ENDOSCOPIC TRANSCANAL PALISADE CARTILAGE MYRINGOPLASTY TECHNIQUE: EARLY FINDINGS
Summary
Purpose of this study was to decrease the morbidity of cartilage palisade myringoplasty by using otoendoscopy for different sized perforations. In total, 32 patients were enrolled in this study operated between March 2015 and December 2017. All the patients were operated through a transcanal approach with endoscope to decrease postoperative morbidity. Perichondrium on both sides of the cartilage palisades and some connective tissue were preserved to increase the viability of the cartilages. Endoscopes provide good exposure of the TM, without canalplasty. Graft success was observed in 30 patients (%93.7). There was a significant change of air-bone gap (p< 0.001). Mean Air Bone Gap (ABG) values decreased postoperatively, and this decrease was statistically significant (p<0.001). Endoscopic transcanal myringoplasty technique has excellent success rates and low morbidity.Introduction
Myringoplasty is one of the most commonly performed operations by otolaryngologists. Different types of techniques and autologous grafts have been well defined in the literature. Cartilage use for tympanic membrane perforations has been advocated in many studies in the literature[1-3]. Studies have shown the benefits of using cartilage such as low recurrence, better graft survival and low infection rates[3-5]. There are many reported cartilage myringoplasty techniques like palisade, composite, diced cartilage, butterfly, mosaic, and Heermann-Tos Chat technique[1-10]. A postauricular incision increases visibility of the tympanic membrane, whereas the transcanal approach is mostly performed for patients with small tympanic membrane perforations and a wider ear canal[11]. For this reason, microscopic myringoplasty with the postauricular approach has become the preferred method worldwide[11]. However, this technique requires postauricular incision which increases postoperative morbidity[11].According to Tos, there are 23 different cartilage myringoplasty methods and he grouped them into six groups from A to F[12]. The palisade cartilage technique (PCT) was categorized by him as Group A cartilage tympanoplasty[12]. Definition of the PCT is the placement of pieces of cartilage slightly overlapping each other like shingles under the TM remnant until the perforation is closed totally. The technique was described by Heermann and proposed as the better technique to treat recurrent defects of TM[13].
There are recent studies showing the efficacy of endoscopic transcanal cartilage tympanoplasty technique using butterfly grafts[14]. It has been also shown that perichondrium is essential for the survival of cartilage, so we have decided to preserve the perichondrium on both sides. By this study we wanted to present our endoscopic transcanal PCT experience and the success of our method.
Methods
This retrospective study included 28 patients who have dry tympanic membrane perforations for more than 6 months between March 2015 and December 2017. Patients with marginal perforations, cholesteatoma and discharging ears were excluded from the study. We collected the data from the Medin medical software system (Medin Software, 4T Inc., İstanbul, Turkey). The study protocol was approved by the ethics committee of the Liv Hospital Ankara Hastanesi and conducted in accordance with the ethical principles of the Declaration of Helsinki. A written informed consent was obtained from all patients before the study.Patients are divided into two groups based on the sizes of TMP. Small perforation group consisted of the patients who have 4 mm diameter or smaller perforations and large perforation group consisted of the patients who have larger than 4 mm diameter of perforations. The hearing status was evaluated by laminar audiometry (considering the frequencies 0.5-1-2-3-4-8 kHz). ABG were evaluated before surgery and 3 months and one year after the surgery.
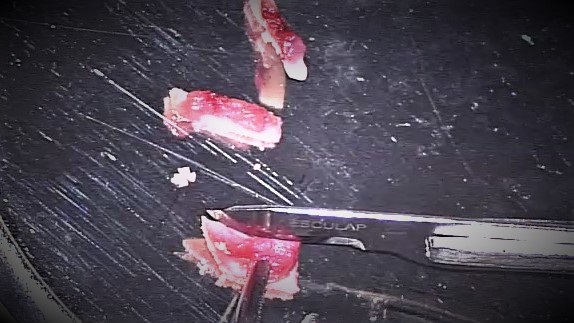
All the surgeries were performed by a single surgeon. PCT with transcanal endoscope assisted approach was used for all the operations. Tragal cartilage was preferred in this study because of its relatively flat shape as opposed to the concave shape of the conchal cartilage. Tragal cartilage was harvested through a 1 cm incision on the medial side of the tragus. While harvesting the cartilage, some connective tissue was obtained adhered to lateral side of the cartilage (Figure 1). 2-mm cartilage strip was left to prevent cosmetic disturbances. Cartilage grafts were prepared by preserving the perichondrium on both sides. The cartilage graft was cut into cartilage palisades with a number 15 blade.
 Büyütmek İçin Tıklayın |
Figure 1: Appearance of tragal cartilage palisades with connective tissue over the lateral surface |
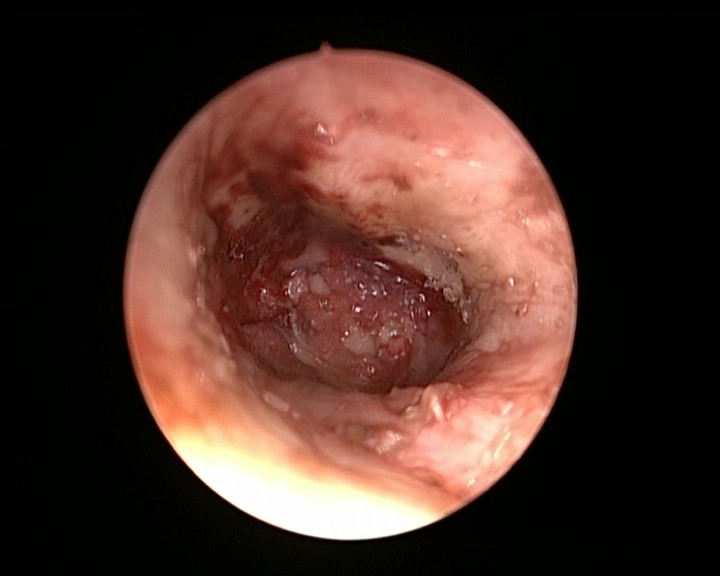
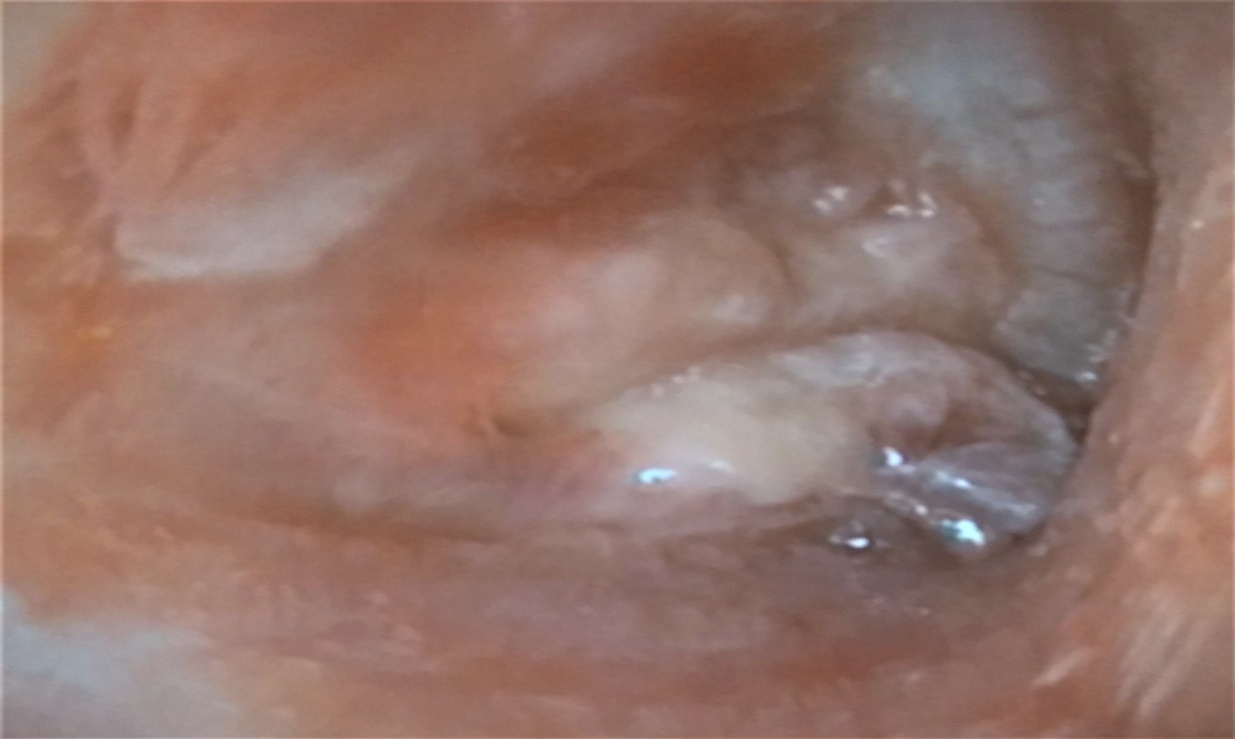
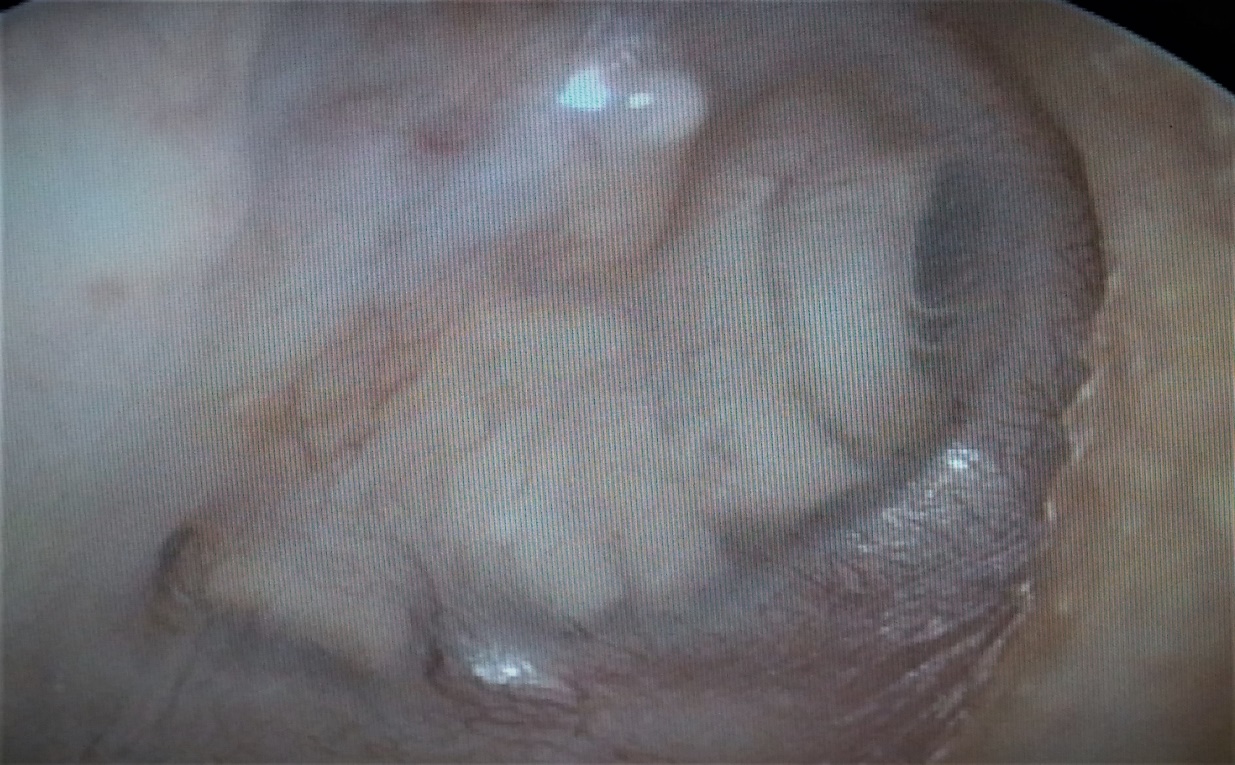
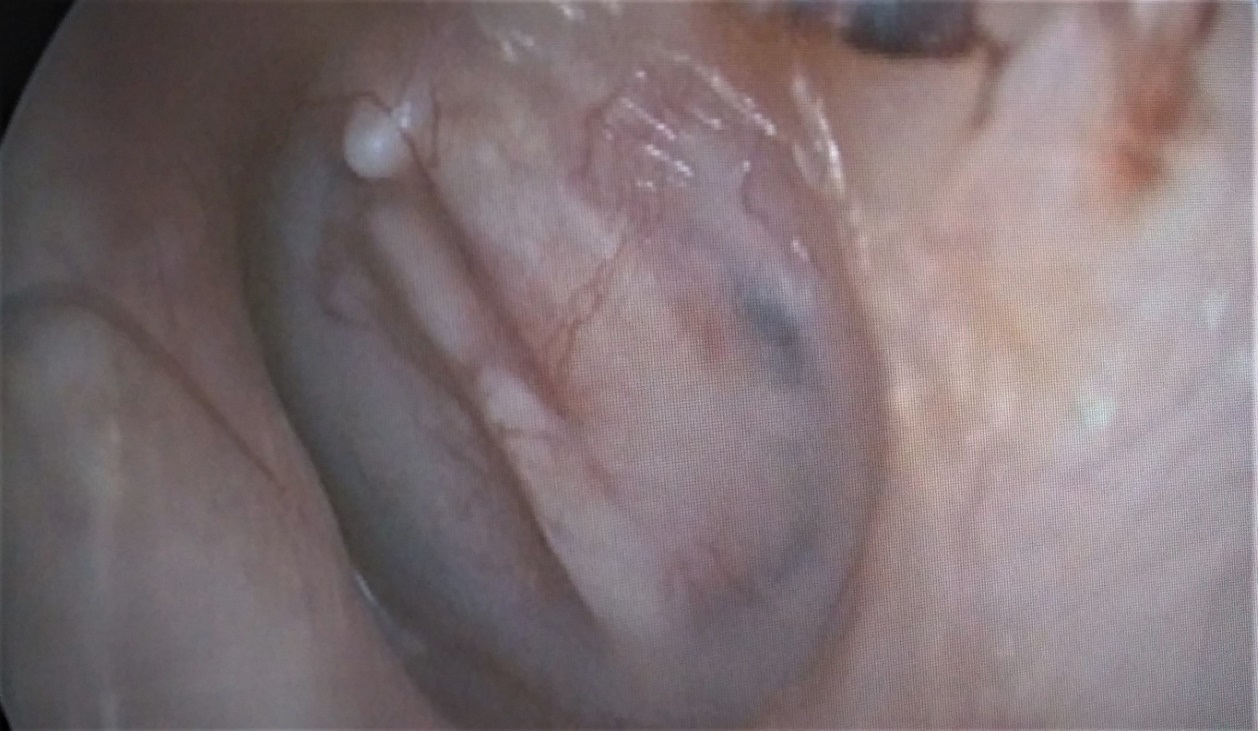
Two rigid Karl Storz endoscopes were used for the surgeries (4.0-mm, 0°, 18-cm long lens and 3-mm, 0°, 14-cm long lens; Karl Storz, Tuttlingen, Germany). A 1 mm strip of perforation edges removed to get a fresh edge. Tympanomeatal flap was not raised and the myringoplasty was performed with the over-underlay technique. Malleus was deepithelized when operating large perforations. Gelfoam bed was prepared to prevent medial displacement. Cartilage palisades were placed parallel to the manubrium mallei from the superior to the inferior direction under the tympanic membrane remnant and over the manubrium. Smaller palisades were used for small perforations. Since we used endoscope for operation, no canalplasty was performed. Connective tissue on the lateral side of palisades were used to fill the spaces between the palisades (Figure 2,3). Connective tissue provided additional support for the palisade segments. To prevent lateral displacement of graft, small pieces of gelfoam placed over the palisades. External ear canal was packed with gelfoam and a cotton ball removed 7 days later. Patients were examined with otoendoscopes for the graft success 7 days, 1 month, 6 months and 1 year following surgery (Figure 4,5).
 Büyütmek İçin Tıklayın |
Figure 2: Intraoperative appearance of placed palisades with connective tissue filling the spaces between palisades |
 Büyütmek İçin Tıklayın |
Figure 3: Postoperative first month appearance of covering connective tissue over the palisades |
 Büyütmek İçin Tıklayın |
Figure 4: Postoperative first year appearance of large perforation closed with palisades |
 Büyütmek İçin Tıklayın |
Figure 5: Postoperative first year appearance of small perforation closed with palisades |
Statistical analysis was performed with the Statistical Package for the Social Sciences 22.0 software package (SPSS Inc.; Chicago, IL, USA). For pre- and post-operative data measurement, the difference was analyzed for abnormal distribution with the Wilcoxon signed-rank test; Paired samples t-test was used if suitable for normal distribution. P values less than 0.05 were considered statistically significant. The relationship between categorical variables was analyzed using Fisher's exact test.
Results
Twenty-eight patients were enrolled in the study. Four of them were operated bilaterally and 32 surgeries were performed in total. Fifteen (53.6%) male, 13 (46.4%) female patients were treated. (18 on right side and 14 on left side) The mean age of patients was 34.5 ± 12.3 years with a range of 11-53 years. The mean follow-up period was 23.3 ± 9.4 months (range 12-30 months). Table 1 summarizes the perforation sizes and characteristics of the patients.Table 1: Characterizations of the patients, perforations and pre-postoperative ABGs.
As a laterality, 18 (56.2%) right, and 14 (43.8%) left ears were operated. The overall graft success was observed postoperatively at 1 month in 30 of 32 cases (93.7%). Two failures and reperforations were occurred as a resorption of one palisade segment. One failure was in small perforation group and the other one was in large perforation group. Total perforation or resorption of two or more segments of palisades was not observed. Reperforations were seen within 3 months after surgery. Reperforations were operated with the same technique and closed successfully one after 4 months and the other one after 6 months following primary surgery. Follow-up of reintervention was successful after one year. Facial nerve or ossicular chain related complications were not occurred postoperatively.
The mean ABG decreased from 24.4 ± 3.21 (mean ± SD) to 14.3±6.28 (mean ± SD) and this decrease was statistically significant (p<0.001). There was no significant correlation between the preoperative and postoperative ABG and the size of the TMP.
Discussion
Myringoplasty or type 1 tympanoplasty has been the only surgery for closuring tympanic membrane perforations. Since its introduction, temporalis muscle fascia is still the first choice of otologists all around the world[15]. There are many reported studies showing high success rates with traditional tympanoplasty technique using temporalis muscle fascia. However, there are several disturbing disadvantages such as postauricular incision and possible need for canalplasty when performing the traditional method.Cartilage has been used in otologic surgeries, and the material is known for its resistance to infection, resorption, and retraction much more than fascia which has been proved by many studies in the literature[1-10]. The use of cartilage palisades as tympanic membrane grafts was described by Heermann[13]. He advocated that slicing the cartilage graft would prevent the torsion associated with a single large piece of cartilage graft[13]. Intact perichondrium is critical for long term survival of the cartilage graft through diffusion[16]. The perichondrium also connects with the perichondrium of the adjacent palisade via tissue fluid[16]. Early studies used additional perichondrial or fascia grafts over the palisades for union and epithelialization[13]. In this study, while harvesting the cartilage, some connective tissue was obtained adherent to lateral side of the cartilage to promote the attachment of palisade segments together. Traditionally, otologists usually strip off the perichondrium on the medial side of the palisades to prevent possible adhesions. In this study, we preferred to keep the medial perichondrium intact to increase the viability and diffusion ability of cartilage palisades.
Many studies have examined the functional and graft success outcomes of the PCT technique[2-4,10]. All the studies showed that there is no significant difference in the hearing results between PCT technique and temporalis fascia technique[2-4,10].
Recently, endoscopic techniques have been introduced to the otology practice especially for cholesteatoma surgery[17]. Also, several studies showed the efficacy of endoscopes as complimentary devices to microscopes for myringoplasty procedure[18-20]. All the studies have agreed that endoscopic approach in otology is practical, minimally invasive when compared to the traditional surgical approaches[18-20]. Tympanoplasty has a high success rate, but elevation of the tympanomeatal flap may cause significant tissue damage. Since there are limited incisions than the traditional techniques, there will be no disturbance in the external ear blood circulation[18-20]. Publications on endoscopic myringoplasty have been conducted on small, central perforations and mostly using temporalis muscle fascia[18-20]. Ayache performed transcanal cartilage myringoplasty technique for different sized perforations and the success rate was 96%[14].
In this study, graft success rate after one month was 93.7%. Reperforation, medialization or medial adhesion was not observed first year following the surgery. Studies regarding endoscope-assisted myringoplasty showed the success rates range between 80% and 96%[14,18-20]. However, endoscopic technique has been used for small perforations with different graft materials but cartilage palisades have not been used for this purpose (aponeurosis, fat, cartilage)[14,18-20]. In the current study, different sized perforations were operated with microscope assisted endoscopic technique. For small perforations, smaller sized palisades were used to close the perforations (Figure 4).
For anterior perforations, transcanal drilling of the anterior portion of the bony canal may be required if there is overhang of anterior bony canal. Endoscope gives good exposure without drilling. Because endoscopic surgery is a one-handed technique, bleeding often interrupts the surgery. In this study, local adrenalin administration with cotton balls effectively controlled bleeding. Epithelium attached to the handle of the malleus was carefully dissected out to prevent formation of cholesteatoma.
All patients were discharged the day after surgery. Since there are no incisions, postoperative wound care, bleeding and pain were not observed.
Reference
1) Dornhoffer J. Cartilage tympanoplasty: indications, techniques, and outcomes in a 1,000-patient series. Laryngoscope. 2003;113(11):1844-1856. [ Özet ]
2) Gun T, Boztepe OF, Atan D, İkincioğulları A, Dere H. A Comparison of Cartilage Palisades and Temporal Fascia in Type 1 Tympanoplasty for Bilateral Tympanic Membrane Perforations in Children. J Int Adv Otol. 2017;13(1):36-39. [ Özet ]
3) Cabra J, Monux A. Efficacy of cartilage palisade tympanoplasty: Randomized controlled trial. Otol Neurotol. 2010;31(4):589-595. [ Özet ]
4) Neumann A, Schultz-Coulon HJ, Jahnke K. Type III tympanoplasty applying the palisade cartilage technique: a study of 61 cases. Otol Neurotol. 2003; 24 (1): 33-37. [ Özet ]
5) Vashishth A, Mathur NN, Choudhary SR, Bhardwaj A. Clinical advantages of cartilage palisades over temporalis fascia in type I tympanoplasty. Auris Nasus Larynx. 2014;41(5):422-427. [ Özet ]
6) Klacansky J. Cartilage myringoplasty. Laryngoscope. 2009;119(11):2175-2177. [ Özet ]
7) Chen XW, Yang H, Gao RZ, Yu R, Gao ZQ. Perichondrium/cartilage composite graft for repairing large tympanic membrane perforations and hearing improvement. Chin Med J. 2010;123(3):301-304. [ Özet ]
8) Yung M. Cartilage tympanoplasty: literature review. J Laryngol Otol. 2008;122(7):663?672. [ Özet ]
9) Neumann A, Jahnke K. Reconstruction of the tympanic membrane applying cartilage: indications, techniques and results. HNO. 2005;53(6):573-584. [ Özet ]
10) Uzun C, Yağız R, Taş A, Adali MK, Koten M, Karasalihoglu AR. Combined Heermann and Tos (CHAT) technique in cholesteatoma surgery: surgical technique and preliminary results. J Laryngol Otol. 2005;119(6):429-435. [ Özet ]
11) Jako GJ. Postaural versus endaural exposure in tympanoplasty. Laryngoscope. 1967;77(11):2022-2031. [ Özet ]
12) Tos M. Cartilage tympanoplasty. New York: Thieme Medical Publishers, 2009.
13) Heermann J, Heermann H, Kopstein E. Fascia and cartilage palisade tympanoplasty: nine years" experience. Arch Otolaryngol. 1970;91(3):228-241. [ Özet ]
14) Ayache S. Cartilaginous myringoplasty: the endoscopic transcanal procedure. Eur Arch Otorhinolaryngol. 2013;270(3):853-860. [ Özet ]
15) Storrs L. Myringoplasty with the use of fascia grafts. Arch Otolaryngo Head Neck Surg. 1961;74(2):45-49.
16) Davidson M. A study of the fate of autogenous cartilage grafts. Laryngoscope. 1959;69:1259-1277. [ Özet ]
17) Tarabichi M. Endoscopic management of limited attic cholesteatoma. Laryngoscope. 2004;114(7):1157-1162. [ Özet ]
18) Yadav SP, Aggarwal N, Julaha M, Goel A. Endoscope assisted myringoplasty. Singap Med J. 2009;50(5):510-512. [ Özet ]
19) Karkuheto TS, Ilomaki JH, Puhakka HJ. Tympanoscope assisted myringoplasty. ORL J Otorhinolaryngol Relat Spec. 2001;63(6):353-357. [ Özet ]
20) El-Guindy A. Endoscopic transcanal myringoplasty. J Laryngol Otol. 1992;106(6):493-495. [ Özet ]




