PRIMARY KAPOSI SARCOMA OF THE PAROTID GLAND IN A HUMAN IMMUNODEFICIENCY VIRUS (HIV) - NEGATIVE PATIENT
2Gazi Üniversitesi Tıp Fakültesi , Patoloji AD, Ankara, Türkiye
Summary
Kaposi Sarcoma (KS) is almost always a malignancy of immunocompromised patients who are mostly Human Immunodeficiency Virus (HIV) - positive and occurrence in an immunocompetent patient is extremely rare. A 54-year-old female patient admitted with a neck mass, and the mass slowly enlarged despite antibiotic treatment during three months follow-up period. Fine needle aspiration biopsy (FNAB) was not diagnostic. A core biopsy was done and Human Herpes Virus (HHV) -8 positive KS was diagnosed. HIV serology, magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET/CT) was obtained. The patient was HIV negative. MRI revealed that the mass was located within the parotid tail. In PET/CT, a submandibular lymph node with low pathological activity was also detected. Excision of the parotid tail and a selective neck dissection (levels I-III) was performed. Final pathological examination revealed HHV-8 positive KS. Since surgical margins were negative, no adjuvant therapy was administered. Although quite rare, primary KS can develop within parotid gland in HIV negative individuals. Surgical resection of the lesion with clear margins is mainstay of the treatment.Introduction
Kaposi Sarcoma (KS) was first described in 1872 by Moritz Kaposi[1]. KS is an angioproliferative disease which derives from endothelial cells. KS is characteristically a low-grade multifocal malignant neoplasm which mainly affects skin and mucous membranes but lymph node and visceral organ involvement is also not uncommon[2]. Head and neck involvement in KS is not unusual but mainly seen in Human Immunodeficiency Virus (HIV) - positive individuals. Primary salivary gland involvement is quite rare. In this case report, we present an extremely rare form of KS arising from parotid gland of an HIV - negative, immunocompetent female patient.Case Presentation
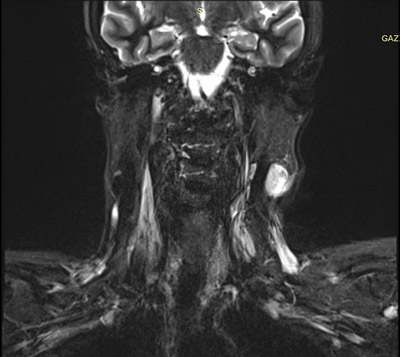
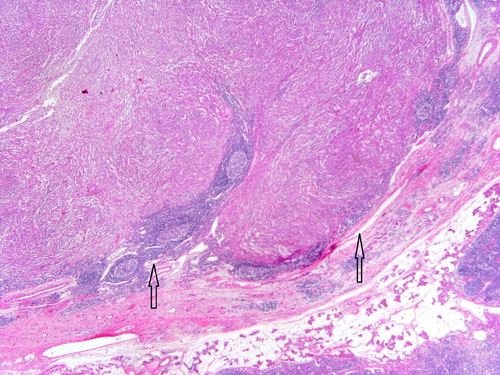
A 58-year-old female was admitted to our department with a complaint of a slowly growing painless left upper neck mass for one month. The patient had diabetes mellitus, hypertension, hyperlipidemia, penicillin allergy and had tonsillectomy and hysterectomy with bilateral ooferectomy before. Physical examination revealed a smooth, non-tender and mobile mass lesion located at left upper jugular region. A small lymph node, 14×11 mm in diameter, was detected at lymph node level II by ultrasound (US) and the patient used a course of antibiotic treatment for ten days. However the mass slowly enlarged and reached to a size of 22×14 mm according to the US, three months later. Fine needle aspiration biopsy (FNAB) was performed but no definitive diagnosis obtained due to insufficient cellularity. An US guided core biopsy was done and the diagnosis was KS. After diagnosis of KS, signs and symptoms of an immunodeficiency situation was questioned in past medical history but there was no evidence. There was no additional skin or mucosal lesion on physical examination. HIV serology was negative, complete blood count and peripheral blood smear were normal. Magnetic resonance imaging (MRI) and positron emission tomography/computed tomography (PET/CT) were obtained. On MRI images, the mass was located within the parotid tail (Figure 1). PET/CT revealed pathological 18F-fluorodeoxyglucose (18F-FDG) uptake of the primary lesion (maximum standardized uptake value [SUV-max]: 4.1) and low pathological 18F-FDG uptake (SUV-max: 2.1) at a submandibular lymph node. Parotid tail resection and an ipsilateral selective neck dissection (levels I-III) were performed. Postoperative period was uneventful. Microscopic examination of the surgical specimen showed spindle cell tumor growth (Figure 2). The tumor was composed of angiomatoid slit-like vascular spaces containing red blood cells surrounded by spindle cells (Figure 3). The spindle cells were arranged in intersecting fascicles and infrequent mitotic figures. The tumor cells showed immunoreactivity for cluster of differentiation (CD) - 31 and human herpes virus (HHV) - 8, thus a diagnosis of KS was made. According to the final pathology report, surgical margins were clear and there were no metastatic lymph nodes. Since surgical margins were clear and there was no metastatic lesion, adjuvant chemotherapy or radiotherapy were not planned. The patient was free of recurrence within a postoperative follow-up period of three months.
 Büyütmek İçin Tıklayın |
Figure 1: View of the lesion on magnetic resonance imaging, T2-weighted coronal section. |
 Büyütmek İçin Tıklayın |
Figure 2: Histology of lymph node shows spindle cell tumor of Kaposi's sarcoma (HE, ×100) |
 Büyütmek İçin Tıklayın |
Figure 3: The spindle cells form intersecting fascicles and are separated by characteristic slit-like spaces containing erythrocytes (HE, x400) |
Discussion
KS is generally accepted as a low-grade mesenchymal lesion which mostly affects mucocutaneous regions but it is still controversial that the KS is whether a true malignancy or a proliferative/inflammatory lesion[3]. The exact etiopathogenesis of KS is still in the dark however it has been recently discovered that HHV-8 has an important role[1]. Together with HHV-8, HIV infection and exposure to iron and some other minerals are suggested to have a role on the development of KS[4].Although KS is a heterogeneous disease, four major groups have been determined in regard to the affected patient population and the epidemiologic basis: endemic or African form, epidemic form, classic or sporadic form, and immunosuppression-related form[4]. The African form is endemic among young African males and infants, the epidemic form affects HIV-positive individuals, and the immunsuppression-related form is seen in patients who had transplantation and using immunosuppressant agents. Finally the classic or sporadic form is mostly seen in elderly males who have Mediterranean origin. Our patient was from Inner Anatolian region and according to this classification, our patient belongs to the sporadic group.
Clinical presentation of KS is highly variable. Head and neck involvement is not uncommon and mostly related with HIV infection[4,5]. Oral cavity is the most common location within the head and neck region and the hard palate and gingiva are the most common locations within the oral cavity[5]. According to a literature review by Patrikidou et al., oral cavity, ear, oropharynx, and palate are the most frequently involved sites in 251 non-HIV KS patients[6]. There are only two non-HIV KS cases involving the major salivary glands according to this literature review.
KS may involve both the salivary gland parenchyma and intraparotid lymph nodes[2]. Parotid and submandibular glands may be involved but the parotid gland involvement is more frequent[2]. As in our case, the patients with salivary gland KS present with a mass or swelling of the salivary gland[7]. Similar to other head and neck regions, KS located at salivary glands are commonly associated with HIV infection[7] FNAB is reported to be a reliable diagnostic tool in KS however in our case a core biopsy was required for definite diagnosis[8]. Because of the heterogeneous nature of the disease, a worldwide accepted treatment guideline is not present[4]. KS management depends on extent of the disease, epidemiological form, and location of the lesion. Local treatment options include surgical excision, cryotherapy, laser applications, and topical applications of chemotherapeutics[6]. External radiotherapy and systemic chemotherapy are other options. Local excision is the treatment of choice in limited and sporadic cases[4]. In the case of parotid involvement, surgical excision was also reported as the treatment of choice[7,9,10].
KS located at salivary glands are usually related with a previously known HIV infection. However diagnosis of KS within parotid gland may be related with a subclinic HIV infection and may lead to the diagnosis of HIV infection[11]. On the other hand, parotid gland involvement may occur in an immunocompetent and HIV - negative patient very rarely as in our case.
Reference
1) Schwartz RA. J Surg Oncol 2004; 87: 146-51. Review. Kaposi's sarcoma: an update. [ Özet ]
2) Pantanowitz L, Dezube BJ. Kaposi sarcoma in unusual locations. BMC Cancer 2008; 8: 190. [ Özet ]
3) Schwartz RA, Micali G, Nasca MR, Scuderi L. Kaposi sarcoma: a continuing conundrum. J Am Acad Dermatol 2008; 59: 179-206. [ Özet ]
4) Szajerka T, Jablecki J. Kaposi's sarcoma revisited. AIDS Rev 2007; 9: 230-6. [ Özet ]
5) Ramírez-Amador V, Anaya-Saavedra G, Martínez-Mata G. Kaposi's sarcoma of the head and neck: a review. Oral Oncol 2010; 46: 135-45. [ Özet ]
6) Patrikidou A, Vahtsevanos K, Charalambidou M, Valeri RM, Xirou P, Antoniades K. Non-AIDS Kaposi's sarcoma in the head and neck area. Head Neck 2009; 31: 260-8. [ Özet ]
7) Castle JT, Thompson LD. Kaposi sarcoma of major salivary gland origin: A clinicopathologic series of six cases. Cancer 2000; 88: 15-23. [ Özet ]
8) Gamborino E, Carrilho C, Ferro J, Khan MS, Garcia C, Suarez MC, Yokoyama H, Schmitt FC. Fine-needle aspiration diagnosis of Kaposi's sarcoma in a developing country. Diagn Cytopathol 2000; 23: 322-5 [ Özet ]
9) Puxeddu R, Parodo G, Locci F, Puxeddu I, Manconi PE, Ferreli C. Parotid mass as an early sign of Kaposi's sarcoma associated with human herpesvirus 8 infection. J Laryngol Otol 2002; 116: 470-3. [ Özet ]
10) Pagani D, Bellinvia M, Capaccio P, Scoppio B, Brambilla L, Pignataro L. An unusual cause of a parotid mass in an immunocompetent host: classic Kaposi's sarcoma. Tumori 2009; 95: 248-50. [ Özet ]
11) Steele NP, Sampogna D, Sessions RB. Kaposi's sarcoma of an intraparotid lymph node leading to a diagnosis of HIV. Laryngoscope 2005; 115: 861-3. [ Özet ]




