FASİYAL SİNİR FELCİ REANİMASYONUNDA STATİK ASKILAMA YÖNTEMİ
2Dışkapı Yıldırım Beyazıt Eğitim ve Araştırma Hastanesi, KBB, Ankara, Türkiye
3Siirt Devlet Hastanesi, KBB, Siirt, Türkiye
Özet
Yüz felci nedeniyle bir çok sorun yaşayan hastaların tedavilerinde bir çok algoritma mevcuttur. Medikal tedaviye cevap vermemiş hastaların tedavilerinde fasyal reanimasyon teknikleri düşünülmelidir. Statik yüz askılama yöntemleri doğru zamanlamayla ve doğru hastaya yapıldığında çok olumlu sonuçlar vaad eder. Çalışmamızda kendi hastamızdan yola çıkarak alternatif statik yüz askılama yöntemlerini derledik ve kendi uyguladığımız yöntemi tarif ettik.Giriş
The facial nerve is responsible for emotional and voluntary facial expression, protection of the eye, lacrimation, oral competence, salivation, taste and sensation. Unfortunately, the facial nerve is the most commonly paralyzed nerve in the human body.[1] Paralysis of the facial nerve is considered to be one of the most devastating of the cranial nerve lesions, due to the clinical, aesthetic and psychological impact it has on patients' lives. The overall effect of facial paralysis on static and dynamic facial appearance, verbal and nonverbal communication, functional issues such as ocular dryness and epiphora, oral incompetence, poor salivation, loss of taste, nasal obstruction, and the resultant impairment in the patient's self-image results in significant global disability, and many patients withdraw from their normal lives. The etiologic factors of facial nerve paralysis are classified under the categories of: birth, neurologic trauma, infection, metabolic, neoplastic, toxic, iatrogenic and idiopathic, and the four most common causes are: trauma, Bell's palsy, iatrogenic, and idiopathic.[2] The history and physical examination are directed to identify the cause and topographic location of the injury as well as the degree of injury. Electromyography (EMG) plays a central role in the evaluation of the patient. EMG allows a prognostic evaluation on the probability of spontaneous healing. Magnetic resonance imaging (MRI) is a preferred method of choice in order to localize a lesion of the facial nerve in the brain stem, the cerebellopontine angle and in the intratemporal course of the nerve. It also helps to determine the mimetic muscle volume and fibrosis. After electrodiagnostic studies and imaging studies have been obtained, the surgeon is faced with decision of when and how to proceed with facial reanimation.While patients present to our clinic in the acute stages of facial nerve paralysis, it is comparatively less common to see or treat a patient in the chronic stages, and therefore, reconstructive surgery of the facial nerve is not considered routine for most head and neck surgeons. The published experiences of strategies to ensure optimal functional results for patients undergoing facial reanimation are based on small case series' with a large variety of surgical techniques. With this background it is worthwhile to develop a standardized approach for diagnosis and treatment of patients asking for facial rehabilitation. In this article, we will discuss the facial reanimation techniques and focus on static suspension.
Surgical Techniques for Facial Reanimation
There are many techniques which have been developed for both facial nerve function and cosmetic deformity restoration. By modifying and combining these techniques, it is possible to achieve successful results with facial reanimation. Facial reanimation techniques generally in the categories of: facial nerve repair and grafting, facial reanimation using cranial nerves, musculofacial transposition (or free muscular transplantation,) static sling techniques, eyelid and muscular positioning procedures, and selective myectomy. The various procedures can be used alone or in tandem with one another depending on the patient and the type of paralysis.[3] Factors which affect which techniques are employed are: the amount of time elapsed post-paralysis, the possibility of nerve regeneration, general physical and mental health, the age, history of radiotherapy, and history of previous surgery. Before constructing a surgical plan, facial paralysis is confirmed, and special attention given to the possibility of spontaneous regeneration considered using electrophysological testing.[4]
Static Facial Suspension
Static facial suspension procedures for those with long-standing paralysis can establish facial symmetry at rest when no viable re-innervation potential exists. It can also be integrated with dynamic procedures such as facial nerve grafting to provide instantaneous restoration of facial symmetry during the postoperative recovery period. Static facial suspension procedures traditionally involve suspension of the mid and lower face with a sling consisting of variable materials. Static facial suspension is usually performed in conjunction with a traditional unilateral face-lift on the paralyzed side for further elevation.[5]
A variety of autologous and alloplastic materials have been used for static facial suspension. They can function as a sling attached from the deep temporalis fascia to the oral commissure without the need for sacrifice of autogenous tissue. Autologous substances (fascia lata and palmaris longus tendon) are immune compatible, but may cause significant donor site morbidity and lead to unpredictable results. Alloplastic materials, such as such as polytetrafluoroethylene (GORE-TEX; W. L. Gore Associates Inc, Flagstaff, Arizona), polypropylene mesh, and silicone rods that tend to form granulomata, are easily stretchable and have a high rate of extrusion and cause wound complications. Numerous studies compare biomechanical properties of different materials used in facial slings to help determine clinical superiority.
Autogenous fascia lata slings have the advantages of superior tensile strength and zero immunological response. In contrast to alloplastic materials autogenous fascia lata is well vascularized and incorporated into the surrounding tissues and closely maintains its pre-surgical length. Lyophilized dried cadaveric fascia, on the other hand, is well integrated but remains structurally weak and yields poor surgical outcomes. As well, acellular dermal grafts (Alloderm; LifeCell Corp, Branchburg, New Jersey), Acellular porcine dermis (Enduragen; Tissue Sciences Laboratories, plc, Aldershot, U.K.) are being used with increasing frequency. The advantages of their availability are without causing additional donor site morbidity, which is seen in autogenous materials and ability to incorporate into the recipient bed with a varying degree of tissue ingrowth and neovascularization.[6] AlloDerm seems to be a more suitable dermal matrix implant than ENDURAGen for cases in which tissue incorporation and neovascularization are sought for the optimal outcome.[7]
Although static suspension slings can recreate definition at the nasolabial fold, they do little to evert the upper lip or to lateralize a collapsed ala to its original preparalyzed position. This is because elevation can be provided only in a flat, 2-dimensional plane. In addition, asymmetry in the length of the upper lip segments is inevitable owing to stretching of the upper lip segment on the paralyzed side by the superior-lateral pull by the static suspension sling. There are complications with this technique of facial suspension as wound problems, healing complications, hematomas, seromas and infections. The most important one is loss of correction.[8]
Aside from the functional problems caused by chronic facial paralysis, taking into consideration the social and psychological affects, we see just how important treatment for facial paralysis is and how much it affects the lives of patients. Regardless of which facial nerve reanimation strategy is used, oculoplastic management of the eyelid is generally employed in patients in common. Oculoplastic management of the paralyzed eye is of paramount importance as exposure keratitis can lead to permanent visual loss. There are variety of alternative methods in repairing of upper eyelid. Eyelid weight placement, palpebral spring procedure, upper eyelid blepharoplasty and lateral tarsorrhaphy. The lower eyelid is managed with the lateral tarsal strip procedure and medial canthopexy. For mid-face asymmetry, external nasal valve repair and nasolabial fold modification can be used as adjunctive treatment procedures.
Our Surgical Technique
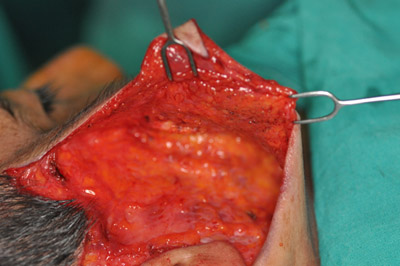
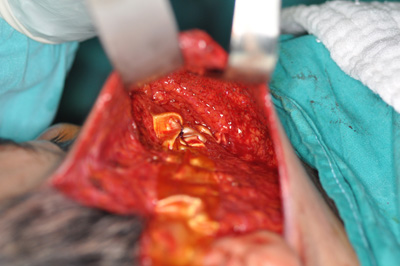
A 42 years old male who had developed Bell's palsy 8 years previously presented to our clinic, and our planned course of action was a static facial suspension using an autologous tensor fascia lata sling. A standard facelift incision was made and subsequent subdermal dissection was performed in the plane above the SMAS until the oral commisure. Subdermal tunnels elevated over the upper and lower lips. (Photo 1) The zygomatic arch was skletonized and two round openings made in the bone. (Photo 2) Fascia lata was harvested from the patients right thigh, and in the interest of creating a thicker layer, was doubled upon itself and sutured for stability. A two cm long horizontal cut made at the distal tip of the fascia to seperate the it into two stripes which were used to fix upper and lower lips deep tissues by sutures through the tunnels elevated previously in the subdermal plane. The corner of the horizontal cut was used to suture oral commissure. (Photo 3) Following that, the fascia lata was stretched to the desired tension and with the help of the openings made earlier, was fixed to the zygomatic arch. (Photo 4) Excess skin and tissue was removed and a drain placed in, completing the procedure. (Photo 5) Postoperative assessment took place 6 months or longer after surgery to ensure that long-term results were assessed. (Photo 6) Evaluation of functional outcome was achieved by patient history.
 Büyütmek İçin Tıklayın |
Photo 1: Subdermal dissection to expose SMAS |
 Büyütmek İçin Tıklayın |
Photo 2: Skeletonization of zygomatic arch |
 Büyütmek İçin Tıklayın |
Photo 3: Orientation of Fascia lata |
 Büyütmek İçin Tıklayın |
Photo 4: Insertion of Fascia lata |
 Büyütmek İçin Tıklayın |
Photo 5: Suspension with Fascia lata |
 Büyütmek İçin Tıklayın |
Photo 6: Pre and post operative photos |
Sonuç
Static facial suspensions are an effective method of correcting facial nerve deficits in cases where nerve repair is not planned or possible. Static suspension procedures address the cosmetic and functional sequelae of facial paralysis. The major goals of facial rehabilitation include corneal protection, oral competence, and restoration of facial symmetry. Reanimation techniques, such as end-to-end anastomosis, interposition grafting, and hypoglossal-facial nerve crossover may improve facial tone and mobility; however, these procedures typically require multiple, lengthy operations to achieve the desired effect. Static techniques may be appropriate for patients who are unable to tolerate dynamic reconstruction. These procedures can provide facial symmetry at rest and oral competence, but have no effect on volitional movement. The use of autogenous fascia for the construction of facial slings is supported by a wide body of literature, and has documented success rates as high as 90% to 95%.These successes are defined by adequate suspension of the oral commissure and, thus, restoration of oral competence and facial symmetry. The drawback of the use of autogenous fascia for this purpose is that a donor site is required, and this generally requires a separate incision and tissue resection, sometimes at a site remote from the recipient site. When considering the confidence, cost, and lack of complications associated with alloplast grafts, it is seen as a viable and preferable choice in facial paralysis treatment.
Kaynaklar
1) Volk F. G, Pantel M, Guntinal-Lichius O. Modern concepts in facial nerve reconstruction.
Head Face Med. 2010; 6: 25.
2) Mehta P. R, Surgical treatment of facial paralysis. Clin Exp Otorhinolaryngol. 2009 March;
2(1): 1-5.
3) Tomat LR, Manktelow RT. Evaluation of a new measurement tool for facial paralysis reconstruction.Plast Reconstr Surg. 2005 Mar;115(3):696-704.
4) Rose E. Autogenous fascia lata grafts: Clinical applications in reanimation of the totally or
partially paralyzed face. Plast. Reconstr. Surg. 116: 20, 2005.
5) Dzwierzynski WW, Sanger JR, Larson DL. Use of Mitek suture anchors in head and neck
reconstruction. Ann Plast Surg. 1997;38(5):449–454.
6) Morgan AS, McIff T, Park DL, et al. Biomechanical properties of materials used in static
facial suspension. Arch Facial Plast Surg 2004;6:308-10.




