DO SEASONAL VARIATIONS HAVE ANY IMPACT ON THE INCIDENCE OF BENIGN PAROXYSMAL POSITIONAL VERTIGO?
Summary
Objective: The objective of the present study is to investigate the hypothesized association between seasonal variations and the incidence of benign paroxysmal positional vertigo (BPPV).Method: The study was conducted in the "Vestibular System Laboratory" of our otorhinolaryngology department between June 1st, 2021, and May 31st, 2022. We excluded patients who showed abnormal findings during their otoscopic examination. The Dix-Hallpike maneuver, supine roll test, and head-hanging test were utilized for the diagnosis of BPPV. Epley, Semont, barbeque roll, Guffoni, and Yacavino maneuvers were performed for the treatment.
Results: A total of 1,650 patients were included in our study. Of all patients, 69.9% (n: 1,153) were female and 30.1% (n: 497) were male. Among the female patients, the incidence of BPPV was 17.7% (n: 204). The percentage of patients diagnosed with BPPV was 20.9% (n: 104) in the male group. The incidence of BPPV was found to be unaffected by seasonal variations both in the female (p=0.806) and the male (p=0.468) patient groups. The number of BPPV detections was not different among the months of the year in men (p=0.794) or women (p=0.615). When the total of the patients was evaluated, there was no difference in the number of monthly BPPV detections (p=0.475).
Conclusion: The seasonal variations throughout the year were found to have no impact on the incidence of BPPV in the present study. However, when the female and male patients were compared, the incidence of BPPV was found to be significantly higher in the female group.
Introduction
Benign paroxysmal positional vertigo (BPPV) is one of the main causes of dizziness [1]. Nystagmus and vertigo occur following translocation of the otoliths that detach from the utricular macula and enter into the semicircular canals. An angular rotation of the head causes movement of the endolymphatic fluid and creates an action potential within the vestibular nerve fibers through deflection of the cupula secondary to this movement. The otoliths, however, may inadvertently alter this mechanism and create a unique situation in which an ongoing feeling of rotation is still perceived by the patient even after his or her head rotation has halted. Dislodged otoliths cause activation of the vestibular end organ by either clinging to the cupula and deflecting it or keeping their motion within the endolymphatic fluid even after the cessation of the fluid movement due to their distinct inertial properties [2].The quality of life is significantly affected in patients suffering from BPPV. The ability of the patient to perform daily tasks is highly compromised and the falling risk is considerably increased in BPPV [3]. The most commonly used tests for the diagnosis of BPPV are the Dix-Hallpike test and the supine roll test. The involvement of posterior (pSSC) and anterior semicircular canals (aSSC) is assessed by a positive Dix-Hallpike test characterized by the presence of torsional nystagmus that can be observed following a brief latent period. BPPV affecting the lateral semicircular canal (LSCC) is diagnosed by a positive supine roll test. Following a latent period, vertigo and geotropic or ageotropic nystagmus may be observed [4,5].
The main objectives of the present study were to determine the overall incidence of BPPV, to investigate the possible association between BPPV and seasonal alterations, to analyze the gender-specific distribution of BPPV, and to assess the incidence of involvement of distinct semicircular canals in BPPV. We aimed to investigate the incidence of BPPV during winter and spring to test the implications of viral infections and allergic reactions. Additionally, the study analyzed the impact of hormonal and autoimmune changes specific to gender on the overall incidence.
Methods
In this cross-sectional study, patients with a complaint of dizziness who were either admitted to our department or referred to our vestibular system laboratory for further investigation by the other departments in our hospital were included in the study. The study was conducted in the "Vestibular System Laboratory" of our otorhinolaryngology department located in a tertiary care university hospital between June 1st, 2021, and May 31st, 2022. Ethical committee approval (No: 2021/220) was obtained from the ethics committee of our hospital. In addition, consent was obtained from the patients regarding their approval to be included in the study. Enrolled patients were categorized by month and season to study BPPV incidence over time. In addition, gender-specific subgroups were formed to analyze the association between BPPV incidence and gender.
Patient Selection
Vertigo patients with any accompanying pathological otoscopic findings were excluded. Other exclusion criteria included the presence of a history of cervical or lumbar disc herniation, loss of cervical lordosis, and a previous surgical operation involving the insertion of screws, plaques, etc. into the vertebral column or intervertebral discs.
Diagnostics
Before the otoscopic examination, a detailed medical history was obtained from each patient. After the completion of the neuro-otological evaluation, dynamic positional tests were performed.
In the Dix-Hallpike maneuver, the patient's head was turned 45 degrees to the right to test the right posterior SCC and hung down to a maximum of 30 degrees. After a latent period in this position, if the patient had a torsional right-upward beating nystagmus and dizziness, the Dix-Hallpike test was assumed to be positive for the right PSCC. To test the left posterior SCC, the patient's head was turned 45 degrees to the left and hung down to a maximum of 30 degrees. After a latent period in this position, if the patient had torsional left-upward beating nystagmus, he or she was accepted to have a positive Dix-Hallpike test for left PSCC involvement.
To detect an LSCC pathology, a supine roll test (Pagnini-McClure maneuver) was performed. The ideal head position for the test should provide the LSCCs in a plane that is perpendicular to the floor and parallel to the gravitational forces. The patient was brought to a supine position and the examining table was inclined 30 degrees (reverse Trendelenburg position). After assuming this position, the patient's head was turned 90 degrees to the right. Following a latent period, the presence of dizziness or a horizontal geotropic or apogeotropic nystagmus was noted. The same procedure was applied to the left side. In the presence of unilateral geotropic nystagmus, symptoms emerged when the affected ear was facing the floor. When diagnosing patients with bilateral geotropic nystagmus, the severity of vertigo and nystagmus on both sides is noted. The affected ear was the side that exhibited more severe symptoms during testing. For patients with bilateral apogeotropic nystagmus, the ear on the side opposite to the tested side where the more intense symptoms were observed was considered the affected ear. For the diagnosis of Anterior SCC, the Dix-Hallpike or Head Hanging test is considered positive if torsional and down-beating nystagmus is observed.
Treatment
Appropriate maneuvers were performed to liberate the otoliths stuck in the SCCs, as described previously in the literature. Epley and Semont maneuvers were performed for posterior SCC involvement and 360 degrees Barbeque Roll and Guffoni maneuvers were performed for lateral SCC involvement. For anterior SCC involvement, Yacavino maneuver was performed.
Checkups
Upon elimination of the nystagmus after liberatory repositioning maneuvers, the patients were scheduled to be called again the following week. In the next visit, dynamic positional tests were applied, and the presence or absence of nystagmus or vertigo was recorded. Patients who had persistent symptoms and findings underwent repositioning maneuvers and were rescheduled for a control visit in the following week. All patients who did not have any symptoms in control visits were evaluated by a phone call after 30 days and questioned for the presence of nausea, dizziness, and blurred vision.
Statistical Analysis
Descriptive data were presented as n (%). Also, the Chi-square goodness of fit test was used to test the deviation from expected values, and the Chi-square test was used to test two proportions. All statistical calculations were performed with Jamovi 2.3.18 statistical software.
Results
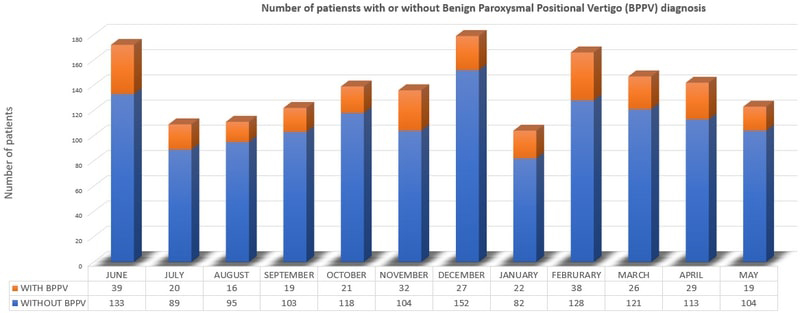
A total of 1,650 patients were enrolled in our study. Of the patients, 69.9% (n: 1,153) were female and 30.1% (n: 497) were male. Two-hundred-four (17.7%) of the women were diagnosed with BPPV, while 104 (20.9%) were diagnosed with BPPV. The number of BPPV cases was significantly higher among women than among men (p<0.001).There was no difference in the number of monthly BPPV detections in women (p=0.794). Similarly, the number of monthly BPPV detections was not significant in men (p=0.615). When the total of patients was evaluated, there was no difference in terms of the number of monthly BPPV detections (p=0.475) (Figure 1).
 Büyütmek İçin Tıklayın |
Figure 1: Number of patients in each month |
When the patients diagnosed with BPPV were examined by seasons, no seasonal difference was observed in female patients (p=0.806) or male patients (p=0.468) (Table 1). The seasonal distribution of patients with BPPV by gender is given in Table 1.
Table 1: Number of BPPV cases by seasonal variations and gender
Of the patients with BPPV, 243 (78.9%) were diagnosed with posterior canal, 56 (18.2%) with lateral canal, and 9 (2.9%) with anterior canal BPPV. Anterior canal BPPV patients were few, and these patients were excluded from the evaluation. There was no significant difference in the right and left side incidence of posterior and lateral canal BPPV (p>0.05).
Discussion
BPPV is one of the main causes of peripheral vertigo. There are limited and contradictory findings in the literature on whether there is a relationship between BPPV frequency and seasonal variations [6-9]. Jeong et al. [6] reported in their study of 1,216 patients that they did not find any difference in BPPV among seasons or months of the year and between the genders. Maia et al. [7] studied 214 patients diagnosed with BPPV and found that the frequency of the disease increased in autumn and winter. Koparal et al. [8] reported a higher incidence of the disease during the winter months in their study on 5,432 patients without subgrouping the causes of peripheral vertigo. In a multicenter study conducted by 116 ENT clinics in Germany on 20,720 patients diagnosed with peripheral vertigo (3,459 Meniere, 11,153 BPPV, and 6,108 vestibular neuritis), no seasonal difference was observed in the incidence of any peripheral vertigo disease [9]. The incidence of BPPV in women was found to be 70%, which was consistent with our study [9]. In the present study, no relationship was observed between BPPV incidence and seasonal variations or air temperature in the region.The current research did not find any significant association between the incidence of BPPV and seasonal variations. This could be due to the unique characteristics of the geographic region where the study was conducted. Istanbul experiences inter-seasonal transitions, with slight differences in the average seasonal temperatures, regular rainfall, and an average humidity level greater than 50% throughout the year. This finding suggests that a viral etiology may not be the cause of BPPV, or it could be a result of even distribution of viral infections in a region where winters and autumns are not severe [10].
The findings of our study could not indicate an association between allergy and BPPV incidence. We believe that the allergic flora remained relatively unchanged during seasonal transitions in our region. Different results can be expected in other regions, like Ankara, where the continental climate is more predominant, with significant variations in air temperature, humidity level, and the number of rainy days per year. In regions where the number of sunny days and average humidity level throughout the year is higher, like Antalya, the possibility of obtaining different outcomes is also high [10].
In terms of the gender distribution of the incidence of BPPV, the studies in the literature either found similar BPPV incidences among men and women [6,11] or significantly higher incidence among women [9,12,13]. In their study, Adegbiji et al., reported the incidence of BPPV in female patients was higher with a ratio of 1.2:1 [11]. Von Brevern et al., found that of 80 BPPV patients, 56 were females and 24 were males [12]. The findings of another study which investigated 11.153 patients. by Seidel et al. indicated that, 69.6 % of their study population were female [9]. Meghji et al diagnosed 339 BPPV patients and the number of female and male patients were found to be 250 and 89, respectively [13]. No study found significantly higher BPPV incidence among men. In the present study, the incidence of BPPV was 30.1% among men and 69.9% among women. The rate of male-to-female patients was 1:2.32. This finding was in concordance with the previous studies that pointed out a higher incidence of BPPV in female patients. In the literature, the increased incidence of BPPV in females was attributed to otoconial demineralization which is aggravated by osteoporosis and osteopenia [12,14,15]. In addition to this hypothesis, we believe that autoimmune hyperreactivity and hormonal alterations may also be responsible for the increased numbers.
BPPV is more common in middle-to-old age adults [8,16]. Oh et al. [16] found that the average age of patients with BPPV was 54.7 years. Koparal et al. [8] reported that the average age of male patients with peripheral vertigo was 47.1 years, which was 45.05 years in female patients. Consistent with the literature, the average age of the patients who complained of dizziness in the present study was 47.39. The average age of male patients was 48.54 years while the average age of female patients was 46.88 years. Likewise, the average age of all patients with BPPV was 53.45 while the average age of male patients was 53.65 and the average age of female patients was 53.34 years. There was no significant difference in terms of the average age of male and female patients with dizziness or BPPV (p>0.05).
The incidence of BPPV was reported in numerous studies in the literature [11,12,17]. In the study conducted by Von Breven et al. [12], 8% of the patients with dizziness were found to have BPPV. Adegbiji et al. [11] concluded that this rate was extremely low (1.9%). In the study conducted by Çelebisoy et al. [17], the rate was 13.2%. In our study, the rate was 18.6%. The fact that we observed a higher incidence rate compared to other studies may be related to the presence of a "Vestibular System Laboratory" in our clinic, which provided counseling for the patients who applied to our emergency department about BPPV and allowed their timely application to our clinic without a delay. As a consequence, the patient's awareness of BPPV was increased and the necessary clinical interventions could be performed easily and on time.
Regarding the affected canals in BPPV, Vaduva et al. [18] found that posterior SCC involvement was 86.7%, lateral SCC involvement was 6.9% and anterior SCC involvement was 6.4%. In their study, Çelebisoy et al. [17] reported that posterior SCC was involved in 87.9%, lateral SCC in 8.9%, and anterior SCC in 1.3%. In the present study, posterior SCC was involved in 78.9% of the patients while lateral SCC was involved in 18.2%, and anterior SCC was involved in 2.9%. In concordance with the previous studies, posterior SCC involvement was also higher in our study. This could be because otoconia are more likely to fall into the posterior SCC due to the combined action of gravitational forces and the anatomical location of the pSCC. Unlike the pSCC, gravitational forces make it almost impossible for the otoconia to fall into the aSCC.
Conclusion
In the present study, the incidence of BPPV was found not to be affected by seasonal variations in our region. Therefore, no association between BPPV and allergic or viral factors could be established. This finding can be attributable to the specific climate characteristics of our region. We believe that large-scale studies should be conducted in our region and the other regions that display distinct climate characteristics to better understand an underlying climate association.The incidence of BPPV was found to be significantly higher in female subjects, which can be attributable to osteopenia and autoimmune or hormonal alterations. Further studies that aim to investigate the association between gender and BPPV incidence should be elucidated.
FINANCIAL AND TECHNIC SUPPORT
The authors received no financial support for the research, authorship, and/or publication of this article and have no conflicts of interest to disclose.
Reference
1) Bhattacharyya N, Baugh RF, Orvidas L, Barrs D, Bronston LJ, Cass S, Haidari J. Clinical Practice Guideline: Benign Paroxysmal Positional Vertigo. Otolaryngol Head Neck Surg. 2008; 139(5 Suppl 4): S47-81. [ Özet ]
2) Parnes LS, Agrawal SK, Atlas J. Diagnosis and management of benign paroxysmal positional vertigo (BPPV). CMAJ 2003; 169(07): 681-693. [ Özet ]
3) Lopez-Escamez JA, Gamiz MJ, Fernandez-Perez A, Gomez-Fiñana M. Long-term outcome and health-related quality of life in benign paroxysmal positional vertigo. Eur Arch Otorhinolaryngol. 2005; 262: 507-511. [ Özet ]
4) Oron Y, Cohen-Atsmoni S, Len A, Roth Y. Treatment of horizontal canal BPPV: Pathophysiology, available maneuvers, and recommended treatment. Laryngoscope. 2015; 125(8): 1959-1964. [ Özet ]
5) Seok JI, Lee HM, Yoo JH, Lee DK. Residual Dizziness after Successful Repositioning Treatment in Patients with Benign Paroxysmal Positional Vertigo. J Clin Neurol. 2008; 4(3): 107-110. [ Özet ]
6) Jeong J, Eo TS, Oh J, Shin HA, Chung HJ, Choi HS. Monthly and seasonal variations in benign paroxysmal positional vertigo. J Vestib Res. 2021; 31(2): 101-107. [ Özet ]
7) Maia FCZE, de Fraga RB, Ramos BF, Cal RV, Albernaz PLM. Seasonality and solar radiation variation level in benign paroxysmal positional vertigo. Acta Otolaryngol. 2019; 139(6): 497-499. [ Özet ]
8) Koparal M, Altuntaş EE, Yılmazer C, Altunışık E, Karataş M. Effects of the Lunar Cycle, Seasons and the Meteorological Factors on Peripheral Vertigo. Turk Arch Otorhinolaryngol. 2022; 60(3): 149-154. [ Özet ]
9) Seidel DU, Park JJH, Sesterhenn AM, Kostev K. Demographic data and seasonal variation in peripheral vestibular disorders in ENT practices in Germany. J Vestib Res. 2019; 29(4):181-190. [ Özet ]
10) Ozturk MZ, Cetinkaya G, Aydin S. Climate Types of Turkey According to Köppen-Geiger Climate Classification. Köppen-Geiger İklim Sınıflandırmasına Göre Türkiye'nin İklim Tipleri. Journ Geography. 2017, 35: 17-27.
11) Adegbiji WA, Olajide TG, Olubi O, Olajuyin OA, Aluko AA. Clinicoepidemiology of benign paroxysmal positional vertigo in Nigerian. J Family Med Prim Care. 2019; 8(10): 3220-3224. [ Özet ]
12) Von Brevern M, Radtke A, Lezius F, Feldmann M, Ziese T, Lempert T, Neuhauser H. Epidemiology of benign paroxysmal positional vertigo: a population based study. J Neurol Neurosurg Psychiatry. 2006; 78(7), 710-715. [ Özet ]
13) Meghji S, Murphy D, Nunney I, Phillips JS. The Seasonal Variation of Benign Paroxysmal Positional Vertigo. Otol Neurotol. 2017; 38(9): 1315-1318. [ Özet ]
14) Luryi AL, Lawrence J, Bojrab DI, LaRouere M, Babu S, Zappia J, Sargent EW, Chan E, Naumann I, Hong RS, Schutt CA. Recurrence in Benign Paroxysmal Positional Vertigo: A Large, Single-Institution Study. Otol Neurotol. 2018;39(5):622-627. [ Özet ]
15) Yu S, Liu F, Cheng Z, et al. Association between osteoporosis and benign paroxysmal positional vertigo: a systematic review. BMC Neurol 2014;14:110. [ Özet ]
16) Oh SR, Min SJ, Kim CE, Chang M, Mun SK. The effects of climate on the incidence of benign paroxysmal positional vertigo. Int J Biometeorol. 2020; 64(12):2119-2125. [ Özet ]
17) Celebisoy N, Polat F, Akyurekli O. Clinical Features of Benign Paroxysmal Positional Vertigo in Western Turkey. Eur Neurol. 2008; 59(6): 315-319. [ Özet ]
18) Vaduva C, Estéban-Sánchez J, Sanz-Fernández R, Martín-Sanz E. Prevalence and management of post-BPPV residual symptoms. Eur Arch Otorhinolaryngol. 2018; 275(6): 1429-1437. [ Özet ]




