PREVALENCE AND RISK FACTORS OF SNORING, OBSTRUCTIVE SLEEP APNEA SYMPTOMS, AND EXCESSIVE DAYTIME SOMNOLENCE IN TRABZON
Summary
Prospective: To investigate the prevalence of snoring, obstructive sleep apnea (OSA) symptoms, and excessive daytime somnolence (EDS) and the correlation with risk factors.Patients and Method: A questionnaire was utilized to determine the prevalence of snoring, apnea, and excessivedaytime somnolence in 3978 people and the data was analyzed seperately for adults and children.
Results: In adults, the prevalence of snoring was % 25.3. It was significantly more common in males (p<0.0005). Snoring was found to have statistically significant correlation with smoking, alcohol consumption, hypothyrodism, hypertension, allergic rhinitis and antidepressant medications. The frequency of OSA in adults was found to be %3.8. It was more common in men (p=0.005). Obstructive sleep apnea was significantly correlated with obesity, smoking, hypertension, allergic rhinitis and antidepressant medications. In adults, rate of OSA with excessive daytime somnolence was % 1.7. It was correlated with smoking, hypertension, allergic rhinitis and antidepressant medications. Snoring was significantly correlated with frequent upper respiratory tract infections, allergic rhinitis, speech disorders and bruxism in children.
Conclusion: Our study contributes to the identification of specific risk groups to optimize the diagnostic and therapeutic algorithm. The raised alertness on the frequency, co-morbidities, and consequences of sleep disorders will help management of related pathologies.
Introduction
Obstructive sleep apnea is characterized by snoring and recurrent apnea. Apnea is defined as the cessation of respiration for at least 10 seconds[1].Symptomatology and consequences of obstructive sleep apnea necessitates the differential diagnosis from snoring. Obstructive sleep apnea is a common disease that may result in serious familial, social, and medical hazards. In children, OSAS may co-exist with sleep disorders and behavioural problems and may lead to neurodevelopmental abnormalities, growth and cardiorespiratory failure[2]. OSAS impairs social functioning, work performance and driving ability, and accounts for a large socio-economic burden on the community[1].The gold standard in diagnosis of OSAS is polysomnography[3]. It is not a practical diagnsotic tool since it calls for “time, team and money”. Limited number of centers have polisomnography laboratories, therefore we used a questionnaire interview alternatively to monitore this cross-sectional study.
Although now acknowledged as a worldwide problem, the majority of affected individuals remain undiagnosed. To our knowledge, no cross-sectional study on prevalence of OSAS had been conducted in our country. Such studies are required to reveal the possible factors contributing to the pathophysiology and to establish preventive and therapeutic protocols for the disease.We hope that this study can contribute to epidemiological database of Turkey, and that it can provide a perspective for selection of people who cannot readily obtain medical service for sleep related problems.
Methods
This cross-sectional, prospective, field study was conducted in Trabzon between July 2006 and June 2007 after the approval of local ethical committee.
Calculation of sample size
The estimated sample size was calculated with respect to the population of Trabzon, which is 190.861 in the year 2000. Considering the expected incidence of OSAS to be 3-4%, with 95% confidence interval and 0.5% deviation, at least 3746 people should be included in the study. The age and gender distribution of the study population was consistent with that of general population of Trabzon.
Selection of samples
Multi-step sampling was used. In the first step, layers were determined according to age groups, gender, and location. In the second step, 12 different regions constituting the downtown were selected. Sample size was estimated for age groups and gender. From each region, a house was randomly assigned and afterwards systematic sampling was performed to reach the aimed number of participants. Interviews were made with all the residents above 2 years of age. Participants were informed on sleep disorders and their consequences. Only patients younger than 2 years of age was excluded from the study.
The parameters to be recorded were age, gender, height, sleeping habits, nocturnal symptoms (sleeping, recurrent apnea, dyspnea, frequent arousal), diurnal symptoms (mouth breathing, excessive somnolence, morning headache, fatigueability), systemic diseases, medications, allergy and smoking status. For children above 2 years of age, additional questions on bruxism, history of nightmares, enuresis nocturna, and school performance were prepared. Questions on nocturnal symptoms were directed to the spouses of the patients. Since polysomnography was unavailable in this study, diagnosis of OSAS was confirmed in case of co-existence of snoring and apnea
The interviews were performed by the medical students who were trained on sleep disorders, and methodology of study. The interviewers visited the families at their homes and asked the quesitons directly to the participants and the parents of children. If the selected family refused to enroll in the study, the interviewers passed to the neighbouring house (See Interview form).
Classification of data
Age: For patients < 20 years of age, groups were formed with 5-year intervals (<5 y, 5-9 y, 10-14 y, 15-19 y). On the other hand, for patients ≥ 20 years, grouping was done for 10-year intervals (20-29 y, 30-39 y, 40-49 y, 50-59 y, ≥60 ).
Smoking habit was classified as smoker, non-smoker, and ex-smoker. Alcohol consumption was classified as consumer, non-consumer and ex-consumer.
Body-mass index (BMI) of patients were calculated according to the formula: BMI= Weight (kg) / height (m)2. The results were classified according to obesity classification of World Health Organization[16].
BMI <18.5: Underweight
18.5 ≤ BMI < 25: Normal
25 ≤ BMI < 30: Overweight
30 ≤ BMI < 40: Obese
BMI > 40: Morbid obese
A total of 3798 people in Trabzon were enrolled in this study. Statistical analysis was performed using Statistical Package for Social Sciences (SPSS 11.5) program. Chi-square test was used for assessment of qualitative data. The p value <0.05 was accepted to be statistically significant.
Results
A total of 3978 people out of 1200 families were involved in the study. Age range was 2-98, and the group consisted of 1983 males and 1995 females. The study group was subclassified into children (2-16 years) and adults (>16 years).The adult group consisted of 3164 people, of which 1553 were men and 1611 were women. The heights and weights of participants were measured during the interviews, and body-mass indexes were calculated. The height and weight measurements were not possible in 255 uncooperative subjects. The distribution of adult subjects according to BMI and gender are shown on Table 1.
Tablo 1: The distribution of adult subjects in respect to BMI and gender
A subgroup of OSAS patients with the symptoms of excessive daytime somnolence were analyzed separately. Therefore three groups were formed: I) Patients with snoring only, II) Patients with OSA symptoms, and III) OSA patients complaining of excessive daytime somnolonce. The distribution of these patients with respect to gender are given in Table 2.
The number of snorers was 801 (25,3%) in the adult group. Rate of males and females with snoring was 33,4% and 17,5% respectively, and this difference was statistically significant (p<0.0005) (Table 2).
The distribution of adult snorers with respect to age groups is presented in Figure 1. It can be observed that the incidence of snoring increases with age and that snoring more likely affects middle-aged or elderly people.
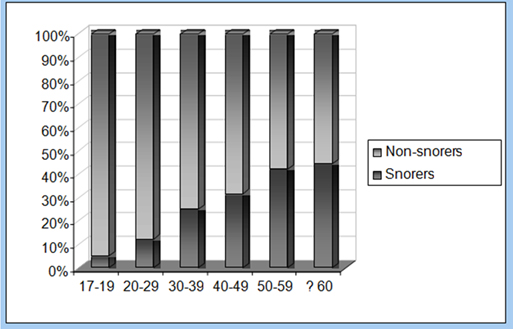 Büyütmek İçin Tıklayın |
Figure 1: Distribution of snoring rate in adults with respect to age groups |
The number of patients with both snoring and apnea was 120 (%3.8). In other words, prevalence of OSAS was estimated to be 3.8%. OSAS prevalence in men and women was 4.8% and 2.9% respectively. The difference between genders was statistically significant (p=0.005).
Distribution of OSAS patients in age groups is demonstrated in Figure 2. Prevalence of OSAS tends to increase with age. Excessive daytime somnolence in addition to OSAS was found in 55 adults (1,7%), of which 24 were women (1,5%) and 31 were men (2%). No statistically significant difference was observed between males and females (p=0.276).
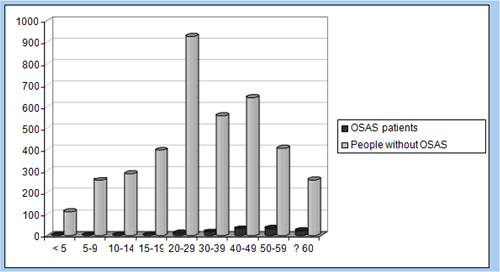 Büyütmek İçin Tıklayın |
Figure 2: Distribution of OSAS patients according to age groups. |
A statistically significant relationship was found between hypothyoidism and snoring (p<0.0005). Allergic rhinitis and antidepressant medication were factors found to be correlated with snoring,OSAS and OSAS +EDS (Table 3).
Table 4 demonstrates the relationship between chronic diseases related to sleep disorders and snoring, OSAS, and EDS in addition to OSAS. The incidences of hypertension in patients with snoring, OSAS, and excessive daytime somnolence in addition to OSAS was significantly higher. There was no statistically significant relationship between diabetes mellitus and snoring, OSAS or OSAS+EDS.
Allergic rhinitis was more frequent in snoring children than those without snoring (p=0.009). The incidence of frequent upper respiratory tract infections in children with and without snoring was 15.4%, and 5.5% respectively (p=0.003).
Stuttering and retardation of speech was more common in the children with snoring (12.8%) than the children without snoring (4.2%). The relationship between snoring and speech disorders was statistically significant (p=0.009). Bruxism was significantly more frequent in children with snoring compared to non-snoring group (p=0.001). However there was no difference between snoring and non-snoring children with respect to enuresis nocturna and frequent nightmares (p=0.113) and (p=0.135) (Table 5).
Tablo 5: Symptomatologic distribution of children with and without snoring
No significant relationship could be found between passive smoking and snoring in children (p=0.860). No significant difference was observed in school performance of children with and without snoring (p=0.675).
Discussion
The earliest, the most common, and the most important symptom of OSAS is snoring. It can occur many years before the existence of other symptoms of OSAS[4]. Unless treated, it may result in excessive daytime somnolence, loss of concentration, and psychological disturbances as well as cor pulmonale, hypertension, stroke, impotence, and genitourinary disorders which may eventually cause deterioration of the life quality of the patient[5]. As the clinical significance of OSAS is unveiled, further studies have been conducted in recent years. Epidemiological studies on prevalence of OSAS can be divided into 3 groups:
1. Studies based on questionnaires investigating habitual snoring and wittnessed apnea. Most of the pioneering studies were of this type.
2. Studies in which polysomnographic assessment of patients selected with respect to results of questionnaire was performed.
3. Studies in which polysomnographic evaluation was routinely made for all patients
The vast majority of recent studies conducted on the prevalence of OSAS are of the second or third type according to the classification above. However, type 1 studies can be useful in studies performed in large populations. Polysomnography is a standard method in diagnosis of sleep apnea. The limited availability of polysomnography due to raised cost and lack of trained personel restricts its utility in epidemiological studies. Therefore studies based on questionnaires may be beneficial to identify risk groups.
In the literature, prevalence of mild OSAS (5 < AHI < 15) and moderate OSAS (15 < AHI < 40) was estimated to be 3-28%, and 1-14% respectively[6,7]. Field studies have revealed that in white race, for a body mass index range of 25-28 the incidences of mild and moderate OSAS were1:5, and 1:15 respectively.
In Turkey, few studies on the prevalence of OSAS have been reported[8]. In one study, the incidence of OSAS in patients with snoring was found to be 9,4%[8]. In a cross-sectional study by Ozdemir et al[9] incidences of snoring and OSAS were estimated to be 37% and 6,4% on 5339 patients. Incidence of snoring in men and women were found to be 33.4% and 17.5% in our study.
Excessive daytime somnolence seems to affect the daytime performance of patients, and may result in morbidity and mortality due to its potential to facilitate accidents[10]. Excessive daytime somnolence is more frequent among patients with high apnea-hypopnea index (AHI). The severity of excessive daytime somnolence is determined by the frequency of nocturnal arousals, and duration of apneas[11]. In our study, 28.2% of snorers and 45.8% of patients with OSAS complained of excessive daytime somnolence .
Obstructive sleep apnea syndrome more commonly occurs in men at 4th-6th decades and its incidence tends to decline after the age of 65. Apnea-hypopnea index (AHI) tends to increase with age, and this increase is most evident after the age of 55[12]. This increase is assumed to be due to changes in body fat composition, tissue elasticity, and tendency of upper airway to collapse. We found that incidences of both snoring and OSAS increased with age and was more frequent after 4th decade. Co-existence of excessive somnolence disorder and OSAS was more common in 4th and 5thdecades.
The male predominance in OSAS patients is related to the androgenic “central” type adipose distribution in the body[13]. The impact of gender on pathogenesis of OSAS changes with age and this change is most prominent in middle ages. Recent studies have shown that predilection for gender was not as prominent as it was thought to be for occurrence of OSAS. For all age groups, the female/male ratio was estimated to be around 1/3[14]. In our study we found that female/ male ratio was 1/2 in snorers, 3/5 in patients with OSAS, and 3/4 in patients with OSAS and excessive daytime somnolence.
There are many studies implicating the increased risk potential of OSAS in obese patients with advanced age[15]. Several mechanisms have been postulated to explain how obesity causesto narrowing and collapse of upper airway. Usually, size of the tongue was found to be larger than average in obese OSAS patients[16]. In addition to that, respiratory muscles were found to be weaker in obese OSAS patients[17]. Therefore, central obesity and OSAS can be related to abnormal upper airway muscle function. In OSAS patients, weight loss causes functional changes rather than structural changes in upper airway[18]. Epidemiological studies have demonstrated an increase in OSAS due to obesity. It was stated that measurement of neck circumference and waist/hip ratio may have predictive value for further development of OSAS[19]. Strohl and Redline[20] have demonstrated that obesity was diagnosed in 11-90% of OSAS patients and neck circumference was measured to be larger in these patients. In our study, we found that increased BMI was significantly correlated with OSAS.
Smoking and alcohol consumption contribute to the development of OSAS via resulting in edema of upper respiratory tract and interfere with the tonus of dilator muscles of pharynx. Alcohol consumption both increases the number of apneas and prolongs the duration of apnea period, and causes to excessive daytime somnolence[21]. Increases in the frequency of snoring and OSAS due to smoking is dose-dependent. In contrast, ex-smokers are not found to be under risk for OSAS[22]. In our study, incidences of snoring in smokers and non-smokers were 39.8% and 19.8% respectively. Smoking was correlated with snoring, OSAS, and OSAS with excessive somnolence disorder.
Asthma, perennial and seasonal allergic rhinitis are frequently diagnosed co-morbidities[23]. Perennial allergic rhinitis causes an inrease in nasal airway resistance due to mucosal congestion. Allergic rhinitis was found to be correlated with snoring, OSAS and OSAS with ESD in our study.
Hypothyroidism increases storage of mucoproteins and decreases the neural output to the muscular structures in upper respiratory tract, thereby facilitating the occurrence of sleep related disorders. The correlation between hypothyroidism and snoring was statistically significant. There was also a statistically significant relationship between antidepressant medication and snoring, OSAS and OSAS with ESD.
Almost 80-90% of OSAS patients worldwide remain undiagnosed. The snorers are usually either unaware of the situation, or they may deny that they are snorers. The history obtained from the partner gains more importance in such circumstances. In the US, the mean period for OSAS patients to be diagnosed is about 10 years, therefore some complications may already have existed by the time of application. The most common complication affecting cardiovascular system is hypertension, and it is encountered in 50% of patients with OSAS. Nocturnal hypoxia results in increase of sympathetic tonus and subsequent changes in baroreceptor functions which leads to increased blood pressure[24]. Hypertension is diagnosed more frequently in patients with OSAS and increased apnea-hypopnea index is correlated with higher incidence of hypertension[25]. The incidence of hypertension in general population, patients with snoring, OSAS, and OSAS with ESD were 9,4%, 18,5%, 27,5% and 36,4% respectively. The difference between groups was significant, hence assessment of hypertensive patients for sleep disorders should not be overlooked. In addition, close follow-up of blood pressure in OSAS patients must be considered as a part of routine evaluation.
Metabolic syndrome consists of central obesity, glucose intolerance and insulin resistance. Oxygen desaturation causes sympathetic nervous system activation and increases catecholamine levels which leads to increased levels of glucose and insulin in blood[26]. Severe OSAS, rather than mild and moderate type, is found to be related with incidence of diabetes mellitus[27]. The influence of sleep disorders on the levels of blood glucose and insulin occurs independently of central obesity[27]. CPAP treatment occurs to be beneficial for hyperglycemia and insulin resistance in diabetic patients[28]. Patients with sleep disorders should be closely monitored for early diagnosis and proper treatment of glucose intolerance. Loss of concentration, anxiety, stuttering, depression, and diminished mental functions are neuropsychological sequelae in patients with OSAS.
We found that the boys were more likely to snore than the girls. In children, obesity was shown to facilitate snoring[29]. Unlike adults, most of the children with OSAS are not obese. Moreover, in some children with OSAS, retardation of growth is noteworthy. Dysphagia due to enlarged tonsils, chronic hypoxia, increased effort to overcome upper airway resistance, and diminished release of growth hormone because of poor sleep quality are possible factors interfering with proper growth of children.
Clinical studies have revealed a correlation between allergic rhinitis and sleep disorders such as snoring and excessive somnolence disorder. It had been shown that incidence of allergic rhinitis was three times more frequent in snorers compared to nonsnorers[30]. Size of palatine tonsils, number of tonsillitis attacks, and asthma are correlated with snoring. Our results revelaed that snoring was correlated with frequent upper respiratory tract infections and allergic rhinitis.
In the literature, symptoms such as bruxism, nightmares, excessive somnolence, problems related with awakening, and mood changes were reported to be more common in patients with snoring[31]. Despite studies stating a relationship between passive smoking and snoring, our findings did not demonstrate such a correlation.
Snoring is an important and common health problem which seriously interferes with the quality oflife. The vast spectrum of morbidities, and mortality due to sleep disorders necessitate the performance of epidemiological studies to identify the possible risk factors and co-morbidities as well as to develop more advanced diagnostic, preventive and therapeutic measures.
Conclusion
Epidemiological data on sleep disorders was collected for the first time in Eastern Black Sea Region of Turkey. Incidences of snoring, OSAS and excessive somnolence disorder were 25.3%, 3.8%, and 1.7% in adults. In adults, a correlation was demonstrated between OSAS and hypertension, obesity, middle age, smoking and allergic rhinitis. In children, the incidence of snoring was estimated to be 7.2%. Snoring was correlated with frequent upper respiratory tract infections, articulation problems, allergic rhinitis, and bruxism in children.Reference
1) Gibson GJ.Obstructive sleep apnoea syndrome: underestimated and undertreated. Br Med Bull. 2005;29:49-65.
2) Chopo GR, Lazaro MA, Ucles P. Obstructive sleep apnea syndrome in childhood. Rev Neurol. 2001;32:86-91.
3) Berg S. Obstructive sleep apnoea syndrome: current status. Clin Respir J. 2005;4:197-201.
4) Polo O, Tafti M, Fraga J, Porkka KV, Déjean Y, Billiard M. Why don't all heavy snorers have obstructive sleep apnea? Am Rev Respir Dis. 1991;143: 1288-1293. [ Özet ]
5) Potolicchio SJ: Disorders of excessive sleepiness. In: Snoring and Obstructive Sleep Apnea, Second edition, NF Fairbanks and S Fugita (Eds), Raven Pres. Ltd. New York, 1994, pp. 45-55.
6) Ip MS, Lam B, Lauder IJ, Tsang KWT, Chung KF, Mok YW, et al. A community study of sleep-disordered breathing in middle-aged Chinese men in Hong Kong. Chest 2001;119: 62-69. [ Özet ]
7) Udwadia ZF, Doshi AV, Lonkar SG, Singh CI. Prevalence of sleep-disardered breathing and sleep apnea in middle-aged urban Indian men. Am J. Respir Crit Care Med. 2004;169: 168-173. [ Özet ]
8) Köktürk O, Tatlıcıoğlu T, Kemaloğlu Y, Fırat H, Çetin N. Habituel horlaması olan olgularda obstrüktif uyku apne sendromu prevalansı. Tüberküloz ve Toraks Dergisi 1996;44(1): 7-11.
9) Ozdemir L, Akkurt I, Sumer H, Cetinkaya S, Gonlugur U, Ozsahin SL, et al. The prevalence of sleep related disorders in Sivas, Turkey. Tüberküloz ve Toraks Dergisi 2005;53:19-26.
10) Guilleminault C, Eldridg FL, Tilkian A, Simmons FB, Dement WC. Sleep apnea syndrome due to upper airway obstruction. Arch Intern Med.1977; 137: 296-300. [ Özet ]
11) He J, Kryger MH, Zorick FJ, Conway W, Roth T. Mortality and apnea index in obstructive sleep apnea. Chest 1988; 94: 9-14. [ Özet ]
12) Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men. Am J Respir Crit Care Med. 1998;157: 144–148. [ Özet ]
13) Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ: Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax, 1999; 54: 323-328. [ Özet ]
14) Hader C, Schroeder A, Hinz M, Micklefield GH, Rasche K. Sleep Disordered breathing in the elderly: Comparison of women and men. J Phys Pharm.2005; 56: 85-91. [ Özet ]
15) Andrews JG, Oei TP. The roles of depression and anxiety in the understanding and treatment of Obstructive Sleep Apnea Syndrome. Clin Psychol Rev 2004; 24: 1031-1049. [ Özet ]
16) Paoli JR, Lauwers F, Lacassagne L, Tiberge M, Dodart L, Boutault F. Craniofacial differences according to the body mass index of patients with obstructive sleep apnoea syndrome: cephalometric study in 85 patients. Br J Oral Maxillofac Surg 2001;39: 40–45. [ Özet ]
17) Lopata M, Onal E. Mass loading sleep apnea and pathogenesis of obesity hypoventilation. Am Rev Respir Dis. 1982;126: 640–645. [ Özet ]
18) Rubinstein I, Colaptino N, Rotstein LE, Brown IG, Hoffstein V. Improvement in upper airway function after weight loss in patients with obstructive sleep apnea. Am Rev Respir Dis. 1988;138:1192–1195. [ Özet ]
19) Deegan PC, McNicholas WT: Predictive value of clinical features for the obstructive sleep apnoea syndrome. Eur Respir J. 1996; 9: 117–124. [ Özet ]
20) Strohl KP, Redline S. Recognition of obstructive sleep apnea. Am J Respir Crit Care Med. 1996;154: 279-289. [ Özet ]
21) Douglas N, Polo O. Pathogenesis of obstructive sleep apnoea/hypopnoea syndrome. Lancet 1994;344: 653-655. [ Özet ]
22) Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurence of sleep disordered breathing among middle aged adults. N Engl J Med 1993;328:1230-1235. [ Özet ]
23) Baiardini I, Braido F, Cauglia S, Canonica GW. Sleep disturbances in allergic diseases Allergy 2006; 61: 1259–1267. [ Özet ]
24) Lindberg E, Berne C, Karl A. Franklin KA, Svensson M, janson C. Snoring and daytime sleepiness as risk factors for hypertension and diabetes in women-A population based study. Respir Med. 2007;101:1283-1290. [ Özet ]
25) Coccagna G, Pollini A, Provini F. Cardiovascular Disorders and Obstructive SleepApnea Syndrome. Clin Exp Hypertens 2006; 28: 217-224. [ Özet ]
26) Braun B, Rock PB, Zamudio S, Wolfel GE, Mazzeo RS, Muza SR, et al. Women at altitude: Short-term exposure to hypoxia and/or alpha1-adrenergic blockade reduces insulin sensitivity. J Appl Physiol 2001; 91: 623–631. [ Özet ]
27) Makino S, Handa H, Suzukawa K, Fujiwara M, Nakamura M, Muraoka S, et al. Obstructive sleep apnoea syndrome, plasma adiponectin levels, and insulin resistance. Clin Endocrinol (Oxf) 2006; 64: 12–19. [ Özet ]
28) Harsch IA, Schahin SP, Radespiel-Troger M, Weintz O, Jahreiss H, Fuchs FS, et al. Continuous positive airway pressure treatment rapidly improves insulin sensitivity in patients with obstructive sleep apnea syndrome. Am J Resp Crit Care Med 2004; 169: 156–162. [ Özet ]
29) Kribbs NB, Pack AI, Kline LR, Getsy JE, Schuett JS, Henry JN, et al. Effects of on night without nasal CPAP treatment on sleep and sleepiness in patients with obstructive sleep apnea. Am Rev Respir Dis 1993;147:1162-1168. [ Özet ]
30) McColley SA, Carroll JL, Curtis S, Loughlin GM, Sampson HA. High prevalence of allergic sensitization in children with habitual snoring and obstructive sleep apnea. Chest, 1997;111: 170–173. [ Özet ]
31) Eitner S, Urschitz MS, Guenther A, Urschitz-Duprat PM, Bohnhorst B, Schlaud M, et al. Sleep problems and daytime somnolence in a German population-based sample of snoring school-aged children J Sleep Res 2007;16: 96-101. [ Özet ]




