COMPARISON OF THE EFFECT OF TRADITIONAL SEPTOPLASTY AND ENDOSCOPIC SEPTOPLASTY ON VOICE QUALITY
Summary
Objectives: Our aim in this study was to examine and compare the effects of Traditional Septoplasty(TS) and Endoscopic Septoplasty(ES) on voice quality.Material-Methods: Based on clinical examination and paranasal CT, these patients were grouped according to the Mladina classification, and 456 patients with Mladine type 3 septal deviation were included in the study. 40 patients who met the study criteria and agreed to undergo surgery were included in the study. The study population comprised 20 patients in the TS group and 20 patients in the ES group. Praat voice analysis program was used for acoustic voice analysis. Preoperative and postoperative (1st and 3rd months) F0, jitter, shimmer and NHR (noise-harmonic ratio) values were compared between the groups.
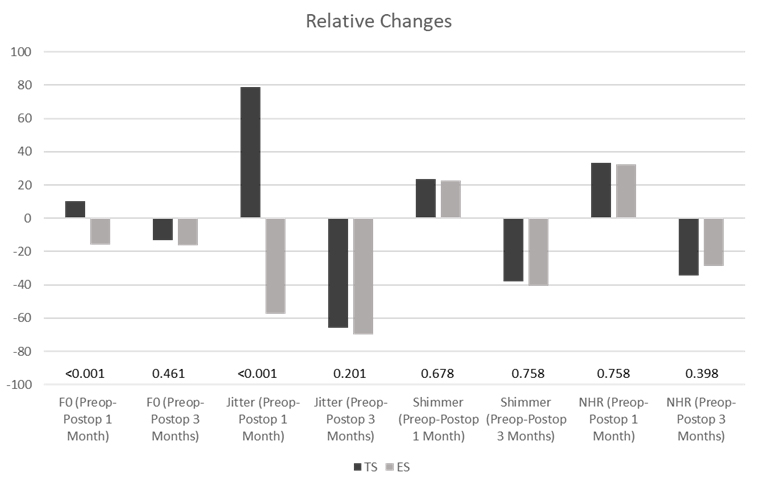
Results: The F0 and jitter change differed between the groups in the postoperative 1st month according to the preop value (p<0.001), and the F0 and jitter change in the postoperative 3rd month did not differ between the groups according to the preop value (p=0.249, p=0.100) .Preop-post op 1st-month and preop-postop 3rd-month shimmer and NHR change did not differ according to the groups (p=0.905, p=0.066) .There was a statistically significant difference between TS and ES only between pre-op F0-postop 1-month F0 change and preop jitter-post op 1-month jitter changes. In the ES group, F0 and jitter changes were higher at post-op 1 month compared with the TS group.
Conclusion: There is no difference in voice quality between endoscopic and traditional septoplasty methods in long-term evaluations.
Introduction
Nasal obstruction is one of the most important symptoms that bring patients to the Ear Nose and Throat Clinic. Today, the most common examination finding in patients presenting with nasal obstruction is septum deviation[1].The prevalence of septum deviation varies according to age and is 22% in newborns and up to 90% in adults[1,2]. With septum deviation, in addition to nasal obstruction, it can cause epistaxis, headache, sinusitis, and middle ear diseases. The treatment of septum deviation is the surgical correction of the nasal septum, that is, septoplasty. Traditional septoplasty (TS), described by Freer and Killian at the beginning of the 20th century, was modified by Cottle in the 1950s[3].In recent years, with the use of endoscopes in nasal surgery, endoscopic septoplasty (ES) has begun to be used in patients with the necessary indications. In TS, the septum is directly visualized with the help of a headlight and the field of view is provided by using a nasal speculum. However, in ES, vision is provided by using 0° or 30° endoscopes. There are studies in the literature showing that endoscopic septoplasty provides better images, shows posterior deviations better, is less invasive, and causes fewer complications compared with traditional septoplasty[4-6].Voice enables people to communicate and express themselves in social life. Voice is produced in the larynx when the air passing from the glottis to the lungs vibrates the vocal cords. Voice quality is affected by the anatomical structure of the upper respiratory tract[7].There are many studies in the literature showing that voice quality changes after septoplasty, adenotonsillectomy, endoscopic sinus surgery, and palatal surgeries involving the nasal, oral, and pharyngeal areas[8-9]. Mora et al. found significant positive changes in F0, jitter, shimmer, and the noise-to-harmonics ratio (NHR) after septoplasty[7]. By contrast, Hong reported that there was no change in these parameters[10]. Some studies have also reported that F0 changes after turbinate surgeries and uvulopalatoplasty[11].
Studies on traditional septoplasty and endoscopic septoplasty have generally been conducted to compare the performance of these two techniques regarding surgical time, surgical success, and postoperative complications[6]. To the best of our knowledge, there is no study in the literature that examines the effect of ES on voice quality with objective voice analysis methods and compares it with other septoplasty techniques . Our aim in this study is to examine the effect of ES on voice quality objectively and to compare it with TS.
Methods
Patients who presented to the Otorhinolaryngology and Head and Neck surgery clinic of Adana City Traning and Research Hospital between January 2021 and January 2022 with the complaint of nasal obstruction were included in this study.Anterior rhinoscopy and nasal endoscopy were performed on these patients, and paranasal CT was performed. Eight hundred sixty-two patients who were diagnosed as having septum deviation were included in the study. Based on clinical examination and paranasal CT, these patients were grouped according to the Mladina classification, and 456 patients with Mladine type 3 septal deviation were included in the study[12]. Mladina type 3 deviation includes unilateral deviations in the posterior nasal septum ,they can be corrected with both endoscopic and traditional methods, septoplasty surgery was recommended for these patients.Patients with a paranasal sinus infection, chronic nasal granulomatous disease, those who had received head and neck radiotherapy, patients with concha pathologies, those who had undergone septal surgery previously, those with asthma, a history of intubation in the last 3 months, patients who had undergone surgery on the vocal cords, and patients with lesions in the vocal cords in endoscopic examination, smoking, nasal drug use, and functional voice disorders, were excluded from the study.
Eighty-two patients who met the study criteria and agreed to undergo surgery were included in the study. Patients were selected randomly and some were TS and some were ES.Forty-two patients were excluded from the study because they did not attend post-op follow-ups and did not complete their voice recordings. The study population comprised 20 patients in the TS group and 20 patients in the ES group. The same general anesthesia was applied to all patients and all surgeries were performed by the same surgeon.
This study was approved by the local ethics committee (No: 2176)) in accordance with the Declaration of Helsinki.
Surgical Technique
Traditional Septoplasty. TS was performed under general anesthesia using a headlight with the help of a nasal speculum. Decongestion with oxymetazoline and submucosal local anesthetic (epinephrine and xylocaine 2%) injections were performed. A mucosal hemitransfixion incision was made using a size 15 scalpel. The mucosa was elevated using a Cottle elevator and the submucosal area was elevated to the posterior, and a mucoperichondrial flap was created. Posterior and inferior chondrotomy was performed from the septal cartilage. A contralateral mucoperichondrial flap was created. The bony septal deviation was removed using force and a hammer. Deviant cartilage fragments were removed en bloc using Weil forceps. Mucuperichondrial flaps were repositioned. The mucosal incision was sutured using absorbable sutures. Doyle nasal packing was placed in the nasal cavity. After 24 hours, the nasal packing was removed and nasal washing with physiologic saline was recommended. Antibiotherapy was given for 1-week post-op[4].
Endoscopic Septoplasty ES was performed under general anesthesia using a 0° 4-mm rigid endoscope. Decongestion with oxymetazoline and submucosal local anesthetic (epinephrine and xylocaine 2%) injections were performed. A mucosal Killian incision was made using a size 15 scalpel. The mucoperichondral flap was lifted under direct endoscopic imaging. A contralateral mucoperichondrial flap was created. Cartilage and bone curvatures were excised endoscopically using scissors and forceps. The flaps were then repositioned. Doyle nasal packing was placed in the nasal cavity. After 24 hours, the nasal packing was removed and nasal washing with physiologic saline was recommended. Antibiotic therapy was given post-op for 1 week[4].
Voice recording
Audio recordings were made in a soundproof room using the Audio Technica Model AT 2020 cardioid microphone. The microphone was taken 5 cm away from the patient's mouth. Audio recordings of all patients were made in mono at a sampling rate of 44100 Hz and in a 16-bit sampling format. All audio recordings were made 1 week before the surgery and 1 month - 3 months after the surgery. Praat version 6.017 was used for voice analysis[13]. F0, jitter, shimmer and NHR, which are the most frequently evaluated parameters in Pratt, were evaluated[14]. Analysis results were compared between the pre- and postoperative groups.
Statistical analysis
Data analysis was performed using the IBM SPSS 21 program . Normality control of continuous variables was evaluated using the Shapiro-Wilk test. Student"s t-test and the Mann-Whitney U test were used to compare two independent groups depending on the normality distribution of the data. The Friedman test was used to compare pre-op, post-op 1st month, and post-op 3rd month. In the determination of time group interaction, repeated measures analysis of variance (ANOVA) was used.
Results
There was no significant difference between the TS and ES groups in terms of age, BMI, and sex (Table 1).Table 1: Age, BMI and gender of traditional septoplasty and endoscopic septoplasty
The change in F0 and Jitter over time differed according to the groups separately (p<0.001). The F0 and jitter change differed between the groups in the postoperative 1st month according to the preop value (p<0.001), and the F0 and jitter change in the postoperative 3rd month did not differ between the groups according to the preop value (p=0.249, p=0.100) (Table 2, 3).
Preop-post op 1st-month and preop-postop 3rd-month shimmer and NHR change did not differ according to the groups (p=0.905, p=0.066) (Table 4, 5).
There was a statistically significant difference between TS and ES only between pre-op F0-postop 1-month F0 change and preop jitter-post op 1-month jitter changes (Table 6).
In the ES group, F0 and jitter changes were higher at post-op 1 month compared with the TS group (graphic 1).
 Büyütmek İçin Tıklayın |
Grafik 1: Preop-post op1 results of F0, jitter, shimmer and NHR in traditional septoplasty and endoscopic septoplasty groups. Difference of month and preop post op 3rd month values |
Discussion
As the importance of voice quality in our lives increases,studies on this subject have started to increase day by day.The anatomical structure of the upper respiratory tract such as the supraglottic larynx, pharynx, oral-nasal cavity and sinuses can affect the resonance of the voice and change the voice quality.I t is a situation that is predicted to change the voice quality in surgical interventions to these regions, and there are some publications in the literature about them[8,15].Atan et al. compared patients with severe and mild septum deviation, found a decrease in jitter and shimmer values in both groups at the post-op 1st month after septoplasty, but found a significant change in F0 value only in the group with severe septum deviation[8]. We did not group septum deviation as mild or severe in our study. We included only patients with Mladina type 3 septal deviation to ensure standardization because our study aimed to compare traditional and endoscopic methods. Mladina et al. divided the septum deviation into 7 types in 1995[12]. Types 1 and 2 include anterior deviations, and types 4-7 include more complicated and bilateral deviations. In our study, we evaluated the type 3 group with unilateral and more posterior deviation. Because this group is suitable for both TS and ES surgery.
There are studies in the literature showing that ES is more advantageous than TS[16]. Champagne et al. stated that the occlusion due to septal deformity decreased in both groups after TS and ES; the nasal passage was evaluated objectively using post-op rhinomanometry and there was no difference in surgical success between the two groups[6]. Similarly,, Garzaro et al. stated that the improvement in quality of life and the improvement in disease-related septum deviation were equal in both surgical methods[4]. Since ES provides a better view especially in posterior and inferior deviations, residual deviation rates are lower. While the incomplete improvement in septum deviation was 4.6% in the ES group, it was 12.4% in the TS group[4].In addition, it was reported that complications such as bleeding, mucosal damage and synechiae were less common in ES at 3-month follow-ups, and the surgical time was 28 minutes shorter on average[4,6].These are thought to be due to limited mucosal flap dissection and limited cartilage resection in ES. We did not evaluate these overall success parameters and complications. We compared the results of voice analysis after TS and ES.
While evaluating voice quality, objective methods are used as well as MDVP (Multi Dimensional Voice Program) and Praat. In our study, we used the Praat voice analysis method, which is the most frequently used objective method. Generally, F0, Jitter, shimmer, and NHR values are checked. In the literature, besides the studies examining the effect of septum deviation on voice quality by grouping it as mild and severe, there are also publications examining the change in voice quality according to the postoperative months[8,15]. In our study, we evaluated both different techniques and the voice quality in different months after surgery. F0 indicates the vibration rate of the vocal cords and is affected by the supraglottic structures.In the study by Atan et al., post-op F0 increased significantly in the group with severe septum deviation, whereas it decreased in the mild group[8]. In some studies, F0 increased in the 1st and 3rd months, but it decreased in other studies[17,18]. Nasal resistance generally depends on the shape and size of the nasal cavity. Most of this resistance is caused by the internal nasal valve[18].A significant increase in resonance is expected because the enlargement in the post-op nasal passage will be greater in the group with severe septum deviation. These differences between studies; may be according to the recovery period, the resorption process of edema in soft tissues and humoral factors in tissue healing may be.
Jitter and shimmer show amplitude and frequency irregularities in the svoice . The decrease in these parameters after the surgery indicates that the voice quality has changed positivel[18].In a post-op septoplasty study, Özbal Koç et al. reported that jitter and shimmer values increased in the 1st month and decreased in the 3rd month[18]. In a study by Apaydın et al., these values decreased both in the post-op 1st month and 3rd month[15].The reason for these differences between studies; may be due to the different size and volume of the intubation tube used during anesthesia, nasal lavage performed in the post-op period, and personal tissue healing factors. The unit of NHR is decibels, and high values indicate the increase of noise. NHR was not evaluated in most studies, it decreased after septoplasty in one study, as in our study[17].
In addition to many studies examining the effect of septoplasty on the voice, we think that our study will contribute to the literature both in terms of examining the effect of endoscopic septoplasty on the voice for the first time and comparing endoscopic and traditional methods. In the post-op late period, we saw that the voice quality changed positively and significantly in both methods, but there was no significant difference between them. In the early post-op period, there was a significant difference between the two groups only in F0 and jitter values. Due to the more localized mucosal elevation in the endoscopic method, earlier post-op limited edema may explain the decrease in jitter in the post-op 1st month. F0 indicates the vibrational rate of the vocal cords and is influenced by the supraglottic structures.Changes in F0 may be associated with all supralaryngeal structures.
Limitation. Praat voice analysis method was used because our study was the evaluation of voice quality with objective methods. Subjective methods such as Voice Handicap Index were not used. Objective and subjective methods to evaluate voice quality can be used together in future studies.In addition, multicenter studies with more patients in the study may be conducted in the future.
Reference
1) Sathyaki DC, Geetha C, Munishwara GB, Mohan M, Manjuanth K. A comparative study of endoscopic septoplasty versus conventional septoplasty. Indian J Otolaryngol Head Neck Surg. 2014;66(2):155-161. doi:10.1007/s12070-013-0692-0 . [ Özet ] PMCID: PMC4016353.
2) Hong, C. J., Monteiro, E., Badhiwala, J., Lee, J., de Almeida, J. R., Vescan, A.,, et al. Open versus endoscopic septoplasty techniques: A systematic review and meta-analysis. Am J Rhinol Allergy. 2016;30(6):436-442. doi:10.2500/ajra.2016.30.4366. [ Özet ]
3) Zhao KQ, Pu SL, Yu HM. Endoscopic Septoplasty with Limited Two-line Resection: Minimally Invasive Surgery for Septal Deviation. J Vis Exp. 2018;(136):57678. Published 2018 Jun 20. doi:10.3791/57678. [ Özet ] PMCID: PMC6101966
4) Garzaro M, Dell'Era V, Riva G, Raimondo L, Pecorari G, Aluffi Valletti P. Endoscopic versus conventional septoplasty: objective/subjective data on 276 patients. Eur Arch Otorhinolaryngol. 2019;276(6):1707-1711. doi:10.1007/s00405-019-05393-w. [ Özet ]
5) Juniper EF, Guyatt GH. Development and testing of a new measure of health status for clinical trials in rhinoconjunctivitis. Clin Exp Allergy. 1991;21(1):77-83. doi:10.1111/j.1365-2222.1991.tb00807.x,. [ Özet ]
6) Champagne C, Ballivet de Régloix S, Genestier L, Crambert A, Maurin O, Pons Y. Endoscopic vs. conventional septoplasty: A review of the literature. Eur Ann Otorhinolaryngol Head Neck Dis. 2016;133(1):43-46. doi:10.1016/j.anorl.2015.11.004. [ Özet ]
7) Mora R, Jankowska B, Dellepiane M, Mora F, Crippa B, Salami A. Acoustic features of voice after septoplasty. Med Sci Monit. 2009;15(6):CR269-CR273. [ Özet ]
8) Atan D, Özcan KM, Gürbüz AB, Dere H. The Effect of Septoplasty on Voice Performance in Patients With Severe and Mild Nasal Septal Deviation. J Craniofac Surg. 2016;27(5):1162-1164. doi:10.1097/SCS.0000000000002794. [ Özet ]
9) Koo SK, Kwon SB, Chon KM, Kim YJ, Kim YJ. The role of the maxillary sinus on the voice. Eur Arch Otorhinolaryngol. 2015;272(9):2347-2350. doi:10.1007/s00405-014-3357-z. [ Özet ]
10) Hong, C. J., Monteiro, E., Badhiwala, J., Lee, J., de Almeida, J. R., Vescan, A., et al. Effect of Septoplasty on Voice Quality: A Prospective-Controlled Trial. Clin Exp Otorhinolaryngol. 2016;9(3):238-243. doi:10.21053/ceo.2015.01354. [ Özet ] PMCID: PMC4996097
11) Göker, A. E., Aydoğdu, İ., Saltürk, Z., Berkiten, G., Atar, Y., Kumral, T. L.et al. Comparison of Voice Quality Between Patients Who Underwent Inferior Turbinoplasty or Radiofrequency Cauterization. J Voice. 2017;31(1):121.e17-121.e21. doi:10.1016/j.jvoice.2016.02.002. [ Özet ]
12) Mladina, R., Heinzel, B., Belussi, L. and Passali, D. (1995) Staging in Rhino Sinusitis Septal Deformities. Rivista Italiana Di Oto Laringologi, 7, 16.
13) Tuhanioğlu, B., Erkan, S. O., Özdaş, T., Derici, Ç., Tüzün, K., & Şenkal, Ö. A.et al. The Effect of Electronic Cigarettes on Voice Quality. J Voice. 2019 Sep;33(5):811.e13-811.e17. doi: 10.1016/j.jvoice.2018.03.015. [ Özet ]
14) Shrivastava D. Impact of sleep-disordered breathing treatment on upper airway anatomy and physiology.Sleep Med. 2014;15(7):733-741. doi:10.1016/j.sleep.2014.01.002. [ Özet ]
15) Apaydın E, İkincioğulları A, Çolak M, Atan D, Ensari S, Dere HH. The Voice Performance After Septoplasty With Surgical Efficacy Demonstrated Through Acoustic Rhinometry and Rhinomanometry. J Voice. 2020;34(4):649.e15-649.e20. doi:10.1016/j.jvoice.2019.01.008. [ Özet ]
16) Kemker BJ, Corey JP, Branca J, Gliklich RE. Development of the allergy outcome survey for allergic rhinitis. Otolaryngol Head Neck Surg. 1999;121(5):603-605. doi:10.1016/S0194-5998(99)70065-3. [ Özet ]
17) Ersoz Unlu C, Akkoca O. The effect of nasal septum deviation on voice aging. Logoped Phoniatr Vocol. 2022;47(3):189-193. doi:10.1080/14015439.2021.1904285. [ Özet ]
18) Ozbal Koc EA, Koc B, Ercan I, Kocak I, Tadihan E, Turgut S. Effects of septoplasty on speech and voice. J Voice. 2014;28(3):393.e11-393.e3.93E15. doi:10.1016/j.jvoice.2013.09.008. [ Özet ]




