KIMURA'S DISEASE: A DIAGNOSTIC CHALLANGE
2Dr. Lütfi Kırdar Reserach and Training Hospital Department of Pathology, Istanbul, Turkey
Summary
Kimura's disease is a rare, chronic, benign disorder primarily seen in male Orientals during second and third decades of life. Many clinicians don't have enough knowladge about clinical presentation of this entity. Disease presents itself as a tumor like lesion with a predilection for the head and neck region often with parotid gland involvement and usually associate with lymphadenopathy, peripheral eosinophilia and markedly elevated serum IgE levels.The diagnosis of Kimura's disease is frequently based on the biopsy or excision of the involved node. Resection of the tumor mass, systemic and intralesional corticosteroids local irradiation are the three major therapeutic options. A 43 years old Turkish male who had been misdiagnosed was referred to our clinic for treatment of recurrent neck mass. In addition to pathological reevaluation of patients histologic speciemens, various blood work was done. Kimura's disease was discussed with treatment options.Introduction
Kimura's disease is a chronic benign disorder primarily seen in male Orientals during second and third decades of life.1 Disease presents itself as a tumor like lesion with a predilection for the head and neck region often with parotid gland involvement and usually associate with lymphadenopathy, peripheral eosinophilia and markedly elevated serum IgE levels. After the first described as ‘eosinophilic lymphogranuloma' by Kung et al.[1] in 1937, then disease was made known as Kimura's disease by Kimura et al.[1] in 1948. Disease usually affects the Orientals but there are isolated case reports from other parts of the world affecting other races[2,3,4]. Recognition of the clinical picture may allow clinicians to reduce the concern about the possibility of malignant disease and limit the number of laboratory tests.We report a case of Kimura's disease to drow attention to this disease as its presentation could easily confused with malignancy.
Case Presentation
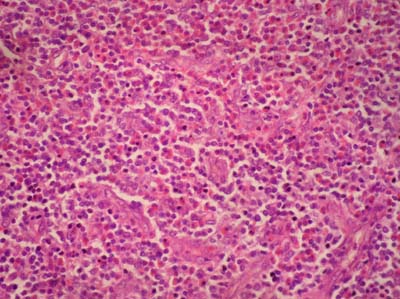
A 43 year old Turkish male was first seen, in 2000, with a painless diffuse superficial swelling in the left postauricular area. The swelling had grown gradually to the size of 3x2 cm since it had been first noted 1 year earlier. Ultrasonograpy showed solid round mass in postauricular region. Fine needle aspiration cytology (FNAC) was performed. The aspirate showed mature and transformed lymphocytes, hystiocytes, leucocytes, atypical cells with hyperchromatic nucleus. Then for accurate diagnosis, excisionel biopsy performed and histologic diagnosis made as sialoadenitis chronica. One month after the operation swelling recurred firstly on the insicion scar and rapidly growing tumor again developed at the left postauricular area. At this time tumor was enucleated by direct approach, the histologic diagnosis was at this time pseudolymphoma. Two years after last procedure, tumor recurred again. This time physical examination revealed 3x2 cm endurated mass overlying parotid gland and postauricular area in association with multiple lymph nodes measuring less than 1 cm that were palpaple anterior to the left sternocleidomastoid muscle. Facial nerve functions were intact. Ultrasonograpy and computed tomography showed solid mass with diffuse margins in left superficial parotid gland and periauriculer area. FNAC was inconclusive, complete tumor removal with left superficial parotidectomy was performed. At the time of surgery, dissection was difficult. Parotid tissue was noted as firm but without palpable tumor. Tumor was adherant to the skin and closely related to the facial nerve. The histology again showed sialoadenitis chronica and pseudolymhoma. The patient was consultated by our clinic, because of the discrepancy between the aggresive clinical course and previous benign diagnosis. We advised to reevaluate the last specimens. The specimens were reevaluated by a different pathology department. The diagnosis of Kimura's disease was made at last. This was based on picture of inflammatory cellular infiltrate in the interfollicular area consisting of lymphocytes, plasma cells, eosinophils and the lymphoid follicules with prominent germinal centers that surrounded by a fibrous tissue without impairment of follicular structure (Fig.1,2,3). Laboratory studies revealed peripheral eosinophlia of 28 per cent, and increased blood IgE concentration. The urinary protein was checked, there was no proteinuria. Patient was treated with 30 mg of prednisolon for 12 days then put on 8 mg prednisolone. He has been followed up in our clinic regularly. When the medication had been decreased, tumor recurred, dosage increased to 8 mg again, tumor resolved. At present patient show no recurrence (Fig. 4), the blood eosinophils and serum IgE are in normal levels .
 Büyütmek İçin Tıklayın |
Figure 1: İnterstitial fibrosis and lymphoid follicules which has prominent germinal centers (H+E×10). |
 Büyütmek İçin Tıklayın |
Figure 2: Perinodal eosinophil and plasma cell infiltration (H+E×100). |
 Büyütmek İçin Tıklayın |
Figure 3: Eosinophil and plasma cell infiltration, capillary proliferation(H+E×100). |
 Büyütmek İçin Tıklayın |
Figure 4-5: No recurrence 18 months after last surgery with contunious low dose steroid therapy. |
Discussion
Kimura's disease is a rare, benign chronic inflammatory disease which commonly occurs among the Oriental population. But there are isolated case reports from other parts of the world affecting other races.[2,3,4] The patients are usually in the second or third decade of life (reported mean age 27 to 40 ) with a male predominance (M:F=5/1).The typical physical manifestation of this disorder is slowly enlarging swelling with diffuse margins in the head and neck area, predominately in the preauricular or submandibular area. Rare cases have been reported to include tympanic membrane[2] and eye lids[3]. Lesions can occur in parts of the body other than in the head and neck ( axilla, groin, limb and trunk etc.).Viceral involvement is rare, in some cases there may be associated proteinuria with or without nephrotic syndrome, so urinary protein level should be checked in every patient. Renal involvement is the only frequent systemic manifestation, nephrotic syndrome has been reported in up to 60% of patients.[5] The onset is insidious, often long duration. Peripheral eosinophilia and elevated serum IgE levels almost always present.[5]
Kimura's disease can be confused clinically and histologically with angiolymphoid hyperplasia with eosinophilia (ALHE). Kimura's disease and ALHE was thougt to be same disease[1] but recent literature describes these as two distinct clinical entity.[3]
The diagnosis of Kimura's disease is often difficult. FNAC is a safe procedure, but has only limited value.[2] Pathologic diagnosis is frequently based on the biopsy or excision of the involved node. The characteristic histological features include preserved nodal architecture, florid follicular hyperplasia with reactive germinal centers, protein and IgE deposits in germinal centers, germinal center necrosis, eosinophilic infiltrates, proliferation of postcapillary venules, sclerosis, polykaryocytes of the Whartin-Finkeldey type, eosinophilic folliculolysis, and prominent eosinophilic microabscesses.[5,6]
The clincal differential diagnoses of Kimura's disease should include ALHE, reactive lymphadenopathy secondary to drug reaction and parasitic infections, lymphoma, parotid tumor with nodal metastasis, and Mikulicz disease.[5] A healing abscess can be differentiated by its content of large number of polymorphs and histiocytes. Appropriate cultures, histochemical stains, and immunophenotyping studies will help separate these unique and distinct lesions.
The pathophysiology of Kimura's disease is not understood at this time, may be related to a disturbance of an interaction between type 1 and 2 T helper cells (Th1 and Th2). Patients with Kimura's disease have been shown to have high levels of circulating eosinophilic cationic protein ( ECP ) and major basic protein ( MBP ) with heavy concentrations of IgE in their tissue.[6] Atopic reaction to a continuous antigenic stimulus ( specially candida albicans)[7], parasitic infection, neoplasm have been actively tought in the etiology for Kimura's disease but not defined. Perhaps continous antigenic stimulus causing IgE deposits along the glomerular capillary membrane causes epitheloid damage to renal glomeruli, results renal disease in Kimura's disease.[8] No evidence of antigenic stimulus was found in our case.
Three major management options exist for Kimura's disease. Resection of the tumor mass may be effective but lesions tends to recur.[5,7] At the time of surgery the affected tissue are discribed as poorly circumscribed, matted together, fibrous and vascular.[5] Systemic and intralesional corticosteroids have been shown to reduce the size of lesion, but the tumor tends to recur when these drugs are discontinued as exprienced in our case .[8] Long term steroid treatment may side affects that limit its use. Finally local irradiation has also been shown to be affective but generally not advocated in younger patients.[8] Indications for radiotherapy include patients who have failed with medical management. Sometimes, even with agressive treatment plan, complete remission is not possible.
These lesions are benign, malignant degeneration has never been observed.[4] It may be adviseble to take a conservative approach, treating only if the mass continues to grow or causes significant deformity[4]. Patients should be followed up for recurrance , proteinuria and for side effects of steroid treatment regularly.
Conclusion
In a view of presentation in the head and neck region with a mass or nodular lesion Kimura's disease should be in the differantial diagnosis. A routine protocol for treating recurrent and systemic Kimura's disease has not been accepted yet. Kimura's disease usually affects the Orientals and thus many clinicians and pathologists in the other parts of the world are unaware of this entity; it could easily misdiagnosed. Recognition of the clinical picture may allow practitioners to reduce the concern about the possibility of malignant disease and limit the number of laboratary tests.Reference
1) Armstrong WB, Allison G, Pena F, Kim JKV. Kimura's disease: Two case reports and a literature review. Ann Otol Rhinol Laryngol 1998;107: 1066-71. [ Özet ]
2) Nyrop M. Kimura's disease: case report and brief review of the litherature. J Laryngol Otol 1994; 108: 1005-1007. [ Özet ]
3) Kennedy SM, Pitts JF, Lee WR, Gibbons DC. Bilateral Kimura's disease of eyelids. Br J Ophthalmol 1992; 76: 755-757. [ Özet ]
4) Calli C, Oncel S, Pinar E, Bener S, Calli A. Kimura's disease: two case reports with a review of the literature. Kulak Burun Bogaz Ihtis Derg. 2004;12:139-143. [ Özet ]
5) Kuo T, Shih L, Chan H. Kimura's disease involvement of lymph nodes and distinction from angiolymphoid hyperplasia with eosinophilia. Am J Surg Path 1988; 12: 843-854. [ Özet ]
6) Motoi M, Wahid S, Horie Y, Akagi T. Kimura's disease; clinical, histological and immunohistochemical studies. Acta Med Okayama 1992; 46:449-455. [ Özet ]
7) Terada N, Konno A, Shirotori K, Fujisawa T, Atsuta J, Ichimi R, Kikuchi Y,Takaki S, Takatsu K, Togawa K. Mechanism of Eosinophilic granulation in the patients with subcutaneous angioblastic lymphoid hyperplasi with eosinophilia (Kimura's disease) Int Arch Allergy Immunol 1994;104: 18-20. [ Özet ]
8) Day TA, Abreo F, Hoajsoe DK, Aarstad RF. Treatment of Kimura's disease; a therapetic enigma. Otolaryngol Head Neck Surg. 1995; 112: 333-337. [ Özet ]




