EVALUATION OF THE EFFECT OF ADENOTONSILLECTOMY ON EMOTIONAL AND BEHAVIORAL PROBLEMS IN CHILDREN
2Sivas Cumhuriyet Üniversitesi Tıp Fakültesi, Çocuk ve Ergen Piskiyatrisi Anabilim Dalı, Sivas, Turkey
Summary
Objective: The aim of this study is to evaluate the effect of tonsillectomy and/or adenoidectomy (T&A) applied to children and adolescents with adenotonsillar hypertrophy (ATH) on externalizing and internalizing problems.Material and Methods: Physical and psychiatric symptoms that may be associated with ATH were evaluated with a questionnaire created by the researchers twice, before T&A surgery and at the 3rd month after surgery. Physical symptoms included the loss of appetite, snoring, and excessive daytime sleepiness. Psychiatric symptoms were enuresis (5 years and above), difficulty falling asleep, sleep talking, teeth grinding, difficulty waking up in the morning, hyperactivity, irritability and anger, damaging property, belligerent behavior, anxious mood, being tearful or sad, tics, attention deficit and concentration problems, language, speech and communication problems.
Results: In the preoperative evaluation of symptoms that may be related to ATH, the most frequently reported physical symptom was the loss of appetite, while the most common psychiatric symptom was attention deficit and concentration problems. In postoperative evaluation, the symptoms showing the highest recovery rates were snoring and excessive daytime sleepiness. In addition, recovery rates for physical symptoms were higher than those for psychiatric symptoms.
Conclusion: This study indicated that T&A has a curative effect on many psychiatric symptoms, especially snoring and excessive daytime sleepiness, seen in children with ATH. Still, further longitudinal studies are needed to confirm our findings to draw firm conclusions.
Introduction
Adenotonsillar hypertrophy (ATH) is the most common cause of chronic airway obstruction in childhood[1]. The obstructive complaints caused by ATH are dependent on the extent of choanal and oropharyngeal occlusion rather than the size of the adenoid and tonsil tissue. In particular, chronic ATH and related symptoms have been shown to affect children"s development, behavior, and mood[2]. Chronic ATH is known to cause sleep disorders ranging from loud snoring to severe obstructive sleep apnea (OSA), which are all collected under the umbrella term of sleep-disordered breathing (SDB)[3]. SDB is a common condition that has serious physical, developmental, cognitive, emotional, and behavioral consequences in childhood and is included in the indications for tonsillectomy and/or adenoidectomy (T&A) surgery. Nocturnal symptoms associated with SDB include snoring, witnessed apnea, sialorrhea, restless sleep, and enuresis. Daytime symptoms consist of behavioral problems such as hyperactivity, attention deficit, anxiety, depressed mood, excessive sleepiness, irritability, and aggression. In addition, SDB has been associated with multisystemic diseases (such as obesity, cor pulmonale, heart failure, hypertension, and hormonal imbalance) and growth retardation[4]. Developmental delays were reported in 27% to 62% of pediatric patients OSA and behavioral problems in 40% of children with SDB[5]. Untreated SDB has been shown to negatively impact the emotional, behavioral, and cognitive functions of both children and their families[6,7]. Moreover, the treatment of chronic ATH was found to have a mitigating effect on psychopathologies such as attention-deficit hyperactivity disorder (ADHD), enuresis, and behavioral disorders [2,8-11]. However, few studies have investigated the effect of T&A on the most frequently reported psychopathologies in children with ATH[2,8-12]. In addition, studies in this field have focused more on externalizing problems, including aggression, anger, oppositionality, hyperactivity, and attention deficit, and internalizing problems such as anxiety and depressive state have been relatively neglected[2,9-12].Therefore, this study aimed to determine the effect of T&A on psychiatric problems in children and adolescents with ATH, including emotional and internalizing problems.Methods
This prospective study was conducted with children 51-78 months of age who presented to an otolaryngology clinic with symptoms such as nasal congestion, sleeping with the mouth open, snoring, and frequent tonsillitis for more than 3 months; had physical and endoscopic examination findings of ATH that narrowed the airway passage by at least 50%; and underwent T&A surgery. The prevalence of children included in this study was taken as 2.1% (p) according to the study conducted by Polat C. et al. based on the calculation of sample size determination according to prevalence in cases where the universe is unknown, the study's power was calculated to be 97.7% according to the frequency of occurrence used as a reference in the study. In the calculations performed, ? was taken as 0.05. The applied sample size formula is provided below[13].
Tonsil hypertrophy was graded using a standard Brodsky scale from 0 to +4, where 0 indicates the surgically induced absence of tonsil tissue and +4 indicates that the tonsils extend to the midline (also called kissing tonsils). Patients with +3 and +4 hypertrophy were included in this study. Flexible endoscopic examinations were performed by one otorhinolaryngologist doctor with 14 years of experience using the Karl Storz Tele Pack endoscopic system before surgery. Adenoid size was assessed as in the study conducted by Zwiers et al. Patients with grade 2 and 3 adenoid hypertrophy were included in our study. Grade I corresponds to adenoid tissue occupying less than one-third of the vertical extent of the choanae. Grade II indicates adenoid tissue occupying between one-third and two-thirds of the choanae, and Grade III signifies adenoid tissue filling more than two-thirds of the choanae[14]. Exclusion criteria were the presence of concomitant sinonasal disease, active upper respiratory tract infection, allergic rhinitis, asthma, history of previous otorhinolaryngologic surgery, and craniofacial anomaly.
Of 203 patients initially enrolled, the study was conducted with 151 children and adolescents after excluding those who did not meet the study inclusion criteria and those who did not consent to participate or did not attend follow-up. After the study procedure was explained in detail to the children who met the eligibility criteria and their parents, verbal consent was obtained from the children participating in the study and verbal and written consent was obtained from the parents. The study was approved by the local ethics committee (date: 15.01.2020, no: 2020-01/15) and conducted in accordance with the Good Clinical Practice procedures and the current version of the Declaration of Helsinki.
Procedure
All patients participating in the study were evaluated twice by a qualified child and adolescent psychiatrist, once before and again 3 months after T&A. In these assessments, the preoperative presence of any psychiatric symptoms that may be associated with ATH and the improvement/resolution or persistence of these symptoms at postoperative 3 months were noted. In this study, based on literature data[2,6-8,11,15-18], we categorized the symptoms that may be associated with ATH into two types: physical and psychiatric symptoms. The physical symptom was the loss of appetite, and the psychiatric symptoms were enuresis (5 years and older), difficulty in falling asleep, snoring, talking in sleep, teeth grinding, excessive daytime sleepiness, difficulty in waking up in the morning, hyperactivity, irritability and anger, damaging things, belligerent behaviors, anxious mood, being tearful or sad, tics, attention deficit and concentration problems, language, speech and communication problems. Sociodemographic information and clinical data such as drugs used, history of systemic disease and allergy, and ATH characteristics were collected using a questionnaire created by the researchers.
Statistical Analysis
IBM SPSS version 23.0 (IBM Corp., Armonk, NY) software was used to evaluate the data obtained in the study. After necessary corrections, demographic data were summarized in a descriptive statistics and frequency table. The patients" pre- and postoperative values were compared using McNemar test. In addition, differences in categorical variables were analyzed using chi-square analysis. All results were interpreted at a 95% confidence level. A p value of <0.05 was considered statistically significant for all tests.
Results
Of the 151 patients who participated in the study, 59.6% (n=90) were male and 40.4% (n=61) were female. The mean age was 61.91±6.79 months and the mean age at surgery was 55.31±6.15 months (range: 48-67 months). Area of residence was urban for 61.6% (n=93) and rural for 38.4% (n=58) of the participants. Family income level was minimum wage or below for 49.7% (n=75) and above minimum wage for 50.3% (n=76) of the participants.In the preoperative assessment of psychiatric symptoms possibly associated with ATH, the most commonly reported symptom was lack or loss of appetite for food (68.2%), followed by attention deficit and concentration problems (59.6%), difficulty falling asleep (51.7%), snoring (51.7%), and hyperactivity (47%). The distribution of all preoperative psychiatric symptoms that may be associated with ATH is presented in Table 1.
Analysis of the distribution of preoperative psychiatric symptoms by sex showed that loss of appetite, anxious mood, being tearful or sad, and language, speech, and communication problems were significantly more frequent in girls than boys, whereas attention deficit and concentration problems, difficulty falling asleep, snoring, hyperactivity, irritability and anger, difficult waking up in the morning, enuresis, excessive daytime sleepiness, belligerent behaviors, damaging things, and tics were significantly more frequent in boys than girls. There was no significant difference between the sexes in terms of the prevalence of sleep talking or teeth grinding (bruxism). The distribution of preoperative psychiatric symptoms by sex is shown in Table 2.
Table 2: Distribution of preoperative psychiatric symptoms by sex
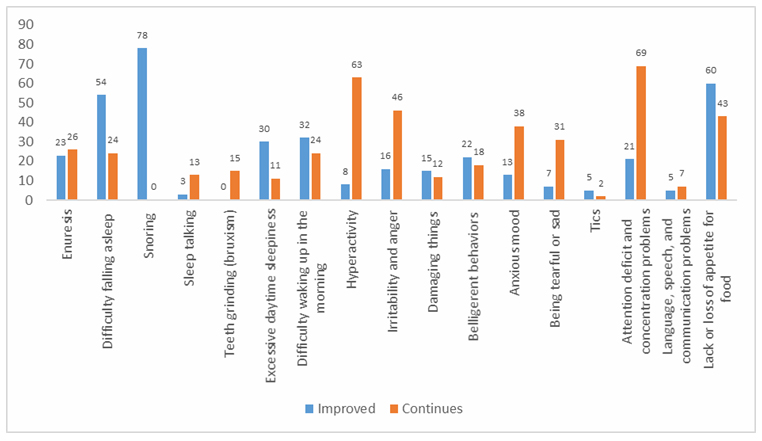
In the postoperative evaluation of psychiatric symptoms that may be associated with ATH, the symptoms with the greatest improvement were snoring (100%) and excessive daytime sleepiness (73.2%). The rate of postoperative improvement was also over 50% for tics, difficulty falling asleep, lack or loss of appetite for food, difficulty waking up in the morning, damaging things, and belligerent behaviors. Rates of improvement/resolution and persistence of all psychiatric symptoms that may be associated with ATH are shown in Table 3 and Figure 1.
 Büyütmek İçin Tıklayın |
Figure 1: Postoperative status of psychiatric symptoms that may be associated with adenotonsillar hypertrophy |
Discussion
This study examined the effect of the surgical treatment of ATH on psychiatric symptoms that may be related to ATH in children, and our results show that T&A was associated with improvement in both internalizing and externalizing symptoms.The lymphoid tissue of the upper respiratory tract increases from birth to about 14 years of age[19]. At the same time, there is a gradual increase in the size of the skeletal borders of the upper respiratory tract. However, between the ages of 5 and 7 years, hypertrophic tonsils and adenoids can reach their maximum size in proportion to the lower airway, resulting in a relatively narrow upper airway[20]. After T&A, significant improvement was reported in the symptoms of sleeping with the mouth open and snoring, which are obstructive symptoms secondary to ATH.
Beyond the physical health effects of ATH-related SDB on the child, authors have also emphasized that it has negative effects on mental health and may be an important psychosocial stressor for children and their families[21]. When we evaluated psychiatric symptoms that may be associated with ATH in children before they underwent T&A, lack or loss of appetite for food, attention deficit and concentration problems, difficulty falling asleep, and hyperactivity were reported at high rates. Moreover, at least a quarter of the patients had symptoms of irritability and anger, difficulty waking up in the morning, anxious mood, enuresis, excessive daytime sleepiness, belligerent behaviors, and being tearful or sad. Our findings are consistent with findings of improvements in sleep-related quality of life and behavioral problems in children with obstructive sleep apnea (OSA) in long-term follow-up after T&A in children with ATH[12]. We also noted that the preoperative prevalence of some psychiatric symptoms differed significantly between the sexes. Girls were more often reported to have loss of appetite, anxious mood, being tearful or sad, and language, speech, and communication problems, while boys were more likely to exhibit attention deficit and concentration problems, difficulty falling asleep, snoring, hyperactivity, irritability and anger, difficulty waking up in the morning, enuresis, excessive daytime sleepiness, belligerent behaviors, damaging things, and tics. Only the symptoms of sleep talking and bruxism showed no sex-based difference. Rosemary et al. did not detect significant sex differences in the severity or outcomes of SDB in children, but noted that girls exhibited more internalizing behavior problems, especially in the older age group. Our findings suggest that sex differences may be significant in terms of the impact on behavior and executive function after T&A in children with ATH[22].
At postoperative 3 months, the symptoms with the greatest improvement were snoring (100% of patients) and excessive daytime sleepiness (73.2% of patients). The proportion of patients with postoperative improvement was also over 50% for tics, difficulty falling asleep, lack or loss of appetite for food, difficult waking up in the morning, damaging things, and belligerent behaviors. These results suggest that the surgical treatment of ATH contributes favorably not only to physical health but also mental health and can help alleviate both internalizing and externalizing problems. Improvement in psychiatric symptoms should also lead to an increase in quality of life. Previous studies have also demonstrated significant improvements in emotional symptoms, behavioral problems, hyperactivity/attention deficit, peer relationship problems, and prosocial behavior after T&A, consistent with our results[2,8-11].
The relationship between ATH and anorexia and growth retardation has often been emphasized in previous research, with a focus on the role of leptin and ghrelin in this relationship[23]. Leptin is a hormone produced by adipocytes that reduces appetite[24]. Ghrelin is secreted by the intestines and increases appetite[25]. In children with ATH, serum leptin levels were found to be lower compared to a normal control group, while there was no difference in ghrelin levels. In addition, it has been speculated that serum leptin would be lower in children with ATH because they have less adipose tissue and leptin is synthesized and released from adipose cells[23]. In addition, it has been emphasized that other possible causes of loss of appetite seen in these children may include impaired retropharyngeal odor perception during eating, chronic infection, or pain during swallowing due to adenotonsillar hypertrophy[10,20,26]. There are also studies showing that T&A has positive effects on appetite and growth[27]. Our findings support these studies, as reduction/resolution of anorexia was reported in 60 of 103 patients (58.3%) after T&A.
In addition to complaints of anorexia, a report from the American Academy of Pediatrics indicated that children with OSA had approximately 3-fold higher rates of emotional and behavioral problems such as hyperactivity, inattention, irritability, restlessness, belligerent behaviors, unhappiness, worried/fearful/anxious state, and somatic problems[28]. Chronic ATH may lie at the root of emotional, neurocognitive, and behavioral problems by causing SDB and the associated recurrent sleep interruptions, arousal episodes, and subsequent daytime sleepiness. Although its pathophysiology has not yet been fully elucidated, it is thought that behavioral problems and impaired neurocognitive performance may occur as a result of neurochemical changes in certain areas of the brain due to intermittent or chronic hypoxia associated with sleep disruption[15]. In addition, oxidative stress and inflammatory mechanisms and neurochemical changes related to the hippocampus and prefrontal lobe have also been reported to play a role in the pathogenesis[16]. In contrast, many studies have supported the favorable impact of T&A on these emotional and behavioral problems[10]. Consistent with previous studies, we found that T&A was associated with the improvement or regression of many psychiatric complaints that may be associated with ATH.
Besides the relationship between ATH and emotional and behavioral psychiatric symptoms, it has been emphasized that ATH also shows high comorbidity with nocturnal enuresis, and ATH-related sleep disturbances play a role in this association[17]. In this study, nocturnal enuresis was reported in 32.5% of children with ATH preoperatively and improved postoperatively in nearly half of those children (46.9%). Our findings of improved nocturnal enuresis following T&A are consistent with those of other studies examining the relationship between ATH and nocturnal enuresis[18].
Strengths of this study include its prospective design and relatively large sample size. However, it has certain limitations. Firstly, cross-sectional research does not allow for generalization of the results or definitive determination of causality. Secondly, the children"s symptoms were evaluated based on subjective reporting by parents, with no objective assessment of their sleep or behavior. Longitudinal prospective studies that include a much larger sample size and address this limitation of our study would provide extremely valuable data.
Conclusion
In this study, we determined that psychiatric symptoms that may be associated with ATH were common among children with ATH before undergoing T&A surgery, especially lack or loss of appetite for food, attention deficit and concentration problems, difficulty falling asleep, and hyperactivity. Emotional and behavioral problems such as irritability and anger, difficulty waking up in the morning, anxious mood, enuresis, excessive daytime sleepiness, belligerent behaviors, and being tearful or sad were also fairly common. Improvements in most psychiatric symptoms were reported at postoperative 3 months, suggesting that undergoing T&A for ATH has a favorable impact on both physical and mental health and can help mitigate both internalizing and externalizing problems. Improvement in psychiatric symptoms should also lead to an increase in quality of life. However, further research is needed to replicate, expand, clarify, and validate these findings before definitive conclusions can be reached.Reference
1) Erakman NI, Ataş C, Güven G. Adenoid Hypertrophy in Children: Etiology, Symptoms and Current Overview of Dentofacial/Orthodontic Treatments. HRU International Journal of Dentistry and Oral Research. 2022;2(3):162-169.
2) Türkoğlu S, Tahsin Somuk B, Sapmaz E, Bilgiç A. Effect of adenotonsillectomy on sleep problems, attention deficit hyperactivity disorder symptoms, and quality of life of children with adenotonsillar hypertrophy and sleep-disordered breathing. Int J Psychiatry Med. 2019;54(3):231-241. doi: 10.1177/0091217419829988. [ Özet ]
3) Di Filippo P, Orlandi G, Neri G, Di Pillo S, Chiarelli F, Rossi N, Attanasi M. Effect of tonsillectomy in a child with obesity and obstructive sleep apnea: A case report and review of the literature. Front Pediatr. 2023;10:1101267. doi: 10.3389/fped.2022.1101267. [ Özet ]
4) Marcus CL. Sleep-disordered breathing in children. Am J Respir Crit Care Med. 2001;164(1):16-30. doi: 10.1164/ajrccm.164.1.2008171. [ Özet ]
5) Caixeta JAS, Sampaio JCS, Costa VV, Silveira IMBD, Oliveira CRF, Caixeta LCAS, Avelino MAG. Long-term Impact of Adenotonsillectomy on the Quality of Life of Children with Sleep-disordered breathing. Int Arch Otorhinolaryngol. 2021;25(1):e123-e128. doi: 10.1055/s-0040-1709195. [ Özet ]
6) Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep. 2006;29(9):1115-34. doi: 10.1093/sleep/29.9.1115. [ Özet ]
7) Blunden S, Lushington K, Kennedy D, Martin J, Dawson D. Behavior and neurocognitive performance in children aged 5-10 years who snore compared to controls. J Clin Exp Neuropsychol. 2000;22(5):554-68. doi: 10.1076/1380-3395(200010)22:5;1-9;FT554. [ Özet ]
8) Ali NJ, Pitson D, Stradling JR. Sleep disordered breathing: effects of adenotonsillectomy on behaviour and psychological functioning. Eur J Pediatr. 1996;155(1):56-62. doi: 10.1007/BF02115629. [ Özet ]
9) Derakhshanpour F, Eslami M, Kashani L, Asani M. Effect of adenotonsillectomy on the symptoms of attention deficit hyperactivity disorder in children with adenotonsillar hypertrophy. J Gorgan Univ Med Sci 2021, 23(2): 46-50. URL: http://goums.ac.ir/journal/article-1-3747-en.html
10) Sizer B, Akdağ M, Sizer E, Yılmaz Ü, Demir S. Evaluation of symptoms of preopoperative and postoperative psychosomatic screening in children with adenoidectomy and adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2020;134:110072. doi: 10.1016/j.ijporl.2020.110072. [ Özet ]
11) Soylu E, Soylu N, Yıldırım YS, Sakallıoğlu Ö, Polat C, Orhan I. Psychiatric disorders and symptoms severity in patients with adenotonsillar hypertrophy before and after adenotonsillectomy. Int J Pediatr Otorhinolaryngol. 2013;77(10):1775-81. doi: 10.1016/j.ijporl.2013.08.020. [ Özet ]
12) Song IS, Hong SN, Joo JW, Han MS, Hwang SJ, Seo MY, Lee SH. Long-term results of sleep-related quality-of-life and behavioral problems after adenotonsillectomy. Laryngoscope. 2020;130(2):546-550. doi: 10.1002/lary.27951. [ Özet ]
13) Polat C. , Demirören K. Frequency of the tonsillectomy and adenoidectomy in children in Elazig province, in the east of Turkey. Dicle Tıp Dergisi. 2010; 37(3): 263-266
14) Zwierz A, Masna K, Zwierz K, Bojkowski M, Burduk P. Impact of Isolation on Adenoid Size and Symptoms in Preschool Children Who Previously Qualified for Adenoidectomy: A Case-Control Study. Ear Nose Throat J. 2023;102(7):NP358-NP363. doi: 10.1177/01455613211010085. [ Özet ]
15) Bucks RS, Olaithe M, Eastwood P. Neurocognitive function in obstructive sleep apnoea: a meta-review. Respirology. 2013;18(1):61-70. doi: 10.1111/j.1440-1843.2012.02255.x. [ Özet ]
16) Owens JA. Neurocognitive and behavioral impact of sleep disordered breathing in children. Pediatr Pulmonol. 2009;44(5):417-22. doi: 10.1002/ppul.20981. [ Özet ]
17) Uzun Çiçek A, Bora A, Altuntaş E. Adenoid hypertrophy and nocturnal enuresis are associated with sleep disturbances. ENT Updates. 2020;10(2): 311-320. doi: 10.32448/ entupdates.729178
18) Snow A, Vazifedan T, Baldassari CM. Evaluation of Nocturnal Enuresis After Adenotonsillectomy in Children With Obstructive Sleep Apnea: A Secondary Analysis of a Randomized Clinical Trial. JAMA Otolaryngol Head Neck Surg. 2021;147(10):887-892. doi: 10.1001/jamaoto.2021.2303. [ Özet ]
19) Dhanuka A, Mahajan A, Gupta K, Mahajan S. Evolution of Adenoid Surgery. Tonsils and Adenoids. IntechOpen; 2023. doi: 10.5772/intechopen.1001462.
20) Di Cicco M, Kantar A, Masini B, Nuzzi G, Ragazzo V, Peroni D. Structural and functional development in airways throughout childhood: Children are not small adults. Pediatr Pulmonol. 2021;56(1):240-251. doi: 10.1002/ppul.25169. [ Özet ]
21) Bhargava S. Diagnosis and management of common sleep problems in children. Pediatr Rev. 2011;32(3):91-8; quiz 99. doi: 10.1542/pir.32-3-91. [ Özet ]
22) Horne RSC, Ong C, Weichard A, Nixon GM, Davey MJ. Are there gender differences in the severity and consequences of sleep disordered in children? Sleep Med. 2020;67:147-155. doi: 10.1016/j.sleep.2019.11.1249. [ Özet ]
23) Keskin N, Keskin S. Association between adenotonsillar hypertrophy and leptin, ghrelin and IGF-1 levels in children. Auris Nasus Larynx. 2021;48(2):248-254. doi: 10.1016/j.anl.2020.08.002. [ Özet ]
24) Mantzoros CS, Magkos F, Brinkoetter M, Sienkiewicz E, Dardeno TA, Kim SY, Hamnvik OP, Koniaris A. Leptin in human physiology and pathophysiology. Am J Physiol Endocrinol Metab. 2011;301(4):E567-84. doi: 10.1152/ajpendo.00315.2011. [ Özet ]
25) Overduin J, Figlewicz DP, Bennett-Jay J, Kittleson S, Cummings DE. Ghrelin increases the motivation to eat, but does not alter food palatability. Am J Physiol Regul Integr Comp Physiol. 2012;303(3):R259-69. doi: 10.1152/ajpregu.00488.2011. [ Özet ]; PMCID: PMC3423988)
26) Kara CO, Ergin H, Koçak G, Kiliç I, Yurdakul M. Prevalence of tonsillar hypertrophy and associated oropharyngeal symptoms in primary school children in Denizli, Turkey. Int J Pediatr Otorhinolaryngol. 2002;66(2):175-9. doi: 10.1016/s0165-5876(02)00247-1. [ Özet ]
27) Mistretta A, Modica DM, Pitruzzella A, Burgio S, Lorusso F, Billone S, Valenti C, Vita G, Poma S, Amata M, Vita P, Gallina S. OSAHS Growth Impairment and Resolution after Adenotonsillectomy in Children. Iran J Otorhinolaryngol. 2022;34(122):145-153. doi: 10.22038/IJORL.2022.57642.2986. [ Özet ]
28) Schechter MS; Section on Pediatric Pulmonology, Subcommittee on Obstructive Sleep Apnea Syndrome. Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics. 2002;109(4):e69. doi: 10.1542/peds.109.4.e69. [ Özet ]