TRAINING ON BOTOX APPLICATIONS ON THE FACE MODEL PREPARED USING A 3D PRINTER SIMULATION
Summary
Objective: Society demands competent physicians, and patients do not want to be the object of education, revealing the contradiction between medical service and residential education. Surgical simulators can be introduced to residents and medical students in facial aesthetics before real-life applications. Within the scope of this research, we aimed to elucidate the benefits of simulation Training in botox applications on a 3D-printer model in residency education.Methods: Otorhinolaryngology assistants and medical faculty students (n=30) who have not previously performed botox applications and received surgical training have participated in this prospective observational research. After oral training on botox applications, the application training was given on the face model obtained using a 3D printer (Ender-4 Pro, Creality, Shenzhen, China). Following this, the participants were requested to perform applications on face models. A survey administered before and after the training evaluated whether the participants' practical competencies had increased.
Results: The residents and medical students evaluated within the scope of the study were asked three questions in the pre-test and seven questions in the post-test, and the distribution of pre-test and post-test questions is denoted in Table 1. When the table was examined, a statistically significant difference was achieved between the pre-test and post-test measurements in the first three questions in the Wilcoxon test. Additionally, there was a statistically significant difference between the pre-test and post-test measurement scores (p <0.05).
Conclusion: Regarding the outcomes of this research, the simulated system can be observed in detail by researchers, thus, the use of detailed observations leverages a better understanding, eliminating previously unseen deficiencies and establishing a more effective physical and operational system.
Introduction
The integration of education and technology is one of the undeniable facts today. Although simulation environments have recently been included in education through technology, they are one of the oldest known methods. It is an education in a physical or technological environment developed in medical faculties to increase and facilitate the learning of assistants and students[1]. For this reason, simulation environments are used in training in many fields. Examples of these include combat techniques training given in military schools, troubleshooting training on aircraft models, flight training given to pilots and flight crews, training prepared for motorsports, especially Formula 1, virtual discussion environments created in the field of social sciences, and models in the field of medical training[2].In simulation environments, assistants and students work on a model to discuss an event or problem from different aspects, imitate to analyze the documents they have, perform operations to solve problems, notice errors in operations by testing them, correct them, and complete their tasks. Simulation environments provide the opportunity to study a model education system prepared by and integrated with the curriculum or through various educational projects for a certain period and to evaluate the results. For this reason, it should start from a simple to a complex structure. The testing phase of the applied model should be completed and suitable for development and updating according to needs[3].
The fact that society wants competent physicians and patients do not want to be the object of education reveals the contradiction between medical service and education. Simulation-based medical education applications are one of the most innovative techniques that can solve this situation. Performing professional practices on the patient first stresses assistants and students for many reasons. The primary reasons are worrying about making mistakes and fear of harming the patient. Other reasons include being unable to try again on the patient, being unable to learn due to lack of supervision, and not feeling competent[4]. Training on actual patients is a short, opportunistic educational experience and learning that varies according to interest. This situation causes learning to occur in a difficult, incomplete, feedback-free, and unsafe environment. It is one of the good examples of the application areas of simulation-based learning. It allows the patient to gain experience by repeating, making mistakes, and learning from their mistakes without harming the patient. Scenarios can be prepared as desired, and all possible situations can be tested. The use of simulation helps reverse all these negativities. Regarding aesthetic applications, the patient's concerns come to the fore and increase excessively[5].
Simulation-based education brings prestige to the institution. This innovative initiative is an indicator of continuous improvement efforts to increase the training program and the service quality of the institution. It will be seen as an institutional structure that respects and cares about patient autonomy, considers ethical practices, and reflects this in its educational philosophy. From a broad perspective, it will be an institution that provides quality assurance, is insured against malpractice, and allows new medical tools and technologies to enter the medical environment with its structured and safe stance. Simulation-based education is also important in ensuring the effective distribution of resources based on social justice[6].
Surgical simulators can be introduced to residents and medical students in facial aesthetics before real-life applications. Within the scope of this research, we aimed to elucidate the benefits of simulation Training in botox applications on a 3D-printer model in residency education.
Methods
Otorhinolaryngology assistants and University Of Health Sciences Faculty of Medicine students (n=30) who have not previously performed botox applications and have not received surgical training have participated in this prospective observational research. After oral training on botox applications, botox application training was given on the face model obtained using a 3D printer (Ender-4 Pro, Creality, Shenzhen, China). Following this, the participants were requested to perform applications on face models. Physiological saline was used as liquid material during application. A survey administered before and after the training evaluated whether the participants' practical competencies had increased.Before and after using the 3D simulator, participants were asked to objectively evaluate the following parameters as yes or no for themselves;
• Knows the steps of Botox application,
• Knows where to apply Botox on the face,
• Is confident about the procedure,
• Can apply as medical treatment,
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Ethics committee approval was granted from our institution on 27/03/2023 with protocol number 451, and informed consent has been obtained from all participants.
Statistical Analysis
Patient data collected within the scope of the study were analyzed with the IBM Statistical Package for the Social Sciences (SPSS) for Windows 26.0 (IBM Corp., Armonk, NY) package program. Frequency and percentage for categorical data and mean and standard deviation for continuous data were given as descriptive values. For comparisons between groups, the "Independent Sample T-test" was used for two groups, and the "Pearson Chi-Square Test" was used to compare categorical variables. The results were considered statistically significant when the p-value was less than 0.05.
Results
The residents and medical students (n=30) evaluated within the scope of the study were asked three questions in the pre-test and seven questions in the post-test, and the distribution of pre-test and post-test questions is denoted in Table 1. When the table was examined, a statistically significant difference was achieved between the pre-test and post-test measurements in the first three questions in the Wilcoxon test. Additionally, there was a statistically significant difference between the pre-test and post-test measurement scores (p <0.05).Table 1: Distribution of Pre-test and Post-test Evaluation Results
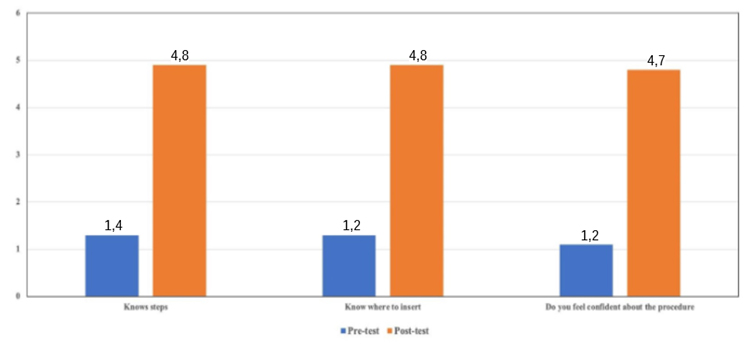
Regarding the responses of residents and medical students on three specific questions about the application methodology, there was a significant improvement (p<0.001). The participants admitted that they learned the procedural steps and where to make the injection (p<0.001). Additionally, after the simulation training, they felt more competitive about the application (p<0.001).
 Büyütmek İçin Tıklayın |
Figure 1: The participants admitted that they learned the procedural steps and where to make the injection (p<0.001). Additionally, after the simulation training, they felt more competitive about the application (p<0.001). |
Discussion
The requirement for practicing procedures outside of the operating room and the role of simulation in filling this gap has been increasingly recognized in today"s surgical training paradigm. The benefits of surgical simulation include educational, safety, cost, and outcome-based benefits. Three-dimensional (3D) printing allows for the rapid development and production of task trainers to create accessible training opportunities, an ideal complement to the traditional surgical training model. Rhinoplasty is an extremely common and complex operation requiring thorough anatomy knowledge and necessary technical skills[7].Many benefits of simulation-based applications, whose use is increasing day by day in the world and our country, are mentioned in the literature. A meta-analysis by Oh et al. revealed that standardized patient use statistically significantly affected nursing students' knowledge acquisition, communication skills, self-efficacy, motivation to learn, and clinical competence. Their study also stated that it benefits cognitive, affective, and psychomotor learning[8]. The literature has stated that the communication skills, self-confidence, and satisfaction of students who practice with standard patients increase, their critical thinking skills improve, and their level of application of patient safety principles also improves[9].
It is stated in the literature that the analysis session held after the simulation application is very important in simulation-based education. Rall et al. state that the debriefing session is the "heart and soul" of simulation training[10]. After the simulation application, the trainer conducts the debriefing session, where the participants' performances are discussed, feedback is given, and reflective thinking is encouraged[11]. The main purpose of this session is to ensure that students' next performance is improved. In the debriefing session, learning is reinforced by ensuring that the correctness and mistakes made by the students in the applications are seen by themselves. Learning can occur in simulation applications, but effective learning is only possible with a debriefing session[11].
In the study conducted by Savoldelli et al. with 42 anesthesia assistants, Verbal feedback was given to the first group, verbal analysis was given to the second group, and a video verbal analysis session was given to the third group. While participants in both analysis groups significantly increased performance scores compared to the group without analysis, no significant difference could be detected between the groups with analysis. Researchers stated that both debriefing sessions were effective and debriefing sessions could also be done without video[12]. In another study by Sawyer et al. on neonatal resuscitation, two analysis methods were compared, and no difference was found between video and verbal analysis[13]. Similar results were found in Reed's study, in which he compared the video and verbal debriefing sessions after intensive care simulation with 64 medical students[14].
Lee et al. used a model ear canal that allowed students to practice with otoscopes to view normal and pathologic images of the external and middle ear. Over 90% of the student respondents agreed that the simulation improved their confidence in otoscopy[15]. Morris et al. found that students could identify effusions with significantly higher accuracy than classmates who did not practice with an ear trainer[16]. The use of 3D printed models allows the use of actual surgical instruments, enhancing the procedural simulations' fidelity[17].
The data from the study of Sparks et al. elaborated that first and 2nd-year medical students with minimal prior exposure to otolaryngology ear anatomy or surgical training had improved self-assessment scores in anatomical knowledge and the procedure steps after practice with a 3D-printed simulator. As such, the students gained early exposure to using instruments, anatomy, and procedural basis for a surgical subspecialty[18]. McAnena et al. found that residents who had taken part in surgical skills modules as medical students had significantly higher technical skills than interns who had not[19]. Yet technical training remains a known challenge, with 28% of senior and 87% of junior residents feeling insufficiently exposed to rhinoplasty during residency with nasal osteotomy as the technique they were least confident performing[20].
Using 3D-printed surgical models for simulation training residents and fellows in pediatric otolaryngology has improved self-reported confidence and expertise in the associated practice. The American Academy of Otolaryngology-Head and Neck Surgery Foundation formed the 3D-Printed Temporal Bone Working Group as a collaborative effort to evaluate 3D-printed ear models for appropriateness of microscopic surgery simulation with reported success[21].
Conclusion
The field of otolaryngology has developed a reputation for being extremely competitive, which can be an intimidating factor for residents considering the field. Regarding the outcomes of this research, the simulated system can be observed in detail by researchers, thus, the use of detailed observations leverages a better understanding, eliminating previously unseen deficiencies and establishing a more effective physical and operational system.
Acknowledgments
Funding
There is no specific funding related to this research.
Competing interests
The authors declare that they have no competing interests.
Ethical Declaration
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Ethics committee approval has been granted from our institution.
Reference
1) Standiford TC, Eltawil Y, Durr ML, Pletcher SD, Chang JL. Leadership Training Curriculum for Otolaryngology-Head and Neck Surgery Residents: A Scoping Review. Otolaryngol Head Neck Surg. 2023 Aug 9. doi: 10.1002/ohn.478. Epub ahead of print. [ Özet ]
2) McInerney N, Nally D, Khan MF, Heneghan H, Cahill RA. Performance effects of simulation training for medical students - a systematic review. GMS J Med Educ. 2022 Nov 15;39(5):Doc51. doi: 10.3205/zma001572. [ Özet ]; PMCID: PMC9733478.
3) Hogan CJ, Winters R. The Current Role of Medical Simulation in Otolaryngology. 2023 Jan 30. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [ Özet ]
4) Jegatheeswaran L, Naing TKP, Choi B, Collins R, Luke L, Gokani S, Kulkarni S. Simulation-based teaching: an effective modality for providing UK foundation doctors with core ENT skills training. J Laryngol Otol. 2023 Jun;137(6):622-628. doi: 10.1017/S0022215122001712. Epub 2022 Aug 1. [ Özet ]
5) Schlegel L, Malani E, Belko S, Kumar A, Barbarite E, Krein H, Heffelfinger R, Hutchinson M, Pugliese R. Design, printing optimization, and material testing of a 3D-printed nasal osteotomy task trainer. 3D Print Med. 2023 Jul 13;9(1):20. doi: 10.1186/s41205-023-00185-9. Erratum in: 3D Print Med. 2023 Aug 21;9(1):23. [ Özet ]; PMCID: PMC10339601.
6) Gray T, Boccardi A, Shahwan KT. Simulation-based training in dermatologic surgery: a literature review. Arch Dermatol Res. 2023 Oct;315(8):2227-2232. doi: 10.1007/s00403-023-02606-5. Epub 2023 Apr 6. [ Özet ]
7) Schlegel L, Malani E, Belko S, Kumar A, Barbarite E, Krein H, Heffelfinger R, Hutchinson M, Pugliese R. Design, printing optimization, and material testing of a 3D-printed nasal osteotomy task trainer. 3D Print Med. 2023 Jul 13;9(1):20. doi: 10.1186/s41205-023-00185-9. Erratum in: 3D Print Med. 2023 Aug 21;9(1):23. [ Özet ]; PMCID: PMC10339601.
8) Oh PJ, Jeon KD, Koh MS. The effects of simulation-based learning using standardized patients in nursing students: A meta-analysis. Nurse Educ Today. 2015 May;35(5): e6-e15. doi: 10.1016/j.nedt.2015.01.019. Epub 2015 Feb 2. [ Özet ]
9) Ha EH. Experience of nursing students with standardized patients in simulation-based learning: Q-methodology study. Nurse Educ Today. 2018 Jul; 66: 123-129. doi: 10.1016/j.nedt.2018.04.023. Epub 2018 Apr 23. [ Özet ]
10) Rall M, Manser T, Howard S. Key elements of debriefing for simulator training. Eur J Anaesthesiol. 2000; 17(8): 516-517.
11) Fanning RM, Gaba DM. The role of debriefing in simulation-based learning. Simul Healthc. 2007 Summer;2(2):115-25. doi: 10.1097/SIH.0b013e3180315539. [ Özet ]
12) Savoldelli GL, Naik VN, Park J, Joo HS, Chow R, Hamstra SJ. Value of debriefing during simulated crisis management: oral versus video-assisted oral feedback. Anesthesiology. 2006 Aug;105(2):279-85. doi: 10.1097/00000542-200608000-00010. [ Özet ]
13) Sawyer T, Sierocka-Castaneda A, Chan D, Berg B, Lustik M, Thompson M. The effectiveness of video-assisted debriefing versus oral debriefing alone at improving neonatal resuscitation performance: a randomized trial. Simul Healthc. 2012 Aug;7(4):213-21. doi: 10.1097/SIH.0b013e3182578eae. [ Özet ]
14) Reed SJ, Andrews CM, Ravert P. "Debriefing simulations: Comparison of debriefing with video and debriefing alone." Clinic Simul Nurs. 2013; 9(12): e585-e591.
15) Lee DJ, Fu TS, Carrillo B, Campisi P, Forte V, Chiodo A. Evaluation of an otoscopy simulator to teach otoscopy and normative anatomy to first year medical students. Laryngoscope. 2015 Sep;125(9):2159-62. doi: 10.1002/lary.25135. Epub 2015 Jan 19. [ Özet ]
16) Morris E, Kesser BW, Peirce-Cottler S, Keeley M. Development and validation of a novel ear simulator to teach pneumatic otoscopy. Simul Healthc. 2012 Feb;7(1):22-6. doi: 10.1097/SIH.0b013e31822eac39. [ Özet ]
17) VanKoevering KK, Malloy KM. Emerging Role of Three-Dimensional Printing in Simulation in Otolaryngology. Otolaryngol Clin North Am. 2017 Oct;50(5):947-958. doi: 10.1016/j.otc.2017.05.006. Epub 2017 Aug 31. [ Özet ]
18) Sparks D, Kavanagh KR, Vargas JA, Valdez TA. 3D printed myringotomy and tube simulation as an introduction to otolaryngology for medical students. Int J Pediatr Otorhinolaryngol. 2020 Jan; 128:109730. doi: 10.1016/j.ijporl.2019.109730. Epub 2019 Oct 15. [ Özet ]
19) McAnena PF, O'Halloran N, Moloney BM, Courtney D, Waldron RM, Flaherty G, Kerin MJ. Undergraduate basic surgical skills education: impact on attitudes to a career in surgery and surgical skills acquisition. Ir J Med Sci. 2018 May;187(2):479-484. doi: 10.1007/s11845-017-1696-7. Epub 2017 Oct 17. [ Özet ]
20) Zammit D, Ponnudurai N, Safran T, Gilardino M. Reevaluating the Current Model of Rhinoplasty Training and Future Directions: A Role for Focused Maneuver-Specific Simulation. Plast Reconstr Surg. 2019;144(4): 597e-605e.
21) Mowry SE, Jabbour N, Rose AS, Wiet GJ, Svrakic M, Zopf DA, Vankoevering K, Powell A, Freiser ME, Hochman J, Smith R. Multi-institutional Comparison of Temporal Bone Models: A Collaboration of the AAO-HNSF 3D-Printed Temporal Bone Working Group. Otolaryngol Head Neck Surg. 2021 May;164(5):1077-1084. doi: 10.1177/0194599820960474. Epub 2020 Oct 6. [ Özet ]




