ANALYSIS AND MANAGEMENT OF HOSPITALIZED PATIENTS WITH EPISTAXIS
Summary
Purpose: The etiology and comorbidity diseases of the epistaxis patients who were hospitalized and treated were evaluated and the management to the epistaxis patients was discussed in the light of the literature.Material and Methods: 68 patients with epistaxis admitted to our emergency department and hospitalized were examined retrospectively. Age, gender, comorbid diseases, methods of treatment, and duration of hospital stay were evaluated.
Results: 68 patients were included in our study (26 female (38.2%) and 32 male (61.8%)). The mean age of our patients was 54 ± 2.41. Hypertension (39.7%) was the most common cause of epistaxis in our study. The second most frequent cause was nasal inflammation (23.5%). Conservative treatments were performed to 50 of our patients and 18 of them underwent surgical treatment. The duration of hospital stay in our patients was found to be 1-11 days (2.77 ± 1.79).
Introduction
Epistaxis is one of the most common otolaryngologic emergencies. It is defined as bleeding caused by coagulation disorder or mucosal damage in the nasal cavity [1]. Although the prevalence of epistaxis is not exactly known, it is very common. It is estimated that only 6% of patients apply to health centers [1,2] as the majority of patients with epistaxis does not go to the health center and therefore not get registered since patients can stop their epistaxis by their own intervention. Epistaxis is a disease symptom and its severity is very variable. The majority of epistaxis can stop with simple pressure exerted by patients. Few patients have severe epistaxis and need advanced treatment methods. [1].Epistaxis has been reported to be more common in males than females. It is more common in dry and cold weather [1]. Epistaxis usually originates from the anterior region of the nose and is mild bleeding. Bleeding from the posterior region may occur, although it is rare [3]. The etiology of epistaxis varies with age and anatomical localization. In patients under the age of 35, the most common cause is trauma. In patients over 50 years of age, the most common cause of epistaxis is due to comorbid diseases (liver failure, hypertension, etc.) [4].
Epistaxis can be diagnosed and treated with a good anamnesis and nasal examination. In our study, the intervention approaches to epistaxis were explained and the patients who needed hospitalization were discussed in light of the literature.
Methods
In this study, 68 patients admitted to the state hospital otorhinolaryngology outpatient clinic and emergency department for epistaxis and required hospitalization were included. The files of patients with epistaxis between 2012-2019 were reviewed retrospectively.Patients who were treated in the emergency department by controlling their epistaxis, those hospitalized in other clinics, and patients under the age of 18 were not included in the study. The patients were divided into three groups as <50, 50-80, and ?80 years of age. Our patients were evaluated in terms of age, gender, comorbid diseases, etiologic factors, treatment, and hospitalization duration.
Results
Of the 68 patients included in our study, 26 were female (38.2%) and 32 were male (61.8%). The mean age of our patients was 54 ± 2.41. 12 of the patients included in current study were <50 years old, 28 were between 50-80 years old and 3 were ≥80 years old.Hypertension (39.7%) was the most common cause of epistaxis. The second most common cause was nasal inflammation (23.5%). The distribution of etiological factors of our patients divided into groups according to age is shown in Table 1. In our ≥50 year old patients, the most common cause was hypertension and in <50 year old group the most common cause was nasal inflammation. Five patients (3 Septorinoplasty, 2 septoplasty) included in our study had epistaxis between the 3rd and 20th days after nasal surgery. There were no comorbid diseases in 22 of our patients, 27 had hypertension, 14 had type 2 diabetes, 4 had chronic obstructive pulmonary disease (COPD), and 6 coronary artery disease.
Table 1: Distribution of Etiological Factors by Age Groups
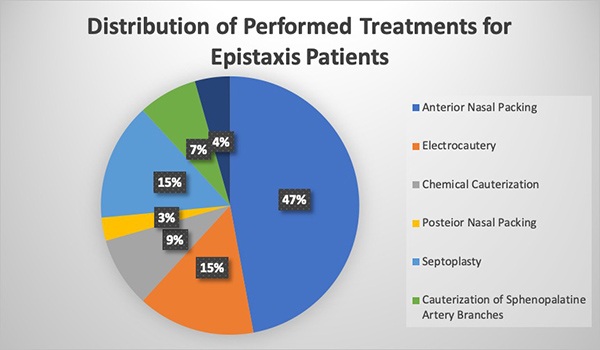
The duration of hospitalization of our patients was found to be 1-11 days (2.77 ± 1.79). Conservative treatments were performed in 50 (73.5%) of our patients and surgical treatment was performed in 18 (26.5%). As conservative treatment, the most common were anterior nasal packing (47.1%), electrocautery (14.7%), chemical cauterization (8.8%), and posterior nasal packing (2.9%). As a surgical procedure, 10 (14.7%) patients with septal deviation had septoplasty, 5 (7.4%) patients had endoscopic cauterization of sphenopalatine artery branches, and 3 (4.4%) patient had sphenopalatine artery ligation (Figure 1).
 Büyütmek İçin Tıklayın |
Figure 1: Distribution of Performed Treatments for Epistaxis Patients |
Discussion
Epistaxis is one of the most common emergencies in the ENT department. Very few patients need to go to a physician for epistaxis and a very small proportion of them are hospitalized. The majority of epistaxis originates from the anterior part of the nose, and the severity of this epistaxis is low. Therefore, epistaxis caused by the anterior part of the nose can be easily stopped with small interventions [1,5].It has been reported in the literature that few of the patients with epistaxis presented to the hospital. Only 10% of these patients consult a physician for epistaxis and only 2% of them require surgical treatment [6,7]. In our study, our surgical procedure rate was 26.5%. The reason for this is that the number of patients consists of fewer people than studies in the literature. In addition, only hospitalized patients were included in our study and we think these were the reasons for the higher surgical treatment rate.
Epistaxis has been reported to be more common in male and the elderly [8,9]. In a study conducted by Pollice et al., 70% of patients with epistaxis were found to be 50 years and older [5]. In our study, as reported in the literature, epistaxis was more frequent in males and elderly patients.
There are three different groups in the etiology of epistaxis; local, systemic and environmental factors. It is known that the frequency of epistaxis increases in regions where winter is cold, and summer is dry [8,10]. The most common local cause is trauma and often occurs after digital trauma and accidents [1,2]. Other local causes include septal pathologies (septal perforation, septal deviation, etc.), tumors (inverted papilloma, etc.) and aneurysms. The most common group of systemic diseases is blood coagulation disorders (thrombocytopenia, von Willebrand disease, hereditary hemorrhagic telangiectasia, etc.). In addition, hormonal causes (endometriosis, pregnancy, etc.) and cardiac pathologies can be considered as systemic diseases that may cause epistaxis [11]. Neto et al. found a relationship between hypertension, ventricular hypertrophy, and epistaxis, indicating that long-term hypertension may be the cause of epistaxis [12]. In our study, the most common cause of epistaxis was hypertension, followed by septal perforation and nasal inflammation, respectively.
Dabrowska-Bien et al. In the study, in which 5639 patients were included, the frequency of axial and epistaxis after the nasal surgery was observed (3.3%). In our study, it was observed that nasal inflammation was the most common cause of epistaxis in patients <50 years of age group. Nasal inflammation causes damage to the nasal mucosa, moreover, nasal inflammation is very common in patients <50 years of age due to the low rate of comorbid diseases and nasal inflammation is the most common cause [13,14].
Epistaxis originates from the anterior and / or posterior anatomical regions of the nose [14]. Anterior epistaxis occurs in young and children, and posterior hemorrhage occurs mostly in the elderly people. Anterior epistaxis is usually caused by the Kisselbach plexus located in the anterior of the septum, while posterior hemorrhages are caused by the Woodruff plexus formed by the branches of the sphenopalatine artery [5]. In all age groups, 82% of epistaxis occurs as anterior epistaxis and can be treated with conservative and local methods [15].
Epistaxis treatment varies according to the underlying cause. Generally, anterior bleeding can be stopped easily. Treatment in epistaxis varies according to the underlying cause, so treatment can be very complex. Epistaxis treatment is divided into two as conservative and surgical treatments. In the literature, epistaxis treatment is mostly used for conservative treatment because it is easier to apply and less postoperative complications. Huang et al. found that the patients treated with conservative methods had less hospitalization time and the complications were shorter [16]. In our study, 73.5% of the patients underwent conservative treatment and 18 patients required surgical treatment.
Although the vast majority of patients have anterior epistaxis, some of them may be of posterior origin. In such cases patients may need posterior nasal packing which can be 70% effective when applied by trained physicians, although it is not as successful as endoscopic or surgical treatment. There is a risk of pain and aspiration of posterior nasal packing and therefore it should be performed by experienced physicians [17]. In our study, two patients needed posterior nasal packing and it was performed effectively without the need for surgical treatment.
Follow-up and treatment of comorbid diseases were planned in one patient who was hospitalized for epistaxis. This patient had intermittent epistaxis and anticoagulant (acetylsalicylic acid) treatment had to be discontinued after consultations. Intravenous tranexamic acid treatment was given since general anesthesia could not be performed due to comorbid diseases. Joseph et al. in their review in 2018 observed that tranexamic acid was effective in patients and moderate-quality evidence was found [18].
Massive or fatal hemorrhage appears to be very rare in patients with epistaxis [19,20]. Approximately 10% of patients with epistaxis require posterior tampon or further procedures. If bleeding cannot be controlled, the patients should be referred to advanced centers [11,21].
The duration of hospitalization is variable in patients with epistaxis. Pollice et al. found this period as 4 days [5], Vaamonde et al. as 9.2 days [22]. In our study, the mean duration of hospital stay was 2.77 ± 1.79 days.
It should be remembered that epistaxis is a symptom. Possible complications of patients should be taken into consideration, especially elderly and comorbid patients should be hospitalized, and appropriate consultations should be requested and treated.
Reference
1) Shaw CB, Wax MK, Wetmore SJ. Epistaxis: a comparison of treatment. Otolaryngol Head Neck Surg 1993;109:60-65. [ Özet ]
2) Alvi A, Joyner-Triplett N. Acute epistaxis. How to spot the source and stop the flow. Postgrad Med 1996;99:83-90, 94-96. [ Özet ]
3) Schaitkin B, Strauss M, Houck JR. Epistaxis: medical versus surgical therapy: a comparison of efficacy, complications, and economic considerations. Laryngoscope 1987;97:1392-1396. [ Özet ]
4) Pallin DJ, Chng YM, McKay MP, Emond JA, Pelletier AJ, Camargo CA Jr. Epidemiology of epistaxis in US emergency departments, 1992 to 2001. Ann Emerg Med 2005;46:77-81. [ Özet ]
5) Pollice PA, Yoder MG. Epistaxis: a retrospective review of hospitalized patients. Otolaryngol Head Neck Surg 1997;117:49-53. [ Özet ]
6) Ram B, White PS, Saleh HA, Odutoye T, Cain A. Endoscopic endonasal ligation of the sphenopalatine artery. Rhinology 2000;38:147-149. [ Özet ]
7) Kitamura T, Takenaka Y, Takeda K, et al. Sphenopalatine artery surgery for refractory idiopathic epistaxis: Systematic review and meta-analysis. Laryngoscope 2019;129:1731-1736. [ Özet ]
8) Juselius H. Epistaxis. A clinical study of 1,724 patients. J Laryngol Otol 1974;88:317-327. [ Özet ]
9) Iqbal IZ, Jones GH, Dawe N, et al. Intranasal packs and haemostatic agents for the management of adult epistaxis: systematic review. J Laryngol Otol 2017;131:1065-1092. [ Özet ]
10) Tan LK, Calhoun KH. Epistaxis. Med Clin North Am 1999;83:43-56. [ Özet ]
11) Rudmik L, Smith TL. Management of intractable spontaneous epistaxis. Am J Rhinol Allergy 2012;26:55-60. [ Özet ]
12) Lubianca Neto JF, Fuchs FD, Facco SR, Gus M, Fasolo L, Mafessoni R, Gleissner AL. Is Epistaxis Evidence of End-Organ Damage in Patients With Hypertension?. Laryngoscope 1999;109:1111-1115. [ Özet ]
13) Dabrowska-Bien J, Skarzynski PH, Gwizdalska Lazecka K, Skarzynski H. Complications in septoplasty based on a large group of 5639 patients. Eur Arch Otorhinolaryngol. 2018;275:1789-1794. [ Özet ]
14) Jackson KR, Jackson RT. Factors associated with active, refractory epistaxis. Arch Otolaryngol Head Neck Surg 1988;114:862-865. [ Özet ]
15) Kaygusuz İ, Karlıdağ T, Keleş E, et al. Hastaneye Yatırılarak Tedavi Edilen 68 Epistaksisli Hastanın Retrospektif Analizi. Fırat Tıp Dergisi 2004;9:082-5. (Corpus ID: 70744131)
16) Huang CL, Shu CH. Epistaxis: a review of hospitalized patients. Zhonghua Yi Xue Za Zhi (Taipei) 2002;65:74-78. [ Özet ]
17) Schlosser RJ. Clinical practice. Epistaxis. N Engl J Med 2009;360:784-789. [ Özet ]
18) Joseph J, Martinez-Devesa P, Bellorini J, Burton MJ. Tranexamic acid for patients with nasal haemorrhage (epistaxis). Cochrane Database Syst Rev. 2018;31;12:CD004328. [ Özet ]
19) Manes RP. Evaluating and managing the patient with nosebleeds. Med Clin North Am 2010;94:903-912. [ Özet ]
20) Marin E, Watelet JB, Gevaert P, Van Zele T. Severe spontaneous epistaxis: retrospective study in a tertiary ENT centre. Eur Arch Otorhinolaryngol 2019;276:1693-1699. [ Özet ]
21) Petruson B, Rudin R. The frequency of epistaxis in a male population sample. Rhinology 1975;13:129-33. [ Özet ]
22) Vaamonde Lago P, Lechuga García MR, Mínguez Beltrán I, Frade González C, Soto Varela A, Bartual Magro J, Labella Caballero T. [Epistaxis: prospective study on emergency care at the hospital level]. Acta Otorrinolaringol Esp 2000;51:697-702. [ Özet ]




