SHORT TERM RESULTS OF OSSICULER RECONSTRUCTION WITH TITANIUM-GOLD TOTAL OSSICULAR REPLACEMENT PROSTHESIS IN CHRONIC OTITIS MEDIA SURGERY
Summary
In this report, results of the applications of titanium-gold total ossicular replacement prosthesis are presented and they are compared with other types of prosthesis used in clinical practice.
Material & Method
This study was performed on 24 patients, 14 male and 10 female, aged between 13 to 67. In all patients, primary pathology was chronic cholesteatomatous otitis media, and none of them were revision cases. In all cases, canal wall down technique tympanoplasty type 3 was performed with titanium-gold prosthesis. A thin block of conchal cartilage was put over the plate of the prosthesis and ear drum was reconstructed with autograft temporalis muscle fascia in all cases. The control group consisted of 30 patients operated for same middle ear pathology. In these cases, surgeries were similar except the prostheses that have been used. In this group, in seven of patients pure hydroxyapatite TORP`s were used; in the rest, the choice was a hydroxyapatite polyethilen hybrid prosthesis. An average air-bone gap for all calculated frequencies of 0.5, 1, and 2 kHz was investigated in study and control groups. Statistical analysis is performed using Independent-Samples T Test.
Results
There was no statistically significant difference in post-operative hearing gain between control and study groups. In the study group all but two tympanic membrane healed well, in 22 cases, the prostheses remained stable. Only in one case the slipage of the cartilage cover caused a partial show up of prosthesis without extrusion at fourth mounth. In one out of 30 patients in control group, the grafts were intact up to 1 year, and in one case, extrusion of the hydroxyapatite TORP was seen. When the air-bone gap "gold standard" (i.e., < or =10 dB) was investigated in the main speech spectrum, 2 patients from the study group and 2 patients from the control group had post-operative air-bone gap < or =10 dB. An average air-bone gap between 11-20 dB was achieved in 19 patients in study group and in 21 patients in control group. A post-operative air-bone gap between 21-30 dB was achieved in 3 patients in study group and in 6 patients in control group. In one case in the control group, hearing was deteriorated.
Conclusion
Initial evaluation of the titanium-gold prostheses produced low extrusion rates with acceptable hearing results. We have found this prosthesis as successful as hydroxyapatite and hydroxyapatite hybrid prostheses, when used in a similar situations.
Introduction
One of the most difficult problem in chronic otitis media surgery is to rebuilt the sound transmission mechanism in ears without ossicles. After 1980s, many biomaterials have been used to replace ear ossicles[1]. Metallic prostheses have been less accepted than plastics and ceramics.Limitations in biocompatibility and hearing improvement with ossicular chain reconstruction prostheses are addressed with new, lightweight titanium prostheses[2]. Since 1993, titanium prostheses have been used in Europe as a biocompatible implant for ossicular reconstruction[3]. Titanium is known well-tolerated in various surgical procedures[4]. Pure titanium or titanium-gold middle ear prostheses have been reported to be succesful. They may be re-sized to the necessary length at the time of the surgery. It consist of a cup, a shaft and a headplate. Because of it`s design characteristics, the surgeon can see this prostheses on the footplate[2]. The headplate is open, thus allowing the surgeon to see through the headplate, and the shaft is narrow, allowing better vision around the device[2]. The shape and easy to insert of titanium gold prostheses was found to be attractive and was used in 24 chronic otitis media cases in our clinic.
In this report, short term results of titanium-gold prosthesis were presented and they were compared with other types of prosthesis used in clinical practice.
Methods
This study was performed on 24 patients (14 male and 10 female), aged between 13 to 67, with an average age of 36. In all patients, primary pathology was chronic cholesteatomatous otitis media , and none of them were revision cases. During surgery, all ossicles were found to be destroyed and/or nonusable in all patients. As a result of chronic cholesteatomatous otitis media, the middle ear mucosa was inflamated, edematous and mucosal ulceration and breakdown of the epithelial lining was observed. Canal wall down technique tympanoplasty type 3 with titanium-gold prostheses was performed to all cases. The piston of the implant was inserted over the oval window, a thin block of conchal cartilage was put over the plate of the prosthesis and ear drum was reconstructed with autograft temporalis muscle fascia in all cases. Patients were followed-up regularly, 6 to 12 months, and they were evaluated audiologically and otomicroscopically.The control group consisted of 30 patients operated for same middle ear pathology. In these cases, surgeries were similar except the prostheses that have been used. In this group, in seven of patients pure hydroxyapatite TORP`s were used; in the rest, the choice was a hydroxyapatite polyethilen hybrid prosthesis. A thin block of conchal cartilage was also put over the plate of the prosthesis and ear drum was reconstructed with autograft temporalis muscle fascia in all cases. An average air-bone gap for all calculated frequencies of 0.5, 1, and 2 kHz was investigated in study and control groups. Success was based on the hearing gain postoperatively. Statistical analysis was performed using Independent-Samples T Test.
Results
In the study and the control groups, the mean postoperative air-bone gaps were 16,08 dB (SD: 4,74) and 17,80 dB, (SD: 7,49) respectively. There were no statistically significant difference in post-operative hearing gain between control and study groups (p=0,333).In the study group, all but two tympanic membrane healed well, in 22 cases, the prostheses remained stable. Only in one case the slipage of the cartilage cover caused a partial show up of prosthesis without extrusion at the fourth mounth. In one out of 30 patients in control group, the grafts were intact up to 1 year, and in one case, extrusion of the hydroxyapatite TORP was seen.
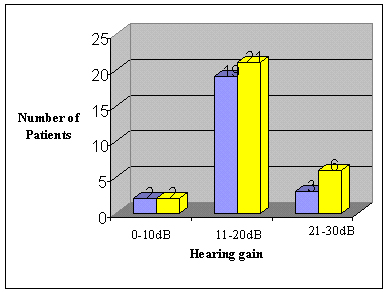
When the air-bone gap "gold standard" (i.e., < or =10 dB) was investigated in the main speech spectrum, 2 patients from the study group and 2 patients from the control group had post-operative air-bone gap < or =10 dB. An average air-bone gap between 11-20 dB was achieved in 19 patients in study group and in 21 patients in control group. A post-operative air-bone gap between 21-30 dB was achieved in 3 patients in study group and in 6 patients in control group. In one case in the control group, who developed extrusion of the hydroxyapatite TORP, hearing was deteriorated.
 Büyütmek İçin Tıklayın |
Grafik 1: Postoperative hearing gains in study (blue) and control (yellow) groups. |
Discussion
After the eradication of the cholesteatoma, the reconstruction of the ossicular system may need some skill and of course some material which is suitable to the middle ear. Middle ear is known to be immunologically low reactive[5,6], so various kinds of materials can be used in chronic otitis media surgery. Failures may be mainly due not to the immunological reactions but due to technical aspects. An adequately shaped implant used with adequate tension between the reconstructed tympanic membrane and oval window generally gives good results [4,7]. In order to achieve this goal, one should put a piece of cartilage over the platform of the prosthesis.In English literature the most widely used TORP is mainly hydroxyapatite base. Recently, prosthesis with hydroxyapatite platform and a kind of plastic shaft have gained popularity. The use of metallic prostheses come mainly from German studies[4] and show similar results with hydroxyapatite prostheses. Most widely used metallic prostheses are titanium gold and titanium prostheses.
In this study, the variables which could have effect on the outcome of the reconstruction, have been kept in mind and both the study and control cases have been chosen among the patients who had similar pathologies. So, from the practical point of view, the most important variable was the implant itself.
The shape of the aerial TORP seems to be advantageous in some points: The tip of the shaft is widely contacted with the stapes footplate and the position of the shaft can be checked after the insertion because of the hallow plate. The shaft also can be bended as desired.
Stupp et al. reported on 100 titanium implants and observed no intolerance or implant rejections[8].
Further studies by Stupp et al. of 661 titanium implants demonstrated that closure to within 20dB was achieved in 72% of cases[9]. Wang et al. also reported on their results with titanium prostheses, finding a hearing gain of more than 10dB in 92,7% of 124 ears and an average reduction in air-bone gap of 23,2 dB[10]. In our study, it was found that 87,5% of the patients had an average air-bone gap between 0-20 dB postoperatively.
Krueger et al.[2] stated that Kurz titanium prostheses also had a good high-frequency conduction rates besides producing low extrusion rates and excellent hearing results. Dalchow et al.[11], in their large series with more than 1300 titanium implants; stated that results already showed a very low complication rate. Extrusions occurred only in cases of middle ear atalectasis with resorption of interposed cartilage (<1%). No adverse reaction to the prostheses could be seen, even in histologic reviews. An average air-bone gap less than 20 dB for all calculated frequencies of 0.5, 1, 2, and 4 kHz was achieved for 76% of cases; 43% of cases showed a calculated air-bone gap of less than 10 dB, only 10% higher than 30 dB. Begall and Zimmermann 12 in their study with titanium middle ear implants, focusing mainly on tissue tolerance and functionality; found that despite pathological middle ear conditions, the tissue-implant healing rate was very high. Only in 4.4% of the patients the implants were rejected.
Short term follow up of the titanium-gold prostheses produced relatively high extrusion rates (8,3%) due to unsuccessful reconstruction with autograft temporalis muscle fascia in our study. As compared with the literature mentioned before, the hearing gain of the patients were found within acceptable limits. In planning of this study, the authors based success of the prosthesis on hearing gain postoperatively, but during follow up, it was observed that the extrusion rates of the titanium-gold prostheses were relatively high as compared with the literature. More definitive consequences will come along with long term follow up and more cases.
Conclusion
Initial evaluation of the titanium-gold prostheses produced relatively high extrusion rates with acceptable hearing results. We have found this prosthesis as successful as hydroxyapatite and hydroxyapatite hybrid prostheses, when used in a similar situations. Due to the good morphological and functional results achieved, titanium implants have proven their worth for middle ear micro-surgery.Reference
1) Geyer G. Implants in middle ear surgery. Eur Arch Otorhinolaryngol Suppl. 1992;(1):185-221. [ Özet ]
2) Krueger WW, Feghali JG, Shelton C, Green JD, Beatty CW, Wilson DF, Thedinger BS, Barrs DM, McElveen JT. Preliminary ossiculoplasty results using the Kurz titanium prostheses. Otol Neurotol. 2002;23(6):836-9. [ Özet ]
3) Neff BA, Rizer FM, Schuring AG, Lippy WH. Tympano-ossiculoplasty utilizing the Spiggle and Theis titanium total ossicular replacement prosthesis. Laryngoscope 2003; 113(9):1525-9 [ Özet ]
4) Hildmann H, Luckhaupt H, Schmelzer A. Using cartilage in middle ear surgery HNO. 1996 ;44(10):597-602. [ Özet ]
5) Geyer G. Materials for reconstruction of the middle ear HNO. 1999;47(2):77-91. [ Özet ]
6) Hüttenbrink KB. Surgical treatment of chronic otitis media. III: Middle ear reconstruction HNO. 1994;42(11):701-18. [ Özet ]
7) Mills RP. The influence of pathological and technical variables on hearing results in ossiculoplasty. Clin Otolaryngol 1993;18(3):202-5. [ Özet ]
8) Stupp CH, Stupp HF, Grun D.. Replacement of ear ossicles with titanium prostheses Laryngorhinootologie. 1996;75(6):335-7. [ Özet ]
9) Stupp CH, Dalchow C, Grun D, Stupp HF, Wustrow J. Three years of experience with titanium implants in the middle ear Laryngorhinootologie. 1999;78(6):299-303. [ Özet ]
10) Wang X, Song J, Wang H. Results of tympanoplasty with titanium prostheses. Otolaryngol Head Neck Surg 1999;121(5):606-9. [ Özet ]
11) Dalchow CV, Grun D, Stupp HF. Reconstruction of the ossicular chain with titanium implants. Otolaryngol Head Neck Surg. 2001;125(6):628-30. [ Özet ]
12) Begall K, Zimmermann H. Reconstruction of the ossicular chain with titanium implants. Results of a multicenter study Laryngorhinootologie. 2000;79(3):139-45. [ Özet ]




