OSAS group had a greater hemoglobin level, which was probably caused by its high ratio of male patients. On the other hand, NLR and PLR values were higher in the CRT group, which was consistent with the chronic inflammatory nature of CRT. Yenigün[8] reported that children who underwent tonsillectomy over chronic tonsillitis had higher NLR values than those who underwent tonsillectomy due to obstruction (1.98 and 1.35 respectively) and after the tonsillectomy, NLR values decreased in chronic tonsillitis group. Besides, Yorulmaz et al.[16] found higher values of PLR and NLR in pediatric patients who underwent tonsillectomy because of chronic tonsillitis compared to control group (NLR: 1.48 and 1.05; PLR: 102.77 and 91.47 respectively). In this regard, high NLR and PLR values are thought to be diagnostic markers for CRT.
Some previous studies showed that adulthood, male gender, and tonsillectomy due to CRT are associated with an increased risk of bleeding.[5,6] In this study, age, sex, and hematologic parameters did not differ between patients in the CRT group who had post-operative bleeding and who did not. On the other hand, in the OSAS group, hemoglobin level and PLR value were higher in the patients who suffered from post-operative bleeding compared to those who did not. Yıldız et al.[17] compared NLR and PLR values of pediatric patients who had postoperative bleeding with those of a healthy control group and found that PLR value was significantly higher in children with postoperative bleeding (127 and 95.2). However, it should be noted that they compared patients who had postoperative bleeding with a completely healthy group, and they did not classify patients according to tonsillectomy indications, which might be considered a limitation[17].
Various techniques and instruments have evolved to aid in tonsillectomy, including bipolar diathermy dissection, harmonic ultrasonic dissection, laser dissection, and the coblation method. In the current study all the surgeries were performed with bipolar diathermy dissection. Bipolar diathermy dissection is preferred because of low cost, shorter surgery time and minimal intraoperative bleeding. The studies in the literature showed no difference in post tonsillectomy bleeding rates between different techniques.[18,19]
Tonsillotomy is considered a safe and effective alternative to tonsillectomy for many patients, especially children, due to its less invasive nature and quicker recovery period.[20] Tonsillotomy has been shown to have a positive impact on obstructive symptoms and quality of life, similar to tonsillectomy.[21] Therefore, tonsillotomy has become a strong alternative treatment method for OSAS.
This study has limitations that should be discussed. Platelet and neutrophil counts may change rapidly. They also vary according to calibration status of measuring devices and the time of the day that the blood sample was obtained. In addition, some parameters (e.g., patients" smoking status, postoperative dehydration, use of nonsteroidal anti-inflammatory drugs) that may affect post-tonsillectomy bleeding were not discussed in this study owing to the lack of information in the patient files. Additionally, the power of the study decreased due to the small number of patients. Studies with larger populations may be beneficial.
To our knowledge, this is the first study in literature to investigate NLR and PLR values as predictors of postoperative bleeding in adult patients. In this study, we found that a PLR value higher than 121.7 is predictive of bleeding with 70% sensitivity and 79% specificity in adult patients who underwent tonsillectomy because of OSAS. Since it is an inexpensive and easy-to-use method, preoperative PLR calculation may be advantageous in terms of evaluating the risk of bleeding after tonsillectomy in OSAS patients.
Reference
1) Nguyen BK, Quraishi HA. Tonsillectomy and Adenoidectomy - Pediatric Clinics of North America. Pediatr Clin North Am. 2022 Apr;69(2):247-259. [ Özet ]
2) Smith SL, Pereira KD. Tonsillectomy in children: indications, diagnosis and complications. ORL J Otorhinolaryngol Relat Spec. 2007;69(6):336-339. [ Özet ]
3) Karaman M, Tek A, Tuncel A, Oysu C, Sheidaei S. Adult tonsillectomy: relationship between indications and postoperative hemorrhage. Kulak Burun Bogaz Ihtis Derg. 2012 Jan-Feb;22(1):21-5.. [ Özet ]
4) Galindo Torres BP, De Miguel García F, Whyte Orozco J. Tonsillectomy in adults: Analysis of indications and complications. Auris Nasus Larynx. 2018;45(3):517-521. [ Özet ]
5) Windfuhr JP, Chen YS, Remmert S. Hemorrhage following tonsillectomy and adenoidectomy in 15,218 patients. Otolaryngol Head Neck Surg. 2005;132(2):281-286. [ Özet ]
6) Ikoma R, Sakane S, Niwa K, Kanetaka S, Kawano T, Oridate N. Risk factors for post-tonsillectomy hemorrhage. Auris Nasus Larynx. 2014;41(4):376-379. [ Özet ]
7) Duzlu M, Karamert R, Tutar H, Karaloglu F, Sahin M, Cevizci R. Neutrophil-lymphocyte ratio findings and larynx carcinoma: a preliminary study in Turkey. Asian Pac J Cancer Prev. 2015;16(1):351-354. [ Özet ]
8) Yenigun A. The efficacy of tonsillectomy in chronic tonsillitis patients as demonstrated by the neutrophil-to-lymphocyte ratio. J Laryngol Otol. 2015;129(4):386-391. [ Özet ]
9) Roxburgh CS, McMillan DC. Role of systemic inflammatory response in predicting survival in patients with primary operable cancer. Future Oncol. 2010;6(1):149-163. [ Özet ]
10) Sivrice ME, Okur E, Yasan H, Tüz M, Kumbul Y, Akın V. Can the systemic immune inflammation index preoperatively predict nasal polyp subtypes? Eur Arch Otorhinolaryngol. 2020;277(11):3045-3050. [ Özet ]
11) Woodley N, Rogers ADG, Turnbull K, et al. Prognostic scores in laryngeal cancer. Eur Arch Otorhinolaryngol. 2022;279(7):3705-3715. [ Özet ]
12) Álvarez Palacios I, González-Orús Álvarez-Morujo R, Alonso Martínez C, Ayala Mejías A, Arenas Brítez O. Postoperative Pain in Adult Tonsillectomy: Is There Any Difference Between the Technique? Indian J Otolaryngol Head Neck Surg. 2017;69(2):187-193. [ Özet ]
13) Blakley BW. Post-tonsillectomy bleeding: how much is too much? Otolaryngol Head Neck Surg. 2009;140(3):288-290. [ Özet ]
14) Torun S, Tunc BD, Suvak B, et al. Assessment of neutrophil-lymphocyte ratio in ulcerative colitis: a promising marker in predicting disease severity. Clin Res Hepatol Gastroenterol. 2012;36(5):491-497. [ Özet ]
15) Qin B, Ma N, Tang Q, et al. Neutrophil to lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR) were useful markers in assessment of inflammatory response and disease activity in SLE patients. Mod Rheumatol. 2016;26(3):372-376. [ Özet ]
16) Yorulmaz M, Tüz M, Yasan H, Okur E, Sivrice M. Comparison of neutrophil/lymphocyte ratio and trombocyte/lymphocyte ratio values between tonsillectomy and a control group. Journal Of Clinical And Analytical Medicine. 2017;8(4):280-283.
17) Yildiz E, Kahveci O, Ulu S, Koca H. Can neutrophil-lymphocyte, platelet-lymphocyte ratio and mean platelet volume be marker in tonsil hemorrhage? Medicine Science 2019;8(3):720-722.
18) Liu G, Xiao C, Zhou X, Liu F. Plasma Ablation vs Other Hot Techniques for Tonsillectomy: A Meta-analysis. Otolaryngol Head Neck Surg. 2020. [ Özet ]
19) Subasi B, Oghan F, Tasli H, Akbal S, Karaman NE. Comparison of three tonsillectomy techniques in children. Eur Arch Otorhinolaryngol. 2021 Jun;278(6):2011-2015. [ Özet ]
20) Attard S, Carney AS. Paediatric patient bleeding and pain outcomes following subtotal (tonsillotomy) and total tonsillectomy: a 10-year consecutive, single surgeon series. ANZ J Surg. 2020 Dec;90(12):2532-2536. [ Özet ]
21) Mesolella M, Allosso S, Coronella V, Massimilla EA, Mansi N, Motta G, Salerno G, Motta G. Extracapsular Tonsillectomy versus Intracapsular Tonsillotomy in Paediatric Patients with OSAS. J Pers Med. 2023 May 8;13(5):806. [ Özet ]




