EFFICACY OF MODIFIED CLOSED REDUCTION MANEUVER IN TEMPOROMANDIBULAR DISEASES OTHER THAN JOINT DISLOCATION
2Manisa Celal Bayar Üniversitesi Tıp Fakültesi, Kulak Burun Boğaz Hastalıkları Anabilim Dalı, Manisa, Turkey
Summary
Objective: The aim of the study is to evaluate the effectiveness of the modified closed reduction maneuver in patients with temporomandibular disease other than joint dislocation.Material and Methods: 218 patients with suspected temporomandibular disease who applied to the outpatient clinic with complaints of earache, jaw pain, noise in the joint, and pain radiating to the head, face, and neck were reviewed. The data of 153 patients who underwent the modified closed reduction maneuver were included. These patients were divided into two groups according to their short-term or long-term complaints. The patients" visual analog scale scores before and after undergoing the modified closed reduction maneuver were compared within and between groups.
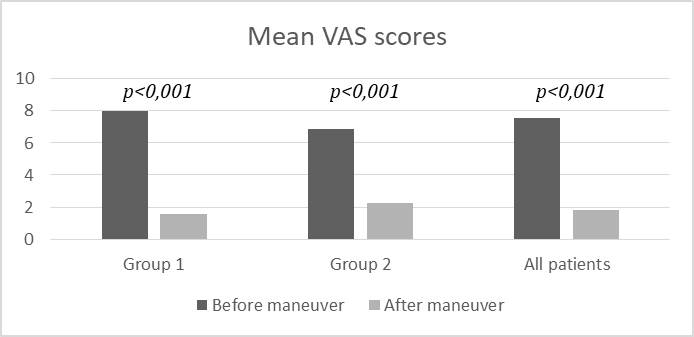
Results: The overall mean visual analog scale scores of both groups before and after undergoing the maneuver were 7.54±1.07 and 1.82±1.09, respectively (p<0.001). The visual analog scale scores were significantly decreased after the maneuver in each group (p<0.001). The overall scores of both groups were also found to be significantly decreased after the maneuver (p<0.001).
Conclusion: According to the current study, the modified closed reduction maneuver is effective for symptom control in patients with temporomandibular diseases (other than joint dislocation). It may be proposed as an alternative to the other treatment modalities or used in combination with them.
Introduction
Pain in the jaw and face region affects quality of life[1]. Temporomandibular muscle and joint disorders (formerly "temporomandibular joint dysfunction) are characterized by acute or chronic dysfunction and pain associated with the temporomandibular joint (TMJ) and/or masticatory muscles. They are the most common cause of orofacial pain[2]. Diagnostic Criteria for these temporomandibular diseases (TMD) were defined in 1992[3]. Many studies have been conducted to evaluate the reliability and validity of this taxonomic system[4-9]. The final version of the diagnostic criteria was published in 2014 and has taken its current form with minor revisions[10]. In this last version, TMD is divided into two major groups: pain-related TMD and TMJ intra-articular disorders. Although the diagnostic criteria have become clear and well grouped, the signs and symptoms of these two groups are extremely similar. In the literature, the overall prevalence of TMD has been reported approximately 31% on adults/elderly[11]. Despite its relatively high prevalence, the level of public awareness is quite low. This leads to referral to non-relevant clinics, which causes delays in diagnosis and treatment. With the acute onset of severe pain, patients" quality of life decreases. Pain control and treatment become compelling when TMD becomes arduous because of delayed diagnosis. In some patients, the clinical picture is severe; likewise, the symptoms may be of varying degrees in a similar clinical picture[12]. For these reasons, difficulties are experienced in TMD treatment. Medical treatment (oral treatment and intra-articular injections), physical therapy, dental treatments, surgery and other treatment options (acupuncture, etc.) are available in the management of TMD. However, most of these treatment modalities vary considerably in effectiveness, and it takes time to get satisfactory results. Currently, there is a lack of a simple, rapid, easy-to-apply and fast- response method that can reduce or eliminate the pain symptoms of patients at the time of admission.In this study, we evaluated the modified closed reduction maneuver (MCRM), which is modified from the closed reduction maneuver used in TMJ dislocations by us. This maneuver can be easily applied to patients with TMD in outpatient settings and rapid response can be obtained. We aimed to evaluate the effectiveness of this maneuver using pain-related visual analog scale (VAS).
Methods
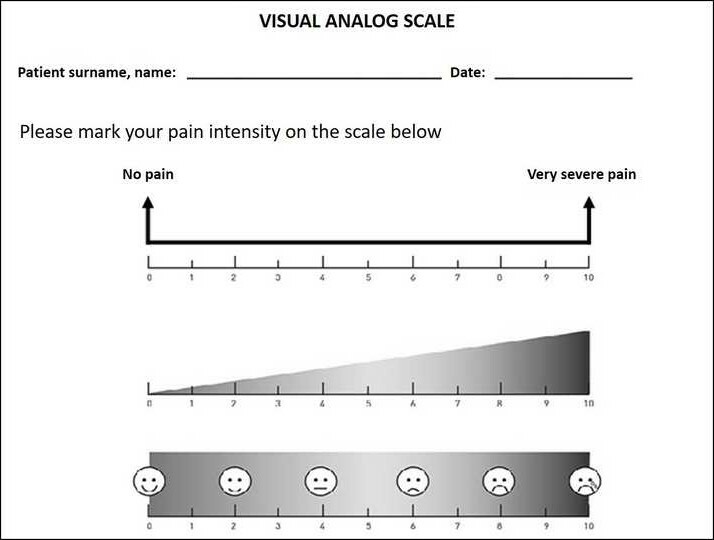
Study Design and SampleThis study was approved by the institutional ethical committee (protocol number: 20.478.486). Written informed consent was obtained from every participant. The study population included patients who applied to otorhinolaryngology outpatient clinic between April 2015 and April 2016 with the complaints of earache, jaw pain, noise in the joint, and/or pain radiating from the jaw to the head, face, and neck, as well as patients with a pre-diagnosis of TMD (other than joint dislocation). Data of all cases including age, sex, physical examination and history of TMD were obtained. Accordingly, a total of 218 patients were enrolled in the study. At first, standard treatment modalities were offered to each of these patients. Patients who refused these modalities for various reasons or patients who were seeking a more practical solution were offered the MCRM option. No imaging examination (radiography, magnetic resonance imaging etc.) was performed on the patients who accepted the maneuver. Patients who did not accept and preferred the standard examination were directed to imaging examination and were not included in the study. Ultimately, target sample consisted of 153 patients who accepted and underwent the MCRM. These 153 patients were divided into two groups according to the duration of their complaints. Those with complaints for a maximum of 10 days were categorized as short-term (group 1), and those for longer than 10 days were categorized as long-term (group 2). The effectiveness of the maneuver was evaluated by comparing the VAS scores of the patients before and after the maneuver (Figure 1). Patients were reexamined 15 days after the maneuver.
 Büyütmek İçin Tıklayın |
Figure 1: Pain-related visual analog scale |
Inclusion criteria for the target sample
i) Patients with a pre-diagnosis of TMD (other than joint dislocation) due to the localization of the symptoms, history of previous dental interventions (extraction, prosthesis, etc.), increased sensitivity in the TMJ, limitation of mouth opening, presence of crepitation, asymmetry in jaw movement, and findings in teeth because of unilateral chewing habits on physical examination
ii) Patients with referred otalgia without any pathology of ear, oropharynx or larynx.
Exclusion criteria
i) Patients with suspected TMJ luxation by history and physical examination
ii) Patients with a non-TMD disease that may cause existing symptoms
iii) Patients with pathologies in other joints or with rheumatological and/or inflammatory diseases and suspected infection
iv) Patients who did not accept the MCRM, instead choosing the standard examination and treatment protocol.
Maneuver technique
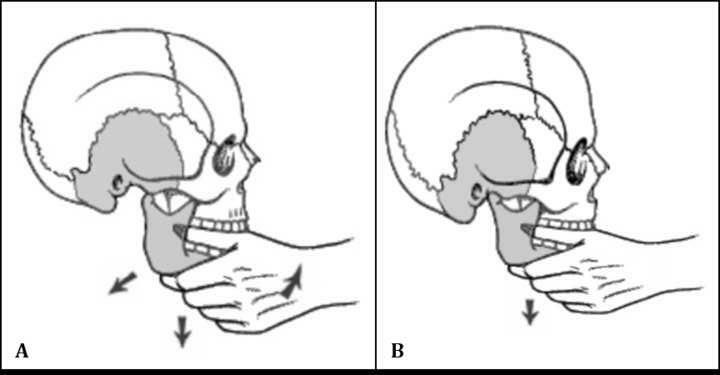
While the patient was in a sitting position, the doctor-after wrapping his thumbs with gauze-placed his thumbs inside the patient"s mouth on the lower posterior teeth, or on the alveolar process if there were no teeth, and grasped the lower jaw with his other fingers. By pressing on the last lower molars or on the retromolar trigone, the doctor gently and quickly pulled the chin down on the axis of the condyle. During pulling, the patient was asked to leave the lower jaw relaxed, not to contract the jaw muscles, and not to allow the head and body to lean forward. The patient was expected to cooperate and maneuver was performed (Figure 2).
 Büyütmek İçin Tıklayın |
Figure 2: A. Traditional closed reduction maneuver, B. Modified closed reduction maneuver |
Statistical analysis
While the data were presented as mean ± standard deviation (SD), the normality test (Shapiro-Wilk test) was used to evaluate the distribution. Comparison of quantitative data was done using the independent sample t-test or the Mann Whitney U and Wilcoxon test, considering the result of the normality test. In-group comparison was done by paired sample t- test. The results were evaluated in a 95% confidence interval and p<0.05 was considered statistically significant. (IBM SPSS Statistics for Windows, Version 21.0.; Armonk, NY, IBM Corp.).
Results
Descriptive dataShapiro-Wilk test results were asymmetric for all data except age (p=0.16 for Group 1, p=0.37 for Group 2) (p<0.05). For this reason, when comparing groups, we used independent samples t-test for age, the Wilcoxon test for VAS, and the Mann Whitney U test for side and gender.
Out of 218 patients with TMD (other than TMJ dislocation), 153 patients [90 females, 63 males; mean age 45.12±17.61] were included in the study. Of these, 94 patients [53 females, 41 males; mean age 35.95±13.31] were included in Group 1 and 59 patients [37 females, 22 males; mean age 59.73±13.23] were included in Group 2. The left side of 80 patients and the right side of 73 patients were affected. The mean age of the group 2 was higher than group 1, and the difference was significant (p<0.001). There was no difference between groups in terms of affected side (p=0.44) and gender (p=0.78) parameters.
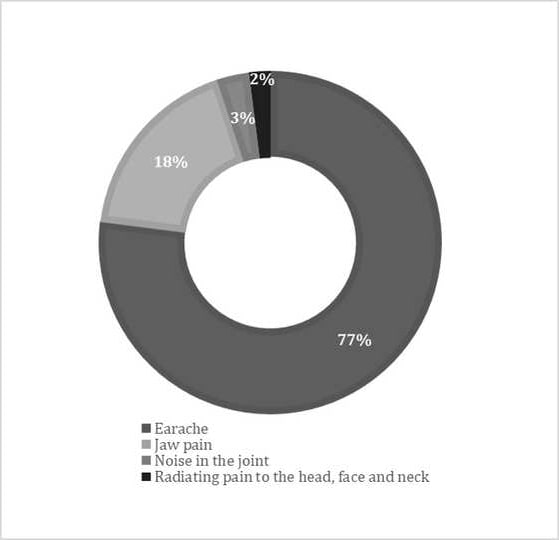
The most common primary complaint at admission was earache (n=119), followed by pain in the jaw joint (n=27), noise in the joint (n=4), and pain radiating from the jaw to the head, face and neck (n=3). We summarized the complaints of the patients in Figure 3.
 Büyütmek İçin Tıklayın |
Figure 3: Pie chart showing distribution of patient complaints |
Comparison of visual analog scale and demographic data
We used the Wilcoxon test to compare VAS scores and observed a significant decrease in the mean VAS scores of all patients after the maneuver (p<0.001) (Figure 4). When patient groups were evaluated separately, pre-maneuver VAS scores were found to be higher than post-maneuver VAS scores (Figure 4). In addition, we found pre-maneuver VAS scores to be significantly higher in group 1 compared to group 2 (p<0.001).
 Büyütmek İçin Tıklayın |
Figure 4: Bar chart showing mean VAS scores of all patients and patient groups before and after the maneuver |
Discussion
In this study, we evaluated pain-related VAS scores of the TMD patients (other than joint dislocation) before and after MCRM, which can be easily applied to patients with TMD in outpatient settings. According to our findings MRCM provides rapid relief from symptoms. We found that this maneuver is particularly effective in reducing or eliminating pain.One of the most assumed factors in the etiology of TMD is occlusion disorders. Loss of maxillary or mandibular posterior teeth also creates an unstable TMJ[13]. We observed that most of the patients in this study had occlusion disorder or tooth loss, especially in the group 2. Mandible hyperextension during long-term and forceful dental applications may also cause trauma to the TMJ and surrounding tissues. Especially applications such as third molar tooth extraction and root canal treatment are known to cause TMD[14]. It was noteworthy that most of our patients in the group 1 had dental applications that caused prolonged opening of the mouth. In the group 2, we think TMD develops secondary to mandibular hyperextension or subsequent malocclusion, especially in elderly patients. We referred our patients, who had TMD secondary to malocclusion and tooth loss, to dentistry because of the possibility of recurrence, even if their symptoms improved after the maneuver.
Temporomandibular diseases are self-limiting pathologies of which symptoms tend to improve over time. There are adaptation mechanisms, such as bone remodeling, TMJ soft tissue metaplasia, and hypoactivity or hyperactivity in the muscles[15]. Despite these mechanisms, symptoms may recur or not be fully controlled. Because of this uncertainty, it is more appropriate to prefer a fast, an easy, and an effective method to relieve the symptoms. As far as we know, MCRM has not been used or defined in any study before. We think that it may be superior to other conservative modalities with easy applicability and rapid relief effect. During the maneuver, especially in the group 1, a sudden relief with a clicking sound on the side of the complaint was observed.
Pain-related VAS is a reliable and valid measurement method for assessing the severity of pain[16]. Considering the VAS scores, we observed a decrease after maneuver in comparisons within and between groups (Figure 4). These findings showed that MCRM was quite effective in pain control. Because of the long treatment period in most of the other conservative treatment methods, adaptation mechanisms may come into play. We think this situation should be considered when evaluating the effectiveness of the other treatments.
The mean age of the group 2 was higher than the group 1 (p<0.001). This may be because of the higher incidence of TMDs due to tooth loss in the elderly. In addition, pre-maneuver VAS scores were higher in the group 1 than in the group 2. It seems that, as the severity of pain increases, the time for admission gets shorter. It can also be asserted that as the disease becomes chronic, the severity of pain decreases with the effect of adaptation mechanisms.
The main treatment modalities for TMD are dental treatments, medication, intra-articular injection, physical therapy, mind-body-based approaches and surgery[17]. Hard/soft stabilization splints, prefabricated splint, mini-anterior splint, anterior reposition splint, and counseling therapy were evaluated in a meta-analysis of 48 randomized controlled studies on occlusal splints, which are the most widely used dental treatments[18]. They stated that there is moderate to low-quality evidence confirming the efficacy of occlusal splint therapy in the treatment of TMD, and that rigid stabilization splint can provide maximum recovery with counseling therapy. However, in another meta-analysis in which 33 randomized controlled studies were evaluated, it was reported that splints provided short-term benefits for patients, and their effects were equalized with other therapeutic methods in long-term follow-up[19]. It has been reported that physical therapy methods are useful in patients with pathology in the masticatory muscles but not in the TMJ[13,20]. The American Academy of Craniomandibular Disorders and the Minnesota Dental Association have also suggested physical therapy as an important treatment modality for relieving musculoskeletal pain, reducing inflammation, and restoring oral motor function[20]. Physical therapy modalities can be listed as superficial and deep hot applications, cold applications, massage, transcutaneous electrical nerve stimulation (TENS), therapeutic exercises, and manual therapy techniques[21]. Although the evidence for these treatments is weak, it has been reported that they are effective in the symptom control of TMD. Furthermore, it can be used alone or in combination with orthodontic, pharmacological, relaxation and/or behavioral treatments[21,22]. Therapeutic exercises are widely used physical therapy methods which are reported to be effective. In one study, patients with TMD associated with localized/regional TMJ pain and diffuse pain were administered a structured supervised exercise program over 10-20 weeks, including 10 sessions of relaxation, coordination of the jaw and neck/shoulders, and resistance training. They revealed reduced pain in terms of jaw pain intensity, time to withstand jaw opening, resistance and protrusion against chewing, and the effects of pain on daily activities[23]. Although this physical exercise program is convenient, it requires time, which makes MCRM superior in this sense.
Manual therapy techniques are somewhat similar to the MCRM. They can be categorized as joint mobilization, manipulation, or treatment of soft tissues. They are used to improve range of motion, reduce local ischemia, stimulate proprioception, break up fibrous adhesions, stimulate synovial fluid production, and reduce pain[24]. However, it has been reported that manual therapy techniques are not superior to occlusal splints[25]. In addition, it was reported that there is a need for several sessions of manual therapies and it would be more effective to combine with therapeutic exercises[26]. This suggested that MCRM would be more appropriate to be applied as the first choice in TMD diseases. However, in a meta-analysis evaluating only 6 randomized controlled studies, it was concluded that manual therapy is effective in the medium term, and the effect can be prolonged when combined with therapeutic exercises[27]. Nevertheless, only in three of these studies manual therapy was applied to the temporomandibular region. Mouth opening was also evaluated in these three studies[28-30]. However, it was reported that the efficacy of the treatment in terms of mouth opening subsides by the 6 month. Therefore, we thought that MCRM might be more effective than manual therapy in terms of pain control.
Concerning the literature, success in the treatment of TMD was defined as i) significant reduction in the severity and frequency of pain, ii) maximum mouth opening of 35 mm, iii) absence of joint sounds[31]. Since it is impossible to eliminate joint sounds, some reduction in joint sounds can also be accepted as a success[32].
As mentioned before, we did not measure maximum mouth opening, objectively. However, the significant reduction in pain and in joint sounds with MCRM shows that it is quite effective. In addition, pain-related VAS scores also demonstrated the effectiveness of MCRM. Another advantage of this maneuver is that it can be combined with other conservative treatments. Furthermore, it has a positive effect on both muscle and joint pathologies. We believe that MCRM is beneficial with mechanisms such as restoring the joint space, correcting the disc displacement if there is any, and reducing the tension by sudden stretching of the muscles. However, there is a need for studies with a long follow-up period and using imaging techniques such as magnetic resonance imaging performed before and after the maneuver. Besides, evaluating some functional parameters of the TMJ, such as painless maximum mouth opening, disability index, and quality of life scales, would increase the strength of our results.
Conclusion
This study showed that the MCRM has positive effects on patients with TMD (other than joint dislocation). This maneuver can be easily applied in outpatient settings and provides fast relieve. It is quite successful in symptom control of TMDs.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
Reference
1) Dahlstrom L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand 2010; 68:80-85. [ Özet ]
2) Lövgren A, Häggman-Henrikson B, Visscher CM, Lobbezoo F, Marklund S, Wänman A. Temporomandibular pain and jaw dysfunction at different ages covering the lifespan--A population based study. Eur J Pain 2016; 20:532-540. [ Özet ]
3) Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6:301-355. [ Özet ]
4) Dworkin SF, Sherman J, Mancl L, Ohrbach R, LeResche L, Truelove E. Reliability, validity, and clinical utility of the research diagnostic criteria for Temporomandibular Disorders Axis II Scales: depression, non-specific physical symptoms, and graded chronic pain. J Orofac Pain 2002; 16:207-220. [ Özet ]
5) Schiffman EL, Truelove EL, Ohrbach R, Anderson GC, John MT, List T, Look JO. The Research Diagnostic Criteria for Temporomandibular Disorders. I: Overview and methodology for assessment of validity. J Orofac Pain 2010; 24:7-24. [ Özet ]
6) Look JO, John MT, Tai F, Huggins KH, Lenton PA, Truelove EL, Ohrbach R, Anderson GC, Shiffman EL. The Research Diagnostic Criteria for Temporomandibular Disorders. II: Reliability of Axis I diagnoses and selected clinical measures. J Orofac Pain 2010; 24:25-34. [ Özet ]
7) Truelove E, Pan W, Look JO, Mancl LA, Ohrbach RK, Velly AM, Huggins KH, LentonP, Shiffman EL. The Research Diagnostic Criteria for Temporomandibular Disorders. III: Validity of Axis I diagnoses. J Orofac Pain 2010; 24:35-47. [ Özet ]
8) Schiffman EL, Ohrbach R, Truelove EL, Tai F, Anderson GC, Pan W, Gonzalez YM, John MT, Sommers E, List T, Velly AM, Kang W, Look JO. The Research Diagnostic Criteria for Temporomandibular Disorders. V: Methods used to establish and validate revised Axis I diagnostic algorithms. J Orofac Pain 2010; 24:63-78. [ Özet ]
9) Look JO, Schiffman EL, Truelove EL, Ahmad M. Reliability and validity of Axis I of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) with proposed revisions. J Oral Rehabil 2010; 37:744-759. [ Özet ]
10) Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, List T, Svensson P, Gonzalez Y, Lobbezoo F, Michelotti A, Brooks SL, Ceusters W, Drangsholt M, EttlinD, Gaul C, Goldberg LJ, Haythornthwaite JA, Hollender L, Jensen R, John MT, De LaatA, de Leeuw R, Maixner W, van der Meulen M, Murray GM, Nixdorf DR, Palla S, Petersson A, Pionchon P, Smith B, Visscher CM, Zakrzewska J, Dworkin SF; International RDC/TMD Consortium Network, International association for Dental Research; Orofacial Pain Special Interest Group, International Association for the Study of Pain: Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: recommendations of the International RDC/TMD Consortium Network* and Orofacial Pain Special Interest Group?. J Oral Facial Pain Headache 2014; 28:6-27.
11) Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, Januzzi E,de Souza BDM. Prevalence of temporomandibular joint disorders: a systematic review and meta- analysis. Clin Oral Investig 2021; 25:441-453. [ Özet ]
12) Cuccia AM, Caradonna C, Caradonna D. Manual therapy of the mandibular accessory ligaments for the management of temporomandibular joint disorders. J Am Osteopath Assoc 2011; 111:102-112. [ Özet ]
13) Al-Baghdadi M, Durham J, Araujo-Soares V, Robalino S, Errington L, Steele J. TMJ Disc Displacement without Reduction Management: A Systematic Review. J Dent Res 2014; 93:37-51. [ Özet ]
14) Cooper BC. Craniomandibular Disorders. In: Cooper BC, Lucente FE, eds. Managementof Facial, Head and Neck Pain, Philadelphia: W.B. Saunders Co, 1989: 153-254.
15) Navi F, Motamedi MHK, Taheri Talesh K, Lasemi E, Nematollahi Z. Diagnosis and Management of Temporomandibular Disorders. In: Motamedi MHK, ed. A Textbook of Advanced Oral and Maxillofacial Surgery, London: IntechOpen, 2013: 10.5772/55018.
16) Bijur PE, Silwer W, Gallagher EJ. Reliability of the Visual Analog Scale for measurement of acute pain. Acad Emerg Med 2001; 8:1153-1157. [ Özet ]
17) Liem T, McPartland JM, Skinner E. Cranial Osteopathy: Principles and Practice. 2nd edition. New York: Elsevier Churchill Livingstone, 2004:418-419.
18) Al-Moraissi EA, Farea R, Qasem KA, Al-Wadeai MS, Al-Sabahi ME, Al-Iryani GM. Effectiveness of occlusal splint therapy in the management of temporomandibular disorders: network meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 2020; 49:1042-1056. [ Özet ]
19) Kuzmanovic Pficer J, Dodic S, Lazic V, Trajkovic G, Milic N, Milicic B. Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of shortand long term effects. PLoS One 2017; 12:e0171296. [ Özet ]
20) Sturdivant J, Fricton JR. Physical therapy for temporomandibular disorders and orofacial pain. Curr Opin Dent 1991; 1:485-496. [ Özet ]
21) McNeely ML, Armijo Olivo S, Magee DJ. A systematic review of the effectiveness of physical therapy interventions for temporomandibular disorders. Phys Ther 2006; 86:710-725. [ Özet ]
22) Murphy GJ. Physical medicie modalitie and trigger point injections in the management of temporomandibular disorders and assessing treatment outcome. Pathol Oral Radiol Endod 1997; 83:118-122. [ Özet ]
23) Häggman-Henrikson B, Wiesinger B, Wänman A. The effect of supervised exercise on localized TMD pain and TMD pain associated with generalized pain. Acta Odontol Scand 2017; 4:1-7. [ Özet ]
24) Mujakperuo HR, Watson M, Morrison R, Macfarlane TV. Pharmacological interventions for pain in patients with temporomandibular disorders. Cochrane Database Syst Rev 2010; 10:CD004715. [ Özet ]
25) Melo RA, de Resende CMBM, Rêgo CRF, Bispo ASL, Barbosa GAS, de Almeida EO. Conservative therapies to treat pain and anxiety associated with temporomandibular disorders: a randomized clinical trial. Int Dent J 2020; 70:245-253. [ Özet ]
26) Gil-Martínez A, Paris-Alemany A, López-de-Uralde-Villanueva I, La Touche R. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res 2018; 11:571-587. [ Özet ]
27) Herrera-Valencia A, Ruiz-Muñoz M, Martin-Martin J, Cuesta-Vargas A, González- Sánchez M. Efficacy of Manual Therapy in Temporomandibular Joint Disorders and Its Medium-and Long-TermEffects on Pain and Maximum Mouth Opening: A Systematic Review and Meta-Analysis. J Clin Med 2020; 9:3404. [ Özet ]
28) Craane B, Dijkstra PU, Stappaerts K, De Laat A. Randomized controlled trial on physical therapy for TMJ closed lock. J Dent Res 2012; 91:364-369. [ Özet ]
29) Kalamir A, Bonello R, Graham P, Vitiello AL, Pollard H. Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: A randomized controlled trial. J Manip Physiol Ther 2012; 35:26-37. [ Özet ]
30) Nagata K, Hori S, Mizuhashi R, Yokoe T, Atsumi Y, Nagai W, Goto M. Efficacy of mandibular manipulation technique for temporomandibular disorders patients with mouth opening limitation: A randomized controlled trial for comparison with improved multimodal therapy. J Prosthodont Res 2019; 63:202-209. [ Özet ]
31) Goss AN. Toward an international consensus on temporomandibular joint surgery.Report of the Second International Consensus Meeting, April 1992, Buenos Aires, Argentina. Int J Oral Maxillofac Surg 1993; 22:78-81. [ Özet ]




