COMPARISON OF MICROSCOPIC AND ENDOSCOPIC SURGICAL APPROACHES IN PITUITARY ADENOMAS
2Adana Şehir Hastanesi, KBB, Adana, Turkey
3Adana Şehir Hastanesi, Nöroşirürji, Adana, Turkey
4Eskişehir Şehir Hastanesi, KBB, Eskişehir, Turkey
Summary
Objective: To compare the endoscopic endonasal transsphenoidal approach and microscopic transnasal transsphenoidal approach, which are used in the surgical treatment of pituitary adenomas.Method: Eighty-six patients who underwent surgery for pituitary adenoma and whose files and radiologic examinations could be accessed from archive records were included in the study. The files of the patients were examined retrospectively, and their ages, gender, preoperative laboratory and imaging findings, length of hospital stay, postoperative complications, postoperative laboratory and imaging findings were evaluated.
Results: Endoscopic surgery was performed in 45 of 86 patients, and microscopic surgery was performed in 41. Twenty of the patients in the endoscopic group had non-functional pituitary adenomas, and 25 had functional adenomas. In the microscopic group, 23 patients had non-functional pituitary adenomas, and 18 had functional adenomas. In the endoscopic group, radiologic remission was achieved in 37 (82.2%) adenomas. In the microscopic group, remission was achieved in 16 (39%) adenomas. Hormonal remission was achieved in 16 (64%) functional adenomas in the endoscopic group. In the microscopic group, hormonal remission was achieved in five (27.8%) functional adenomas. In the endoscopic group, 26 patients had various complications; in the microscopic group, 22 patients had various complications. The median length of hospitalization of the patients in the endoscopic group was 5 days and 7 days in the microscopic group.
Conclusion: This study seems to indicate that endoscopic endonasal transsphenoidal surgery can provide a better tomur resection and preservation of pituitary gland.
Introduction
Pituitary adenomas develop from the anterior adenohypophysis cells and they are the most common benign tumors of the sellar and parasellar region[20]. Although pituitary adenomas are benign masses, they may have a morbid or even mortal course due to the symptoms they cause related to excessive hormone secretion and/or the mass effect they cause on surrounding tissues[15]. The main purpose of the surgical treatment of pituitary adenomas is to remove the compression effect of the mass by removing adenoma tissue, preserving normal pituitary tissue and correcting metabolic disorders caused by excess hormone release[23].Different surgical approaches can be used in the treatment of pituitary adenomas. The choice of surgical approach depends on a few factors. The most important factors are the size of the sella, the degree of mineralization, the size and pneumatization of the sphenoid sinus, the position of the carotid arteries, the presence and direction of growth of any intracranial tumor, the presence of any doubt about the pathology of the lesion and whether treatment was given previously.
The microscopic method, which was used more frequently in pituitary surgery in the past, has left its place to the endoscopic method. The endoscopic method allows us to provide a better view, greater magnification and a good panoramic view[8,14]. However, using an endoscope requires considerable time and effort for neurosurgeons who are used to surgery with a microscope. Therefore, pituitary surgery has become more reliable as a result of the joint work of the otolaryngology and neurosurgery clinics[6,10]. In this study, the duration of hormonal remission, radiologic remission, residual tissue, surgical complication and the hospital stay of patients who underwent surgery with endoscopic and microscopic approaches for pituitary adenoma were compared.
Methods
Eighty-six patients who underwent surgery for pituitary adenomas and whose necessary files and radiologic examinations could be accessed from archive records were included in the study. Patients with incomplete data and those with hormonal dysfunction after previous surgery were excluded from the study. The files and radiologic examinations of the patients who underwent surgery were obtained by scanning the hospital archive.In our study, patients were divided into two groups according to the surgical method used. Forty-five patients who underwent surgery with an endoscopic endonasal transsphenoidal approach (endoscopic group) and 41 patients who had the microscopic transnasal transsphenoidal approach (microscopic group) were evaluated.
Detailed anamnesis gathered from the patients' files were examined, and their physical and neurologic examinations were noted. In these examinations, it was evaluated whether there were signs and symptoms related to headache, visual disturbance, menstrual cycle disorders, galactorrhea, enlargement of the extremities, impotence, infertility and endocrinologic disorders. Then, the laboratory values of the patients were examined. Routinely studied endocrinologic hormone profiles were obtained in pituitary pathologies. Prolactin (PRL), luteinizing hormone (LH), follicle-stimulating hormone (FSH), sexual hormones, thyroid-stimulating hormone (TSH), thyroid function tests (T3, T4), growth hormone (GH), insulin-like growth factor-1 (IGF-1), adrenocorticotropic hormone (ACTH), cortisol level and fasting blood glucose levels were noted. The preoperative visual function of all patients was noted. In the neuroradiologic evaluation, preoperative routine paranasal computed tomography (CT) and pituitary magnetic resonance imaging (MRI) examinations of all patients were examined.
Surgical Approach
All surgeries were performed by the same surgeons in partnership.
Endoscopic Approach
Paranasal sinus CT was performed in all patients before the surgery and the access to the sella and the pathologies of this route were evaluated. Classic endoscopic mononostril transsphenoidal surgery was performed in all patients. After the tumor excision was completed, reconstruction was performed with fat and fascia taken from the thigh and fibrin glue (Figure 1). The reconstruction was supported with a posterior nasal pack and a Merocel pack (anterior pack).
Microscopic Approach
A standard submucosal transseptal transsphenoidal microsurgery procedure was performed to the patients. After the tumor excision was completed, fat tissue was placed in the tumor bed, and reconstruction was performed using the removed bone and cartilage tissue and a graft was taken from the fascia lata. Packs were placed in both nostrils.
Postoperative Follow-up
The patients were followed up in the intensive care unit for the first 24 hours in the postoperative period. Patients whose general condition improved were discharged. After discharge, the patients were called for follow-up at the first and third months. Routine biochemical, endocrinologic, and MRI examinations were performed. Postoperative late period (1-3 months) hormone tests and follow-up MRI examinations were performed. Patients who were found to have total resection according to MR imaging were evaluated as patients having radiologic remission. During the follow-up of the patients, they were referred to the ophthalmology clinic and their visual examinations were repeated. All patients were followed up for at least 3 months.
Hormonal cure criteria for functional adenomas
1. In prolactinoma; Decrease in serum prolactin level below 20 ng/mL without the need for any medical support in the postoperative 6th week.
2. In acromegaly; fasting GH being <2.5 ng/mL, a decrease in GH values below 1 µg/L after an oral glucose tolerance test and a decrease in IGF-1 levels to normal values for patient age.
3. In ACTH secreting adenomas; ACTH levels 10-90 pg/mL and blood serum cortisol levels being below 5µg/dL (50 nmol/L) in the morning and returning of urinary cortisol levels to normal (35-135 pg/24 hours).
4. In adenomas secreting TSH; decrease in TSH level in the morning of the first postoperative day and returning of serum T3, T4 and TSH levels to the normal range in the late postoperative period.
5. In adenomas secreting FSH/LH: normalization of FSH, LH, estradiol levels by age for women and normalization of LH and testosterone levels for men.
The diagnostic criterias used for central diabetes insipidus are serum sodium >142 mmol/L and serum osmolarity >300 mOsm/kg; urine density <1010 and urine osmolality <300 mOsm/kg (1,2,4).
Statistical Analysis
The analysis of the data was performed using the SPSS for Windows 11.5 package program. Descriptive statistics are given as age, mean ± standard deviation, duration of follow-up, median (minimum-maximum), and nominal variables as the number of cases and percentage (%). Normality assessments of age and hospitalization periods were performed using the Shapiro-Wilk test. Student's t-test was used for the comparison of means of age because it showed normal distribution in microscopic and endoscopic groups, and the Mann-Whitney U test was used because the hospitalization period did not show normal distribution. In the analysis of categorical data, the Chi-square test and Fisher's exact test were used in cases of expected values less than 5. Logistic regression analysis was used to determine the difference between the endoscopic group and microscopic group in terms of cure status. Statistical significance level was accepted as p<0.05.
 Büyütmek İçin Tıklayın |
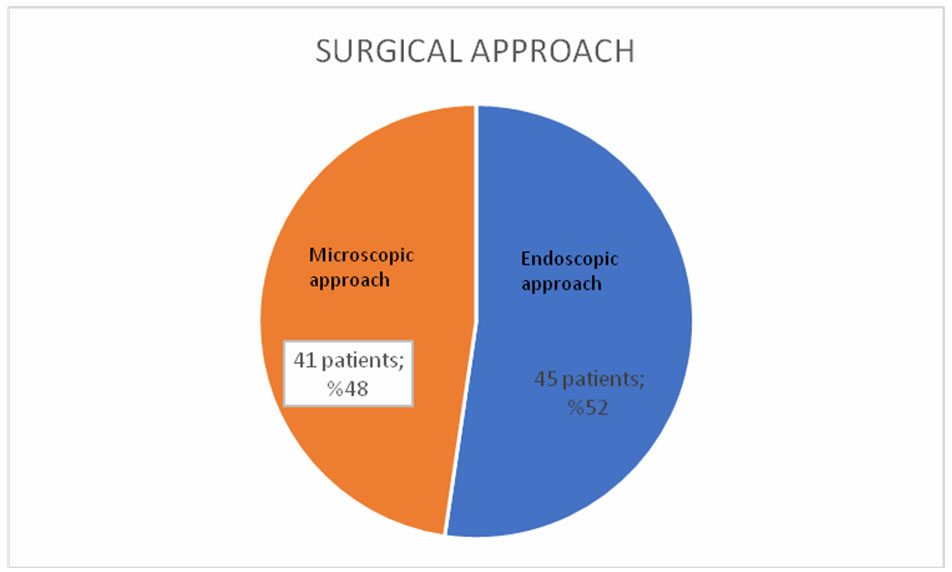
Figure 2: Patients by surgical approach |
 Büyütmek İçin Tıklayın |
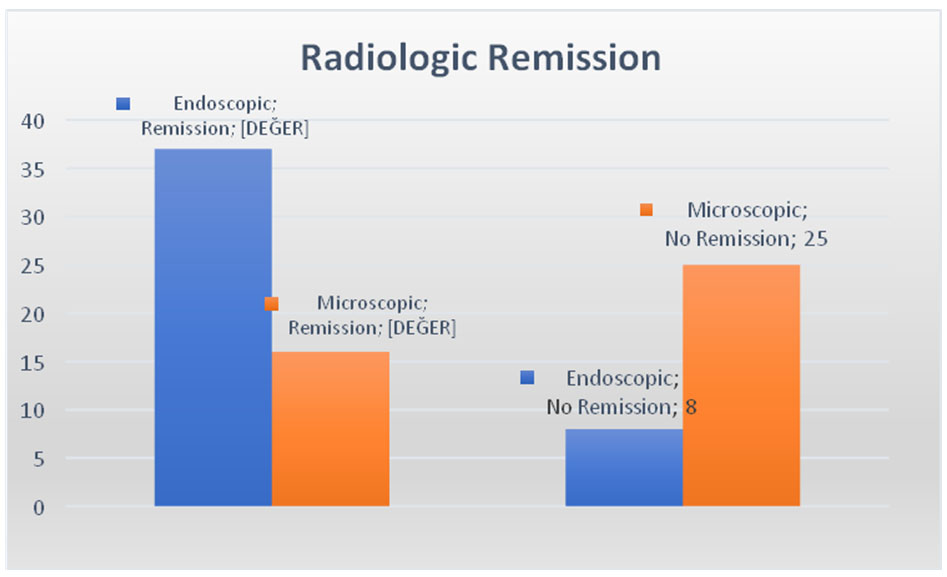
Figure 3: Comparison of the groups in terms of radiologic remission |
 Büyütmek İçin Tıklayın |
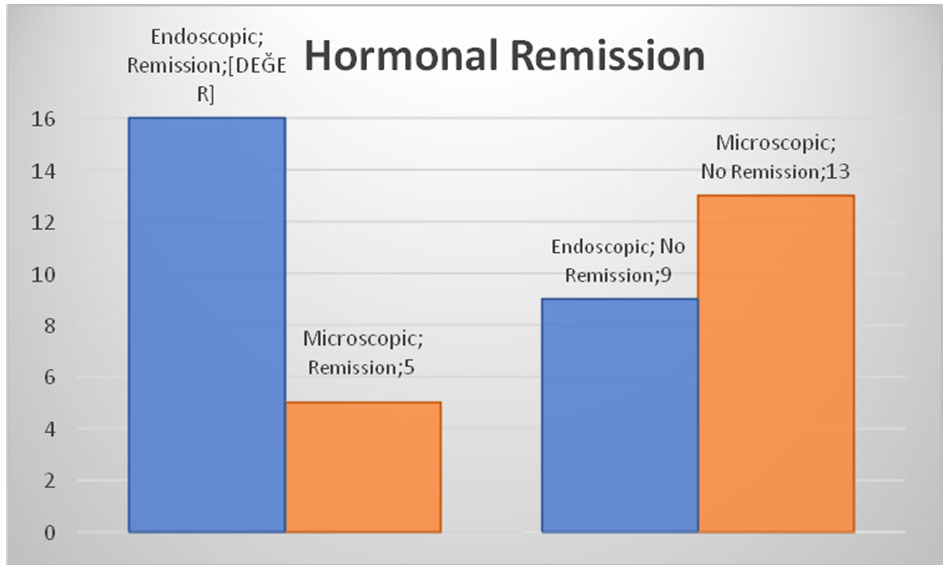
Figure 4: Comparison of the groups in terms of hormonal remission |
Results
Endoscopic endonasal transsphenoidal surgery was performed in 45 (52%) of 86 patients, and microscopic transnasal transsphenoidal surgery was performed in 41 (48%).Demographic details and general results are available in Table 1. Age and gender showed homogeneous distribution in the endoscopic and microscopic groups.
Table 1: Patients" characteristics and results of both group
Twenty patients in the endoscopic group had non-functional pituitary adenomas and 25 had functional adenomas. In the microscopic group, 23 patients had non-functional pituitary adenomas and 18 had functional adenomas. There was no significant difference between the groups in terms of the rates of adenoma types (p>0.05).
According to preoperative MR imaging, seven patients in the endoscopic group had microadenomas and 38 had macroadenomas and in the microscopic group, one had microadenoma and the remaining 40 had macroadenomas. There was no significant difference between the groups in terms of microadenoma rates (p=0.06).
According to postoperative MR imaging, 37 patients in the endoscopic group had a total resection and eight had residual tissue. In the microscopic group, total resection was detected in 16 patients and residual tissue was detected in 25. As a result of the comparison of the groups in terms of radiologic remission, it was observed that there were statistically significant differences between patients in the endoscopic group and those in the microscopic group (p<0.001). There was a statistically significant relationship between the groups and radiologic remission (p=0.001). Accordingly, the rate of radiologic remission in the endoscopic group was 7.2-times higher than in the microscopic group (Table 2).
Table 2: Comparison of the groups in terms of radiologic remission
Hormonal remission was achieved in 16 functional adenomas in the endoscopic group, but not achieved in nine. In the microscopic group, hormonal remission was achieved in five functional adenomas but not achieved in 13. In the group comparison of hormonal remission among functional adenomas, it was found that the patients in the endoscopic group had a higher level of remission compared with those in the microscopic group and there were statistically significant differences between them (p=0.021).
In the endoscopic group, there were no complications in 25 patients in the postoperative period; however, eight patients had transient DI, seven had anterior pituitary insufficiency, four had permanent DI, three had CSF rhinorrhea, two had meningitis, and two patients had syndrome of inappropriate antidiuretic hormone (SIADH). In the microscopic group, 23 patients had no complications; however, eight patients had transient DI, eight had anterior pituitary insufficiency, four had permanent DI, one had meningitis, and one patient had SIADH. There was no significant difference between the groups in terms of complication rates (p>0.05).
In the endoscopic group, while evaluating the hospitalization period of the patients, the median value was determined as 5 days, with the shortest being 4 days and the longest 25 days. In the microscopic group, the median value was determined as 7 days, with the shortest 3 days and the longest 22 days. A statistically significant difference was found between the groups in terms of median hospitalization period (p<0.001).
Discussion
The standard treatment in pituitary surgery was the microscopic method, until the 2000s. The endoscopic method provides a better view, greater magnification, and a good panoramic view[8,14]. For neurosurgeons who are used to surgery with a microscope, using an endoscope requires considerable time and effort. O'Malley et al. emphasized the importance of experience in achieving success in endoscopic surgery[17]. Pituitary surgery has become more reliable with the joint work of ENT and NRS clinics[1]. In this study, endoscopic endonasal transsphenoidal approach and microscopic transnasal transsphenoidal approach used in the surgical treatment of pituitary adenomas were compared in terms of radiologic remission, residual tissue, hormonal remission and surgical complications.The main reasons for residual tumor tissue after pituitary surgery are the desire to preserve pituitary functions and the tumor invasion of the surrounding tissues. O'Malley et al. reported residue rates as 23% in microscopic surgery and 34% in endoscopic surgery[17]. Higgins et al. reported that the residue rate was 17% in microscopic surgery and 11% in endoscopic surgery[14]. In our study, the total resection rate of the tumor was 82.2% in the endoscopic group and 39% in the microscopic group; residua rate was 17.8% in the endoscopic group and 61% in the microscopic group. We could attribute this result to the better quality and closer view provided by the endoscope, the better differentiation of tumor tissue from the healthy pituitary tissue and the wider viewing field provided by angled endoscopes.
The rate of hormonal remission in all functional adenomas was found as 79% in a meta-analysis published by Tabaee et al., when the hormonal remission rates in functional adenomas were examined[19]. In a series of 139 functional adenomas by Kabil et al., this rate was reported as 87[16]. D'Haens et al. reported a hormonal remission rate of 50% in functional pituitary adenomas that underwent surgery with a microscope compared with the surgical approach and this rate was reported as 63% in patients who underwent surgery with an endoscope[7]. In our study, hormonal remission was achieved in 16 (64%) functional adenomas in the endoscopic group and 5 (27.8%) in the microscopic group.
DI is the most common pituitary dysfunction after transsphenoidal surgery. Transient DI is seen at a rate of 15-60%, permanent DI is less common[24]. In a case series by Agam et al. including 1153 patients, no significant difference was found between the endoscopic and microscopic groups in terms of DI, the rates of transient and permanent DI were 4.3% and 0.3%, respectively[3]. O'Malley et al. reported the DI rate as 16% in the microscopic group and 8% in the endoscopic group[17]. In a study by Guo-Dong et al. of 247 patients, the rate of transient DI was 18.4% in the microscopic group and 13% in the endoscopic group and the rate of permanent DI was found as 0% in the microscopic group and 1% in the endoscopic group[12]. In our study, no statistically significant difference was found between the groups in terms of DI rates.
One of the most common complications in transsphenoidal approach is rhinorrhea, which occurs following CSF fistula. Different rates have been presented in many studies for postoperative rhinorrhea. In a meta-analysis by Goudakos et al., the rate of rhinorrhea was reported as 19.5% in the endoscopic group and 14.4% in the microscopic group[11]. Agam et al. reported the incidence of CSF rhinorrhea as 2.6%, and stated that there was no significant difference between endoscopic and microscopic groups[3]. O'Malley et al. reported that there was no difference between the endoscopic and microscopic groups in terms of CSF rhinorrhea incidence[17]. In our study, CSF rhinorrhea was not observed in patients who underwent microscopic surgery, but it was seen in three patients who had endoscopic surgery.
Postoperative meningitis risk has mostly been found as similar between endoscopic and microscopic groups in previous studies, at around 1%[11,18,21]. In a meta-analysis conducted by Ammirati et al., the risk of meningitis was found as 1% in the endoscopic group and 2% in the microscopic group[5]. In our study, the postoperative meningitis rate was 2.4% in patients in the microscopic group and 4.4% in the endoscopic group.
Gao et al. reported the incidence of anterior pituitary insufficiency as approximately 3% after microscopic pituitary surgery, lower than in the endoscopic group, but there was no statistically significant difference[9]. In a study of 247 patients conducted by Guo-Dong et al., the rate of pituitary insufficiency was found as 3% in the endoscopic group and 0.7% in the microscopic group[12]. Güvenç et al. found the rate of pituitary insufficiency as 6.1% in the microscopic group and 17.8% in the endoscopic group[13]. In our study, the rate of pituitary insufficiency was 19.5% in patients in the microscopic group and 15.6% in the endoscopic group.
Although rare, mortality can be seen in pituitary surgery. In a series of 1000 patients, Wilson reported the mortality rate in pituitary surgery as 0.2%[22]. No mortality was reported by Kabil et al. [16]. In our study, there was no surgical mortality.
The invasiveness of surgery performed in patients is one of the most important factors affecting the recovery process in the postoperative period. The duration of the patients' stay in the hospital varies according to the recovery process. O'Malley et al. compared endoscopic and microscopic pituitary surgeries performed by the same surgeon and it was reported that the duration of hospital stay was shorter in the endoscopic group. In that study, the average length of hospital stay was 3.9 days in the endoscopic group and 4.8 days in the microscopic group[17]. In a meta-analysis by Gao et al., the average length of hospital stay of the endoscopic group was 3.8 days, whereas this period was 6.3 days in the microscopic group and a significant difference was found between the groups[9]. Simal-Julian et al. found the duration of hospital stay to be shorter in the endoscopic group compared with the microscopic group, but there was no statistically significant difference[18]. In our study, the duration of hospital stay was statistically shorter in the endoscopic group compared with the microscopic group.
Conclusion
Endoscopic endonasal transsphenoidal and microscopic transnasal transsphenoidal surgery have been compared many times to find the most effective, most advantageous, and least damaging method for the surgical treatment of pituitary adenomas. In our study, when the two methods were compared in terms of postoperative radiologic remission, postoperative hormonal remission and hospital stay, significantly better results were observed in the endoscopic group. No significant difference was observed in terms of complications with either surgical method.As a result, the endoscopic method seems more effective and advantageous than the microscopic method, but longer studies with larger numbers of patients are required to draw firm conclusions.
Reference
1) Abosch A, Tyrell JB, Lamborn KR, Hannegan LT, Applebury CB, Wilson CB. Trans sphenoidal microsurgery for growth hormone secreting pituitary adenomas: initial outcome and long-term results. Int J Clin Endocrinol Metab. 1998;83:3411-8. 2) Adams JR, Blevins LS, Allen GS, Verity DK, Devin JK. Disorders of water metabolism following transsphenoidal pituitary surgery: a single institution's experience. Pituitary. 2006; 9(2):93-9. [ Özet ]
3) Agam MS, Wedemeyer MA, Wrobel B, Weiss MH, Carmichael JD, Zada G. Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J neurosurg 2018; 130(5), 1576-83. [ Özet ]
4) Ahn JY, Jung JY, Kim J, Lee KS, Kim SH. How to overcome the limitations to determine the resection margin of pituitary tumours with low-field intraoperative MRI during transsphenoidal surgery: usefulness of Gadolinium-soaked cotton pledgets. Acta Neurochir (Wien) 2008;150:763-71. [ Özet ]
5) Ammirati M, Wei I, Ciric I. Short-term outcome of endoscopic versus microscopic pituitary adenoma surgery: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry 2013;84:843-9. [ Özet ]
6) Cappabianca P, Cavallo LM, de Divitiis E. Endoscopic endonasal transsphenoidal surgery. Adv Tech Stand Neurosurg 2004; 55(4): 933-40. [ Özet ]
7) D'Haens J, Van Rompaey K, Stadnik T, Haentjens P, Poppe K, Velkeniers B. Fully endoscopic transsphenoidal surgery surgery for functioning pituitary adenomas A retrospective comparison with traditional transsphenoidal microsurgery in the same instution. Surg Neurol 2009; 72. 336-40. [ Özet ]
8) Dusick Jr, Esposito F, Kelly DF, Cohan P, DeSalles A, Becker DP, Martin NA. The extended direct endonasal transsphenoidal approach for nonadenomatous suprasellar tumors. J Neurosurg 2005; 102: 832-41. [ Özet ]
9) Gao Y, Zhong C, Wang Y, Xu S, Guo Y, Dai C, Zheng Y, Wang Y, Luo Q, Jiang J. Endoscopic versus microscopic transsphenoidal pituitary adenoma surgery: a meta-analysis. World J Surg Oncol 2014; 12: 94. [ Özet ]
10) Gondim JA, Schops M, de Almeida JP, de Albuquerque LA, Gomes E, Ferraz T, Barroso FA. Endoscopic endonasal transsphenoidal surgery: surgical results of 228 pituitary adenomas treated in a pituitary center. Pituitary 2010;13(1): 68-77. [ Özet ]
11) Goudakos JK, Markou KD, Georgalas C. Endoscopic versus microscopic trans-sphenoidal pituitary surgery: a systematic review and meta-analysis. Clin. Otolaryngol. 2011; 36(3), 212-20. [ Özet ]
12) Guo-Dong H, Tao J, Ji-Hu Y, Wen-Jian Z, Xie-Jun Z, Jian G, Zhen L, Tai-Peng J, Jian-Jun D, Yong-Zhong G, Wenlan L, Wei-Ping L. Endoscopic versus microscopic transsphenoidal surgery for pituitary tumors. J Craniofac Surg 2016; 27(7), 648-55. [ Özet ]
13) Guvenc G, Kizmazoglu C, Pinar E, Imre A, Kay I, Bezircioğlu H, Yuceer N. Outcomes and complications of endoscopic versus microscopic transsphenoidal surgery in pituitary adenoma. J Craniofac Surg 2016; 27(4), 1015-20. [ Özet ]
14) Higgins TS, Courtemanche C, Karakla D, Strasnick B, Singh RV, Koen Jl, Han JK. Analysis of transsphenoidal endoscopic versus transsphenoidal microscopic approach for excision of pituitary tumors. Am J Rhinol 2008; 22(6): 649-52. [ Özet ]
15) Jagaan-than J, Dumant AS, Jane JA Jr. Diagnosis and management of pediatric sellar lesion. Front Horm Res. 2006; 34: 83-104. [ Özet ]
16) Kabil MS, Eby JB, Shahinian HK. Fully endoscopic endonasal vs. transseptal transsphenoidal pituitary surgery. Minim Invasive Neurosurg 2005;48:348-54. [ Özet ]
17) O"Malley BW Jr, Grady MS, Gabel Bc, Cohen Ma, Heuer GG, Pisapia J, Bohman LE, Leibowitz JM. Comparison of endoscopic and microscopic removal of pituitary adenomas: Single-surgeon experience and the learning curve. Neurosurg Focus 2008; 25(6):10. [ Özet ]
18) Simal-Julian JA, Miranda-Lloret P, Pancucci G, Evangelista-Zamora R, Perez-Borreda P, Sanroman-Alvarez P, Cámara-Gómez R, Botella-Asunción C. Microscopic versus endoscopic pituitary surgery. Neurocirugia (Astur) 2014; 25:170-8. [ Özet ]
19) Tabaee A, Anand vK, Brown Y, Hiltzik DH, Brown SM, Kacker A, Mazumdar M, Schwartz TH. Endoscopic pituitary surgery: A systematic review and meta-analysis. J Neurosurg 2009;111:545-54. [ Özet ]
20) Tascıoglu B, Basar R. Sellar Bolgenin ve Hipofiz Bezinin Anatomisi. 1. Baskı. Editor: Ziyal Erbas T. Hipofiz Adenomları, Hacettepe Universitesi Yayınları, Ankara 12-21, 2008.
21) Wang F, Zhou T, Wei S, Meng X, Zhang J, Hou Y, Sun G. Endoscopic endonasal transsphenoidal surgery of 1,166 pituitary adenomas. Surg Endosc 2015; 29:1270-80. [ Özet ]
22) Wilson CB. A decade of pituitary microsurgery the Herbert olivecrona lecture. J Neurosurg 1984; 61: 814-33. [ Özet ]
23) Wilson CB. Extensive personal experience "surgical management of pituitary tumors". Int J Clin Endocrinol Metab 1997; 82:8. [ Özet ]




