MALIGN CERVICAL LYMPHADENOPATHY. WHOM AND WHERE?
2Sanko Üniversitesi, Kulak Burun Boğaz Hastalıkları, Gaziantep, Turkey
Summary
Introduction: Identification of specific characteristics of enlarged cervical lymph nodes could help the clinician for referring to surgical intervention in the diagnosis algorithm. The main purpose of this research is to identify any possible relation between the malignancy and the risk factors at the cervical lymphadenopathy.Material and Methods: Several factors such age, gender, lymph node size, anatomic location of lymph node was evaluated according to histopathology findings of the paediatric and adult patients between November 2014 and May 2019.
Results: The sizes of lymph nodes, anatomical location (supraclavicular region), adult age, male gender (adults) were the factors that found to be related to malignancy with a statistical significance. While the paediatric hypertrophic lymph node size was 1.5 cm and the adult lymph node size was 1.2 cm, the specificity rate for malignancy was 90% according to the biopsy results.
Conclusion: The malignancy risk for a cervical lymph node may become higher at adult male patients and supraclavicular located ones. Apart from age and gender, we are in the opinion that the risk of malignancy increased by the enlargement of the size of cervical lymph nodes.
Introduction
There are approximately three hundred lymph nodes in the head and neck region (HNR). None of these lymph nodes should be palpable during the routine HNR examination.[1] If any lymph node noted over 1cm length during the examination of HNR; is called Cervical Lymphadenopathy (CL).[2] CL is one of the common cause of neck lumps in childhood and adults. Majority of CL results from the local or generalized infectious conditions. Autoimmune diseases and malignancies could also cause CL.[3]Despite the lower rates (4, 69%), the main fear for the clinician about CL is to be unaware of the malignancy.[4] To maintain an accurate differential diagnosis; taking a detailed history and performing physical examination is essential in the initial approach. A biochemical marker that allows us to make a definite diagnosis of malignancy without tissue sampling has not been identified yet.[5,6] However, some locations like Virchow's node are more suspicious for the malignancy. Virchow's node is a cervical lymph node which locates in the left supraclavicular fossa.[7] It is highly associated with the metastasis of abdominal located carcinomas. Presence of a Virchow's node is related to the low survey [8]. Only invasive procedures are needed for the proper diagnosis of malignant CL.[9]
In the previous decades, it was believed that the role of surgery in the diagnosis of CL will be decreased with the contemporary non-invasive methods such as imaging or novel biochemical markers.[10] However, the gold standard for diagnosis of the CL remains lymph node biopsy.[11] So one of the main question for the CL is '' which patient is an accurate candidate for lymph node biopsy according to the physical findings?" The main purpose of this article is to evaluate the main characteristic patterns of the cervical lymph nodes at the patients with malignancy in a retrospective design.
Methods
The diagnosis of cervical lymph node biopsies between November 2014 and May 2019 at the Gaziantep University was collected from the hospital database system. Additionally, age, gender, imaging modalities (ultrasonography, computerized tomography's and magnetic resonance images) and the physical examination data were also withdrawn from the database system. The location, the length and the side of the cervical lymph nodes were especially scanned in the data of physical examinations.Two groups were created according to age. Patients under eighteen years old create the paediatric age group and over eighteen years old created the adult group. All the patient's physical examination records were checked for head and neck examinations, endoscopic nasopharynx and laryngopharynx examinations. The medical records of these patients for infectious aetiologies were also checked such complete blood count (CBC), erythrocyte sedimentation rate, C reactive protein levels. Additionally, serological laboratory findings for the most common infectious agents that could cause CL (Cytomegalovirus (CMV), Epstein Barr Virus) were also checked. In our clinic, infectious caused CL patients were re-examined four weeks after the medical therapy and neck ultrasonography's were performed. After the one-month follow-up period, if the longest diameter of CL was found over 1, 5 cm; fine-needle aspiration (FNA) of CL was decided in adults and cooperated children. Afterwards, if the FNA results are non-diagnostic CL biopsy decision was made.
Surgical approaches were performed under general anaesthesia by the head and neck surgeons. During the operation, the most evident lymph node was excised if there were conglomerate lymph nodes. The size of the lymph nodes in this study was collected from the ultrasonographic data.
Location of lymph nodes was categorised as follows; the submandibular and submental lymph nodes were Level I, upper jugular lymph nodes were Level II, Middle jugular lymph nodes were Level III, lower jugular lymph nodes were Level IV and posterior triangle group was Level V. Additionally, the supraclavicular lymph nodes considered as levelVB. The supraclavicular region pathologies were classified under Level V cervical lymph nodes which also covers Level VB. . Except, the Virchow lymph node was belonging to Level IV.
If there is any lack of information in the patient data such as demographics, physical examination, head and neck ultrasonography or pathology result; the patient is excluded from the study.
Statistical tests were performed by using SPSS version 18 software (SPSS Inc, IBM Chicago, IL, USA). For numeric variables, student T-test for independent samples was achieved. Chi-square test was executed for categorical variables. After performing regression analysis ROC curves were drawn.
Results
This retrospective study includes the evaluation of two hundred eighty-three patient's cervical lymph node biopsy results and the clinical findings. There were sixty-two patients at the paediatric group and two hundred and twenty-one patients at the adult group. The age, gender of the patients and the locations and the size of the lymph nodes are displayed in Table 1.Table 1: The characteristic features of paediatric and adult groups
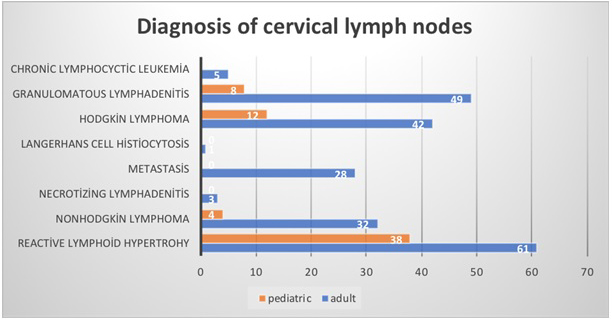
Addition to table 1, the age group was ranged between one-year-old and seventeen years old in the paediatric group and between eighteen years old and eighty years old in the adult group. The calculated long diameter of the lymph nodes was found between one cm and seven cm. According to histopathology results; one hundred twenty-two of the two hundred eighty-one lymph nodes were diagnosed with a malignancy-associated clinical situation. The histopathology results of the whole lymph nodes are shown in Figure 1.
 Büyütmek İçin Tıklayın |
Figure 1: Histopathological results of lymph node biopsy |
According to histopathological findings; there wasn't any benign lymph node found in the supraclavicular region. Five malignant lymph nodes of Level IV were Virchow lymph nodes and all of them was found metastasis of gastrointestinal malignancies (Adeno Ca) Forty-nine lymph node were diagnosed malignant in Level V and fifteen of them were excised from the supraclavicular region. The histopathological findings of the supraclavicular lymph nodes in the Level V section were identified as follows; Five lung squamous cell ca metastasis, four breast ca metastasis, three gastrointestinal adeno ca (stomach ca), two malignant melanoma metastasis and one unknown primary tumour metastasis, respectively. The ratio of benign and malignant lymph nodes to each other and percentages of total lymph nodes is displayed in Table 2.
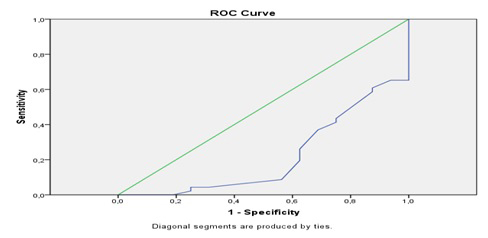
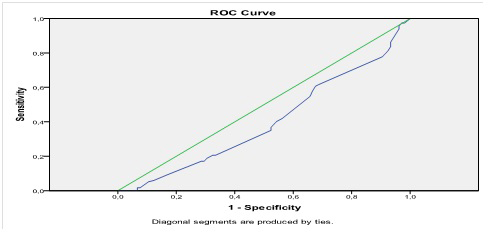
Multiple variable regression analysis was performed for age, gender, lymph node size and the side of the lymph node in both groups. These data are shown in Table 3 with p-value, odds ratio and the 95% confidential intervals. The age, gender and the size of the lymph node were found to be statistical significance after the multiple variable regressions. ROC curves were drawn according to the size of the lymph nodes. ROC curve of the paediatric group is shown in Figure 2 and the ROC curve of the adult group is shown in Figure 3. According to these curves for the lymph node biopsies; if a lymph node is over 1, 5 cm in the paediatric group the sensitivity for malignancy is 90% and if the lymph node is over 5 cm the specificity for malignancy is 90%. With similar methods, the adult group data stated that the lymph nodes over 1, 2 show 90% sensitivity for malignancy and lymph nodes over 3, 5 cm is found to be 90% specificity for the malignancy.
Table 3: Multiple Regression Analysis of the groups
 Büyütmek İçin Tıklayın |
Figure 2: ROC curve of paediatric cervical lymph nodes. Area under curve 0,504 |
 Büyütmek İçin Tıklayın |
Figure 3: Adult cervical lymph node ROC curve. Are under curve 0,568 |
Discussion
Identification of any palpable neck lymph nodes bothers the clinician especially when there is an enlargement identified between two examinations. The majority of CL's disappears within time without needing any further medical evaluation.[11] Tissue sampling for histopathology diagnosis of CL is recommended for the lymph nodes with a noted enlargement or which do not exhibit any decreased change in size in four weeks.[12] Lymph node biopsy is accepted as the gold standard for the accurate diagnosis of CL when compared with the other invasive procedures.[13] So the main question is "Which lymph node characteristic features are more representing a priority for the lymph node biopsy in addition to size and time?" In this article, we search answer for this question by the retrospective evaluation of malignant CL.First, we evaluated the lymph node size measured in the first examination. Previous reports concluded that CL length more than two cm in children and more than one cm in the adult group could be related to malignancy.[12,14] Our findings agreed with these reports. Similarly, we found that the size of CL over 1, 5 cm length in the paediatric group and over 1, 2 cm length in the adult group is related with malignancy with the sensitivity of ninety percentages.
Another point is male gender in the adult population could show an elevated risk for the malignancy at CL.[15,16]
The location of CL is the third variable that we found a correlation about the malignancy. Our findings revealed a higher ratio of malignancy diagnosed lymph nodes were found in the lower cervical levels than the upper levels. Additionally, malignant lymph nodes of level V constitute 17% of the total excised lymph nodes. A trend for the higher lymph node percentage in the lower cervical levels is seen except level III and IV. However, despite having a higher ratio of malignancy in their own single level, these two levels include a lower number of lymph nodes when compared to total lymph nodes. Previous reports state that there are much higher malignancy diagnosis levels at the supraclavicular region CL than the other locations.[14,17,18] Moreover, if a lymph node in the supraclavicular region is solid, fixed with an irregular border, some author is stated that "do immediate biopsy without waiting.[14,19,20,21] We agree with this statement as our results indicate that five left supraclavicular lymph nodes diagnosed with gastrointestinal ca metastasis. Additionally, lower cervical lymph node levels (supraclavicular regions) are more prone to the metastasis of lung, breast or gastrointestinal carcinomas.[22] According to our findings, metastatic lymph nodes were only found at Level IV and Level V. When we separate metastatic lymph nodes, the ratio of other malignancies in cervical lymph nodes distributed more homogeneously.
In addition to these characteristic features, the majority of those malignant lymph nodes diagnosed Hodgkin lymphoma in the paediatric age group. This finding also agreed with the literature.[17,23] In this study; despite the lower rates of lymphoma when compared to the paediatric group, the number of lymphoma patients was higher in the adult group. This difference in the ratios related to the other aetiologies of malignancy such solid organ tumours and their neck metastasis.[12]
The limitation of this study was; we were not able to assess the B symptoms (fever, weight loss, night sweating) due to the retrospective design of this study. Another limitation could be if there was any difference between the two radiologists for assessing the same lesion. Besides the retrospective pattern of this study, this issue is beyond the scope of this article.
To conclude, the enlarged cervical lymph nodes in adult males at the supraclavicular region seem to have a priority in tissue sampling for excluding malignancy.
Acknowledgements
The authors state that there wasn't any financial support was taken from any third person or companies at any stage of this article.
Conflict of interest: None.
This study has been approved by Gaziantep university ethical committee with a number of 2019/225
Reference
1) Penn EB, Goudy SL. Pediatric inflammatory adenopathy. Otolaryngol Clin North Am. 2015;48(1):137-151. doi:10.1016/j.otc.2014.09.010 [ Özet ]
2) Leung AKC, Davies HD. Cervical lymphadenitis: Etiology, diagnosis, and management. Curr Infect Dis Rep. 2009;11(3):183-189. doi:10.1007/s11908-009-0028-0 [ Özet ]
3) Neff L, Newland JG, Sykes KJ, Selvarangan R, Wei JL. Microbiology and antimicrobial treatment of pediatric cervical lymphadenitis requiring surgical intervention. Int J Pediatr Otorhinolaryngol. 2013;77(5):817-820. doi:10.1016/J.IJPORL.2013.02.018 [ Özet ]
4) Deosthali A, Donches K, DelVecchio M, Aronoff S. Etiologies of Pediatric Cervical Lymphadenopathy: A Systematic Review of 2687 Subjects. Glob Pediatr Heal. 2019;6:2333794X1986544. doi:10.1177/2333794x19865440 [ Özet ]
5) Werner MT, Zhao C, Zhang Q, Wasik MA. Nucleophosmin-anaplastic lymphoma kinase: the ultimate oncogene and therapeutic target. Blood. 2017;129(7):823-831. doi:10.1182/blood-2016-05-717793 [ Özet ]
6) Abadi U, Peled L, Gurion R, et al. Prevalence and clinical significance of hypercalcemia at diagnosis in diffuse large B-cell lymphoma. Leuk Lymphoma. June 2019:1-5. doi:10.1080/10428194.2019.1620946 [ Özet ]
7) Fernández Aceñero MJ, Caso Viesca A, Díaz del Arco C. Role of fine needle aspiration cytology in the management of supraclavicular lymph node metastasis: Review of our experience. Diagn Cytopathol. 2019;47(3):181-186. doi:10.1002/dc.24064
8) Nasuti JF, Mehrotra R, Gupta PK. Diagnostic value of fine-needle aspiration in supraclavicular lymphadenopathy: A study of 106 patients and review of literature. Diagn Cytopathol. 2001;25(6):351-355. doi:10.1002/dc.10002
9) Matasar MJ, Zelenetz AD. Overview of lymphoma diagnosis and management. Radiol Clin North Am. 2008;46(2):175-198, vii. doi:10.1016/j.rcl.2008.03.005 [ Özet ]
10) Morris-Stiff G, Cheang P, Key S, Verghese A, Havard TJ. Does the surgeon still have a role to play in the diagnosis and management of lymphomas? World J Surg Oncol. 2008;6. doi:10.1186/1477-7819-6-13 [ Özet ]
11) Hetemoğlu EK, Selim ;, Erbek S. PREDICTING MALIGNANCY IN CERVICAL LYMPH NODE: CLINICAL RESULTS. KBB-Forum . 2019;18(1):28-32. [ Özet ] www.KBB-Forum.net.
12) Celenk F, Gulsen S, Elif Baysal ?, Aytac ? Ismail, Kul S, Kanlikama ? Muzaffer. Predictive factors for malignancy in patients with persistent cervical lymphadenopathy. Eur Arch Otorhinolaryngol. 2016;(273):251-256. doi:10.1007/s00405-015-3717-3 [ Özet ]
13) Patra DK, Nath S, Biswas K, De J, Sarkar R. Diagnostic evaluation of childhood cervical lymphadenopathy by fine needle aspiration cytology. J Indian Med Assoc. 2007;105(12):694-696, 698-699. http://www.ncbi.nlm.nih.gov/pubmed/18478730. Accessed June 7, 2019. [ Özet ]
14) Locke R, Comfort R, Kubba H. When does an enlarged cervical lymph node in a child need excision? A systematic review. Int J Pediatr Otorhinolaryngol. 2014;78(3):393-401. doi:10.1016/j.ijporl.2013.12.011 [ Özet ]
15) Al Kadah B, Popov HH, Schick B, Knöbber D. Cervical lymphadenopathy: study of 251 patients. Eur Arch Otorhinolaryngol. 2015;272(3):745-752. doi:10.1007/s00405-014-3315-9 [ Özet ]
16) Sandlund JT, Downing JR, Crist WM. Non-Hodgkin"s Lymphoma in Childhood. N Engl J Med. 1996;334(19):1238-1248. doi:10.1056/NEJM199605093341906 [ Özet ]
17) Karadeniz C, Oguz A, Ezer U, Ozturk G, Dursun A. THE ETIOLOGY OF PERIPHERAL LYMPHADENOPATHY IN CHILDREN. Pediatr Hematol Oncol. 1999;16(6):525-531. doi:10.1080/088800199276813 [ Özet ]
18) Gupta RK, Naran S, Lallu S, Fauck R. The diagnostic value of fine needle aspiration cytology (FNAC) in the assessment of palpable supraclavicular lymph nodes: a study of 218 cases. Cytopathology. 2003;14(4):201-207. http://www.ncbi.nlm.nih.gov/pubmed/12873313. Accessed June 12, 2019. [ Özet ]
19) Soldes OS, Yunger JG, Hirschl RB. Predictors of malignancy in childhood peripheral lymphadenopathy. J Pediatr Surg. 1999;34(10):1447-1452. doi:10.1016/S0022-3468(99)90101-X10549745
20) Karaman A, Karaman İ, Çavuşoğlu YH, Erdoğan D. The ongoing problem with peripheral lymphadenopathies: which ones are malignant? Pediatr Surg Int. 2010;26(3):247-250. doi:10.1007/s00383-009-2498-4 [ Özet ]
21) Lake AM, Oski FA. Peripheral Lymphadenopathy in Childhood. Am J Dis Child. 1978;132(4):357. doi:10.1001/archpedi.1978.02120290029003 [ Özet ]
22) López F, Rodrigo JP, Silver CE, et al. Cervical lymph node metastases from remote primary tumor sites. Head Neck. 2016;38:E2374-E2385. doi:10.1002/hed.24344
23) Celenk F, Baysal E, Aytac I, et al. Incidence and predictors of malignancy in children with persistent cervical lymphadenopathy. Int J Pediatr Otorhinolaryngol. 2013;77(12):2004-2007. doi:10.1016/J.IJPORL.2013.09.022 [ Özet ]




