THE EFFECT OF THE ADENOID HYPERTROPHY RATE ON UPPER AIRWAY OBSTRUCTION SYMPTOMS
2Antalya Eğitim ve Araştırma Hastanesi, KBB, Antalya, Türkiye
Summary
Objectives: Adenoid hypertrophy causes upper airway obstruction symptoms. Main target of adenoidectomy is to overcome nasal obstruction. However adenoid hypertrophy is also related with sleep problems and nasal discharge. In this study our aim was to determine the relation and correlation between the size of adenoid tissue and symptoms of upper airway obstruction.Patients and Method: Patients who had adenoidectomy operation in university hospital were called for a follow-up control. The pre- and post-operative adenoid size of patients was determined endoscopically and these values were compared with symptoms of nasal obstruction, fatigue during exercise, mouth breathing during sleep, snoring and nasal discharge that evaluated with visual analog scale.
Results: A considerably high correlation was found between the adenoid size and the total symptom scores. Question-based evaluation did not reveal a significant correlation between the adenoid size and nasal discharge.
Conclusion: Size of adenoid tissue has high effect on symptoms of nasal obstruction and sleep disorder. In studies which polysomnography are used for evaluating the success of adeno-tonsillectomy operations; nasal endoscopy should be performed to search for any residual or recurrent adenoid tissue before polysomnography.
Introduction
The pharyngeal tonsil, which is referred to as adenoids in routine ENT practice, is a portion of the lymphatic Waldeyer's Ring located on the posterior wall of the nasopharynx, protruding upwards. It is in close relation with the choanae and ostium of the Eustachian tube. Adenoid hypertrophy may cause nasal obstruction, mouth breathing during sleep, snoring, anterior and posterior nasal discharge, cough, speech disturbances, behavioral disturbances, lethargy and oro-facial development disorders [1].Adenoidectomy, either alone or in combination with tonsillectomy, is one of the most common operations indicated by ENT specialists and is among the most frequent operations performed in the last century. In various trials, 70–100% improvement rates have been reported in the quality of life parameters of patients [2]. In a small percentage of patients, symptoms may persist after surgery. On the other hand, it was reported that in 98% of children with adenotonsillar hypertrophy, respiratory disturbance associated with sleep was not observed [3]. This finding indicates that the relation between adenotonsillar hypertrophy and sleep apnea is not clearly understood yet.
In general, the effects of adeno-tonsillectomy on the upper respiratory tract are evaluated either by polysomnography or by evaluating the symptoms using scales for quality of life [3,4,5]. However, in these trials, residual or recurrent adenoid tissue was not investigated prior to performing post-operative polysomnography or before completion of the quality of life scales. In this trial, our aim was to investigate the effect of pre- and post-adeno-tonsillectomy adenoid tissue size on symptoms of upper respiratory tract.
Methods
Thirty-six patients who had undergone adenoidectomy, adeno-tonsillectomy and adeno-tonsillectomy with tube insertion were enrolled in this trial. The patients who were older than 15 years, patients who had systemic or chest disease and the patients whose parents are unable to complete visual analog scale were excluded from the study. Most of the surgical interventions were performed by ENT residents using the curettage technique, under the supervision of the related specialist. In a limited number of patients, the operation was performed by a senior ENT specialist using curettage technique. All the patients were called for post-operative follow-up visit. The protocol was approved by the Ethics Committee of **** University. The parents of patients were informed about the study and informed consents were obtained. The patients were requested to enter their status of complaints on a scale, which covered five symptoms and classified the symptom severity from 1 to 5. When the patient's age was not suitable for completion of this scale, the parents were asked to fill in. The symptoms indicated in the scale were as follows: Symptom 1: nasal obstruction, symptom 2: fatigue during exercise, symptom 3: mouth breathing during sleep, symptom 4: snoring and symptom 5: nasal discharge. The degree of symptom severity was rated between 0 and 4. Explanations for these ratings are as follows: ‘0' no complaint, ‘1' very mild, ‘2' moderate, ‘3' poor, and ‘4' severe. The sum of scores for 5 symptoms generated a total symptom score (TSS) for each patient.Following the general ENT examination, 0.025% oxymetazoline (Santa Farma, Turkiye) solution was instilled in each nostril and topical anesthesia was provided by 10% lidocaine (Astra Zeneca, UK). Using zero degree 2.7mm rigid endoscopes (Karl Storz, Germany), diagnostic nasal endoscopy was performed and the adenoid nasopharynx rate was described by 10% increases, based on guidelines previously described by Buchinsky et al. [6]. Cases, which displayed no adenoid mass or with an adenoid tissue of lower than 10%, were considered as 0%.
Statistical Method
Correlations of variables with normal distribution were analyzed using the Pearson correlation coefficient and correlation of remaining variables was analyzed using the Spearman rho correlation coefficient. With regard to certain variables, differences between the means of recurrent and non-recurrent groups were also evaluated and the Student's t test was used for this purpose. A p value of <0.05 was accepted as statistically significant. The SPSS 17.0 statistical package program was used in the analysis of the data set (Statistical Package for the Social Sciences, version 17.0, SSPS Inc, Chicago, IL, USA).
Results
The age ranges of cases before the operation were 3-15 (mean 8.9), and that for after surgery was 6-18 (mean 11.58); 17 of the 36 cases were female and 19 were male. Adenoidectomy was performed in 7 patients, adeno-tonsillectomy in 24 cases, and adeno-tonsillectomy + tube insertion in 5 patients. Considering the fact that tonsillectomy itself may also affect the symptom scores, the statistical evaluations were performed for all the patients with adenotonsillectomy and separately for sole adenoidectomy patients. The mean postoperative follow up visit time was 2.7 years (range 1.5 years to 3.2 years) after operation.Before the surgical operation, the rate of adenoid hypertrophy obstructing the nasopharynx was 10-20% in 3 patients, 30-40% in 3 patients, 50-70% in 12 patients, and 80-100% in 18 patients. The surgical procedure of patients who had the adenoid hypertrophy rate lower than 50% was adeno-tonsillectomy or adeno-tonsillectomy with tube insertion. The adenoidectomy was performed due to the possible reservoir potential of adenoid tissue in these patients. After the operation, the rate of adenoid tissue obstructing the nasopharynx was determined as 0% in 15 patients, 10-20% in 11 patients, 30-40% in 6 patients, 50-70% in 3 patients, and 90% in 1 patient. (Fig.1)
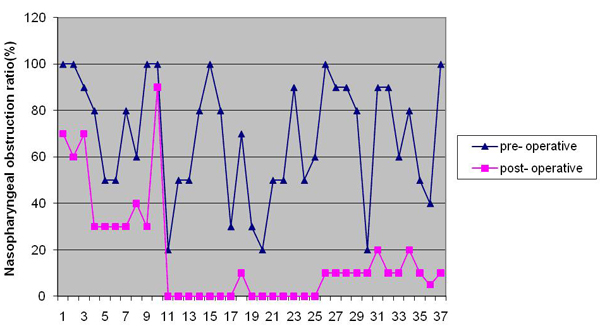 Büyütmek İçin Tıklayın |
Fig 1: Pre- and post-operative nasopharyngeal obstruction rates of patients |
The pre-operative minimum and maximum values of TSS in patients were 0 and 20 with a mean value of 11.2, and the respective values after the operation were 0 and 10 with a mean value of 1.8. (Fig.2) The pre- and post-operative adenoid rates and TSS value scores have been presented in Table 1 and Table 2.
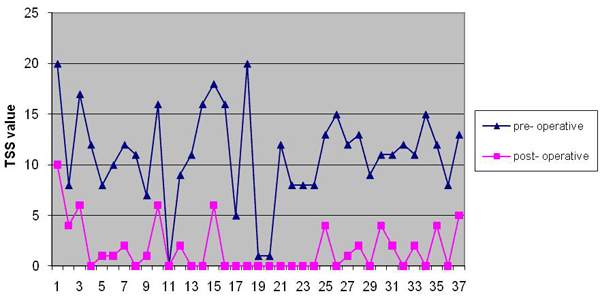 Büyütmek İçin Tıklayın |
Fig 2: Pre- and post-operative TSS values |
Table 1: Distribution of TSS values according to pre-operative adenoid rates
Table 2: Distribution of TSS values according to post-operative adenoid obstruction rates
Positive direct correlations of 55% and 47% were found between the pre-operative TSS values and the pre-operative nasopharyngeal obstruction rates and also between the post-operative TSS values and the post-operative nasopharyngeal obstruction rates, respectively (p<0.01). Furthermore, a statistically significant correlation was determined between the post-operative decreases in TSS values and nasopharyngeal obstruction rates (p<0.01). (Fig.3)
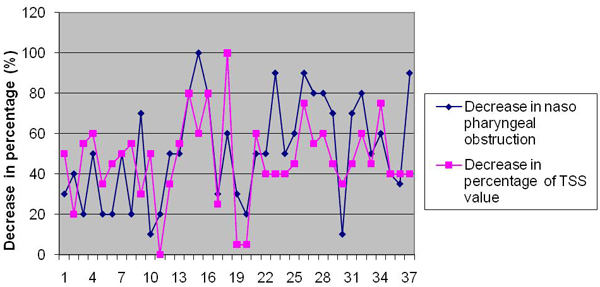 Büyütmek İçin Tıklayın |
Fig 3: Comparison of percentage of post-operative decrease in nasal obstruction and TSS values |
In the evaluation of symptom scores in terms of separate symptoms and comparison of the scores with post-operative decrease in adenoid obstruction rates, all the symptoms were found to be correlated with the change in the adenoid obstruction rate, except for the 5th symptom (p<0.01). The fifth symptom (nasal discharge) was found to be unaffected by the change in the nasopharyngeal obstruction rate.
Separate evaluation of sole adenoidectomy patients revealed a correlation between the change in post-operative TSS values and the change in nasopharyngeal obstruction rates (p<0,05). Similar to the findings stated above, evaluations based on separate symptoms revealed a correlation between the nasopharyngeal obstruction rates and symptoms 1, 3 and 4 (p<0,01); however, no correlation was found for the other symptoms.
Discussion
Adenotonsillectomy operations in children are the most efficient method in the treatment of chronic adenotonsillitis and obstructive sleep apnea [4]. Especially in cases where adenotonsillectomy is solely performed for sleep apnea, polysomnography seems to be the most appropriate test for the follow-up of operated children (American Thoracic Society) [3,5,7]. On the other hand, in some of these trials, it was suggested that there was no correlation between the post-operative apnea-hypopnea indexes, which were revealed by polysomnography and quality of life measurements, and the cause of this finding is not clear yet [5]. However, in these trials the presence of residual and/or recurrent adenoid tissue was not evaluated by endoscopy during patient examinations. In such studies the surgical operations were regarded as totally flawless.A residual or recurrent adenoid tissue after adeno-tonsillectomy operation may change the polysomnography results and that may cause misinterpretation, as success of adeno-tonsillectomy operation is low, although it is not the failure of operation, but it is a failure of surgeon. In our opinion, the status of adenoid mass should be evaluated by endoscopic examination before performing a polysomnography. In a trial conducted by Chien et al., a correlation was found between the pre-operative adenoid size and nasal obstruction, mouth breathing during sleep and snoring [8]. In our trial, we observed significant correlations between the adenoid size and these symptoms, both in the pre- and post-operative periods. Unlike the tonsillar tissues that were fully extracted by direct visualization, adenoid tissues cannot be extracted under direct visualization. Therefore it was not possible to detect whether there was any adenoid tissue left during surgery or a post-operative recurrence present, unless an endoscopic examination would have been performed in the post-operative stage. It may be suggested that the inconsistency between polysomnographic examination and the quality of life scales may be due to these residual or recurrent adenoid masses. In a trial conducted by Wang and Clement, a considerably high correlation was found between snoring and adenoid volume, and larger adenoids were detected by endoscopy in snoring children [9].
Tonsil hypertrophy can also has an impact on obstruction symptoms. Because of ethical limitations it is impossible to form a control patient group who had sole adenoidectomy even they have tonsil hypertrophy. So it is not possible to evaluate that what kind of change could happen in obstruction symptoms of patients who had tonsil hypertrophy after adenoidectomy without tonsillectomy. However our study showed that symptoms are highly correlated with adenoid size. If there is adenoid residue, snoring, mouth breathing and nasal obstruction symptoms persisted even the patients had tonsillectomy. Likewise, the patients who had only complete adenoidectomy did not show any obstruction symptoms even they did not have tonsillectomy. The postoperative evaluation time of adenoidectomies is also important. Early evaluation of symptoms can also cause misinterpreting of the results of the surgery. There could be hemorrhagic crusts, secretions and traumatic edema of surrounding tissues that may cause worse symptom scores in early postoperative follow up. Additionally it may be early to evaluate recurrence symptoms. In a recent study Ezzat showed that mean duration until appearance of recurrence symptoms was 6.2 months [10]. Our follow up period is long enough to prevent such misinterpretation.
Nasal discharge is a sinonasal symptom, which is mainly related to rhinosinusitis. Ramadan and Tiu found that rhinosinusitis improved in 50% of patients following adenoidectomy, while no improvement was observed in 50% of the cases; they suggested that endoscopic sinus surgery is mandatory in these children [11]. In trials, adenoid tissue was blamed as the source of bacteria, which cause rhinosinusisits in children [12]. In our trial, among the 14 patients in whom no adenoid tissue was determined in the post-operative follow-up, nasal discharge was present in only 1 patient (questionnaire nasal discharge score was 1 in that patient). In 2 of 9 patients with heavy nasal discharge (their questionnaire score were between 3 and 4), there was an adenoid mass at a size of 20% or less. No correlation was found between nasal discharge and the adenoid size. This finding once more emphasizes a well-known fact that adenoid tissue may act as a reservoir, causing nasal discharge, and the volume of reservoir (adenoid mass) is not related to the quantity of nasal discharge.
Cooperation problems may be encountered in children while performing nasal endoscopy for observation of adenoid tissue. In such cases, use of flexible endoscopes and provision of short acting benzodiazepines or hypnotics in addition to topical anesthesia while carefully observing the respiratory functions of the child, were recommended [8]. Lateral nasopharynx radiography, computerized tomography (BT) and magnetic resonance (MR) imaging techniques are used as alternatives to endoscopy. However, the high cost and cooperation issues in MRI imaging and similar problems in addition to the high radiation content of computerized tomography evaluation limits their use. In a trial performed by Wormald and Prescott, which compared endoscopic findings with lateral nasopharynx radiography findings, endoscopy was found to show better correlation with the adenoid size and symptoms compared to radiography [13]. Gürpınar et al. compared the tissue volume extracted during adenoidectomy by lateral radiographs and found a significant correlation, but suggested that adenoidectomy was indicated in cases where the obstruction in lateral nasopharynx radiograph was more than 85%, [14]. In our trial, we did not encounter any problems related to tolerance of endoscopic examination. With explaining the procedure to children before intervention and provision of a suitable topical anesthesia, the use of pediatric endoscope with a diameter of 2,7 mm was well tolerated by children.
Another cooperation problem about children is difficulty in obtaining symptom scores. Parents can be asked to fill symptom scale to overcome this problem in children. However parents cannot answer questions like ‘fatigue during exercise' in an exact objectiveness and it reduces the reliability of the studies. It can be accepted as a weakness of our study.
In conclusion, upon considering high correlation with upper respiratory tract obstruction, nasal endoscopy seems to be the most efficient method in pre-operative evaluation and post-operative follow-up of patients in whom adenoidectomy is required. Especially during evaluation of the efficacy of adenoidectomies with polysomnography, it is essential to investigate presence of any residual or recurrent adenoid tissue.
Reference
1) Saxby AJ, Chappel CA. Residual adenoid tissue post-curettage: role of nasopharyngoscopy in adenoidectomy. ANZ J Surg. 2009;79:809-11. [ Özet ]
2) Joshua B, Bahar G, Sulkes J, Shpitzer T, Raveh E. Adenoidectomy: long-term follow-up. Otolaryngol Head Neck Surg. 2006;135:576-80. [ Özet ]
3) Zhang XW, Li Y, Zhou F, Guo CK, Huang ZT. Comparison of polygraphic parameters in children with adenotonsillar hypertrophy with vs without obstructive sleep apnea. Arch Otolaryngol Head Neck Surg. 2007;133:122-6. [ Özet ]
4) Nieminen P, Tolonen U, Löppönen H. Snoring and obstructive sleep apnea in children: a 6-month follow-up study. Arch Otolaryngol Head Neck Surg. 2000;126:481-6. [ Özet ]
5) Mitchell RB. Adenotonsillectomy for obstructive sleep apnea in children: outcome evaluated by pre- and postoperative polysomnography. Laryngoscope. 2007;117:1844-54. [ Özet ]
6) Buchinsky FJ, Lowry MA, Isaacson G. Do adenoids regrow after excision? Otolaryngol Head Neck Surg 2000; 123:576-81. [ Özet ]
7) Standards and indications for cardiopulmonary sleep studies in children. American Thoracic Society. Am J Respir Crit Care Med. 1996;153:866-78. [ Özet ]
8) Chien CY, Chen AM, Hwang CF, Su CY. The clinical significance of adenoid-choanae area ratio in children with adenoid hypertrophy. Int J Pediatr Otorhinolaryngol. 2005; 69:235-9. [ Özet ]
9) Wang D, Clement P. Fiberscopic imaging of the pediatric nasopharynx. Diagn Ther Endosc. 1995;1:153-7. [ Özet ]
10) Ezzat WF. Role of endoscopic nasal examination in reduction of nasopharyngeal adenoid recurrence rates. Int J Pediatr Otorhinolaryngol. 2010;74:404-6. [ Özet ]
11) Ramadan HH, Tiu J. Failures of adenoidectomy for chronic rhinosinusitis in children: for whom and when do they fail? Laryngoscope. 2007;117:1080-3. [ Özet ]
12) Lee D, Rosenfeld RM. Adenoid bacteriology and sinonasal symptoms in children. Otolaryngol Head Neck Surg. 1997;116:301-7. [ Özet ]
13) Wormald PJ, Prescott CAJ. Adenoids: Comparison of radiological assessment methods with clinical and endoscopic findings The Journal of Laryngology and Otology 1992; 106: 342-34. [ Özet ]




