BASAL CELL ADENOMA OF SALIVARY GLAND; CYTOLOGIC FEATURES AND DIFFERENTIAL DIAGNOSIS
2Acibadem Hastanesi, Merkez Patoloji Laboratuvarı, İstanbul, Türkiye
3Nişantaşı Patoloji Grubu, İstanbul, Türkiye
4Maltepe Üniversitesi Tıp Fakültesi, KBB Anabilim Dalı, İstanbul, Türkiye
Summary
Herein, a case of Basal Cell Adenoma of the parotid gland is presented, especially with cytologic features and cytologic differential diagnosis was discussed.Basal Cell Adenoma is a rare neoplasm which is one of the basaloid neoplasms of salivary gland cytologically. Basaloid neoplasms are the most difficult problem in salivary gland Fine Needle Aspiration Cytology. There are various benign and malignant tumors such as; cellular pleomorphic adenoma, basal cell adenocarcinoma, adenoid cystic carcinoma, metastatic basal cell carcinoma, metastatic basaloid squamous carcinoma and small cell carcinoma in differential diagnosis.
Fine Needle Aspiration Cytology in salivary gland lesions can provide a diagnosis that eliminates the need for surgery in non-neoplastic lesions and guides treatment decision.
Introduction
Basal cell adenoma (BCA) of the salivary gland is a rare neoplasm consists of a monomorphic population of basaloid epithelial cells, and it accounts for approximately 1% to 2% of all salivary gland tumors[1]. BCA appears most frequently in the parotid glands and in Adult[2-6]. Clinically, BCA is usually a slow-growing, asymptomatic, and freely movable mass.A review of large series shows that fine needle aspiration cytology (FNAC) of salivary gland tumors is safe, easy to perform, and accurate; all palpable salivary tumors should therefore be studied cytologically[7]. FNAC in salivary gland lesions can provide a diagnosis that eliminates the need for surgery in non-neoplastic lesions and guides treatment decision.
A case of BCA is presented especially with cytologic features and cytologic differential diagnosis was discussed.
Case Presentation
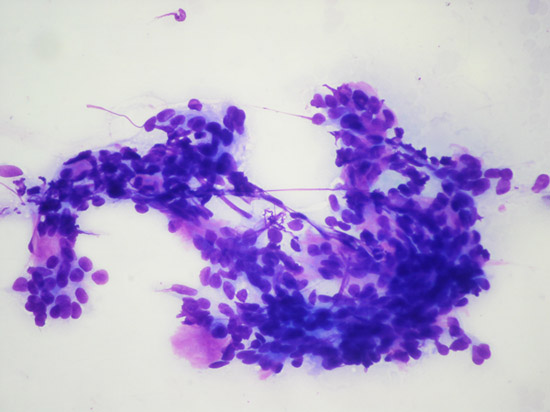
Thirty-eight years-old female patient with a complaint of swelling in right parotid region was examined in ear-nose-throat clinic. On physical examination two small round masses were noted in the right parotid gland. Cervical lymph nodes were not palpable and facial nerve function was normal. FNAC revealed small basaloid type epithelial cells forming cohesive groups. Two populations of epithelial cells were recognized in some areas; cells with larger nuclei and moderate amounts of cytoplasm, and a second population of basaloid cells with dark nuclei and scant cytoplasm. Occasionally basal membrane like material was seen. Palisading of the nuclei was observed at the periphery of some epithelial groups, Distinct stromal component, hyaline globule, necrosis, and prominent cytological atypia were not seen (Fig. 1,2). The case was signed out as “basaloid neoplasm” and a note was added to the cytology report; “The diagnosis of -basaloid neoplasm- includes; basal cell adenoma, cellular pleomorphic adenoma, basal cell adenocarcinoma, adenoid cystic carcinoma, metastatic basal cell carcinoma, metastatic basaloid squamous carcinoma and small cell carcinoma which can not frequently be differentiated by cytology alone. However, features suggesting high grade malignancy was not observed and cytomorphologic findings are primarily consisted with a benign neoplasm. Clinical correlation is recommended”.
 Büyütmek İçin Tıklayın |
Figure 1: Basaloid type epithelial cells MGGX100 |
 Büyütmek İçin Tıklayın |
Figure 2: Basaloid type epithelial cells MGGX100 |
Superficial parotidectomy was performed and the nodule was excised.
Macroscopically, an encapsulated tumoral lesion having a yellow-colored cut-surface measuring 2.5x1.8x1.7 cm. was detected. The second nodule measuring 1.2x1x0.7 cm. was a tumoral lesion showing the same features with the main tumor.
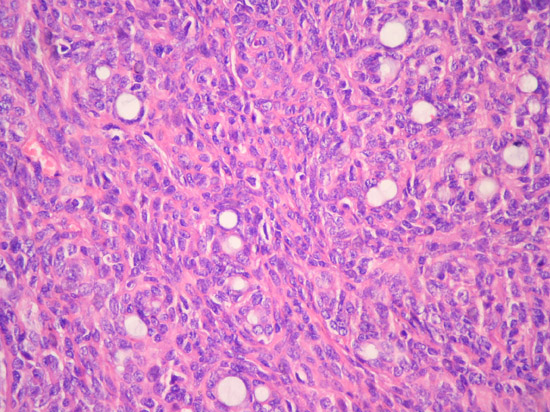
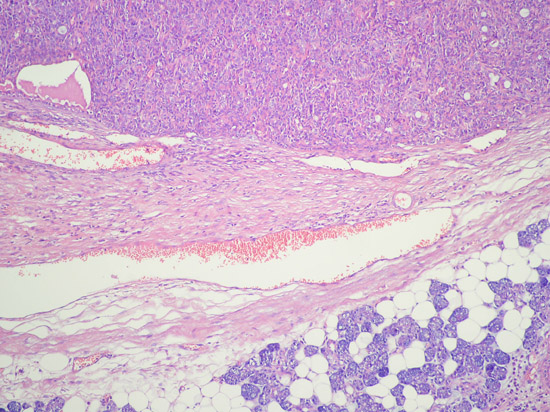
Microscopic examination revealed epithelial nests showing palisading basaloid appearance with a tubulo-trabecular pattern (Fig. 3, 4). The tumor cells were appeared uniform. Occasional small spaces were present throughout the solid clusters of tumor cells. Necrosis, significant mitotic activity or pleomorphism could not be detected. No myoepithelial cells were identified. Although the tumor was surrounded by a relatively thick collagenous capsule (Fig. 5), it invaded the peripheral tissue in a focal area. A few satellite tumoral nodules (Fig. 6) were detected but no widespread invasion was found; therefore the diagnosis of basal cell adenocarcinoma was excluded.
 Büyütmek İçin Tıklayın |
Figure 3: Tubulo-trabecular pattern, Cell Block X200 |
 Büyütmek İçin Tıklayın |
Figure 4: Tubulo-trabecular pattern X200 |
 Büyütmek İçin Tıklayın |
Figure 5: Thick collagenous capsule X200 |
 Büyütmek İçin Tıklayın |
Figure 6: Satellite tumoral nodules X100 |
Conclusion
Basaloid neoplasms are the most difficult problem in salivary gland FNAC[8]. A total of 42 cases of cytologically diagnosed BCA have been reported in the literature. False-positive and false-suspicious diagnoses accounted for 16.7% of cases, illustrating the difficulties in disinguishing between BCA and adenoid cystic carcinoma[7].There are various benign and malignant tumors in differential diagnosis. Although, cytologic atypia, necrosis and significant mitotic activity exclude BCA, the absence of these malignant features does not exclude a malignancy, such as adenoid cystic carcinoma and basal cell adenocarcinoma. Stromal material in BCA often surrounds the neoplastic cells, in contrast adenoid cystic carcinoma, in which cells almost always surround stroma. The matrix material of BCA can be hyalinized, whereas in adenoid cystic carcinoma it is more typically transparent. Additionally, the presence of squamous differentiation exclude adenoid cystic carcinoma, which never exhibits squamous differentiation[8]. Basal cell tumors lack scattered myoepithelial plasmacytoid cells. Inversely, pleomorphic adenomas usually lack the naked nuclei frequently present in basal cell tumors[7]. Although, basal cells can mimic myoepithelial cells, they do not have a plasmacytoid shape. Basaloid neoplasms are also characterized by the presence of three-dimensional dark clusters and peripheral palisading.
Clinical evidence of malignancy as well as a complete history may also be helpful in distinguishing these entities.
In many cases, however, a definitive diagnosis is not possible and signed out as “basaloid neoplasm” noting the presence or absence of features suggesting malignancy and offering a differential diagnosis.
Because of the BCA may have solid and cystic component, the imaging findings have been described as relatively non-specific. Although it can be cystic[9], was purely solid in our patient.
Histopathologically; it has four growth patterns as a solid, trabecular, tubular and membranose type[10]. Our case had tubular and trabecular patterns. BCA is a solid but occasionally cystic and usually encapsulated tumor with well borders. A few cases of bilateral BCA have been reported[11].
But we could not find any report in the literature, which notify a presentation of BCA with unilateral multinodularity like our case. In differential diagnosis; there are several tumors, such as myoepithelioma, pleomorfic adenoma. These possibilities may be excluded with a careful examination. Myoepithelioma and pleomorfic adenoma have myoepithelial cells and later has myxochondroid elements characteristically.
Therapy of BCA is simple total surgical excision. So, pre-operative cytologic diagnosis is very useful for preventing from an aggressive surgery. The case was diagnosed as “basaloid neoplasm, favor benign” by FNAC and superficial parotidectomy was performed and the patient was protected from a radical operation.
Although cytologically, there are diagnostic difficulties in many salivary gland tumors, FNAC is a cost-effective technique that spares as many as one-third of patients unnecessary surgery in experienced hands.
Reference
1) Lee D K, Chung K W, Baek C H, Jeong H S, Hyen Y, Son I S. Basal cell adenoma of the parotid gland characteristic of 2-phase helical computed tomography and magnetic resonance imaging. J Comput Assist Tomogr 2005;29:884-88. [ Özet ]
2) Batsakis JG, Brannon RB, Sciubba JJ. Monomorphic adenomas of major salivary glands. A histologic study of 96 tumours. Clin Otolaryngol 1981, 6: 129-143. [ Özet ]
3) Gök Ü, Sakallıoğlu Ö, Dağlı A. F. Basal cell adenoma of the parotide gland: case report. Fırat Tıp Dergisi 2006;11: 150-152.
4) J H P Main, J A Orr, F M McGurk, R J McComb D Mock. Salivary gland tumour:review of 642 cases. J Oral Pathol 1976; 5:88-102. [ Özet ]
5) L T Byars, L V Ackerman, E Peacock, Tumours of the salivary gland origin in children. A clinical pathologic appraisal of 24 cases. Ann Surg 1957; 146: 40-51. [ Özet ]
6) Hara H, Oyama T, Saku T. Fine needle aspiration cytology of basal cell adenoma of the salivary gland. Acta Cytol. 2007; 51:685-91.
7) Klijanienko J, Vielh P. Adenomas. In: Salivary Gland Tumors. Eds: Klijanienko J, Vielh P. Chapter 6. Karger, Basel. 2000, pp: 22-47.
8) Krane J.F, Faquin W.C. Salivary Gland. In: Cytology. Diagnostic Principles and Clinical Correlates. Eds: Cibas E.S, Ducatman B.S. Second ed. Chapter: 10. Saunders, Edinburgh. 2003, pp: 273-307. 9) Yerli H, Aydin E, Coşkun M, Geyik E, Özlüoğlu L N, Haberal N, Kaskati T. Dynamic multislice computed tomography findings for parotid gland tumors. J Comput Assist Tomogr 2007; 31:309-16. [ Özet ]




