THE INFLUENCE OF SMOKING ON SURGICAL SUCCESS IN TYMPANOPLASTY
2Balıklıgöl Devlet Hastanesi, KBB, Şanlıurfa, Turkey
Summary
Background: To investigate the impact of hookah smoking and cigarette smoking on graft success rate and hearing outcomes in patients undergoing cartilage tympanoplasty.Material and Methods: The case group was constituted from patients whose cartilage tympanoplasty operations led to re-perforation, while the control group was constituted of patients with successful post-operative results.
Results: Case and control groups were found to be similar in terms of baseline characteristics. Hookah and cigarette smoking were found to be more frequent in the case group compared the control group. Those smoking both cigarettes and hookah were found to have worse surgical outcomes compared to those smoking either cigarettes or hookah.
Conclusions: Both cigarette and hookah smoking lead to impairment in surgical success after cartilage tympanoplasty. Thus, it is evident that urging patients to quit hookah use and smoking is critical -at least before surgery. However, our results should be confirmed by further studies.
Introduction
Since the initial experiences reported by Wullstein and Zoellner, tympanoplasty constitutes the most influential surgical treatment modality in the management of chronic ear disease.[1,2] Simply put, tympanoplasty is the establishment of an adequate sound-conducting mechanism through the reconstruction of the sound conduction apparatus in a well-aerated, mucosal lined middle ear cleft.[3] However, even in experienced hands, several factors limit the success of tympanoplasty which is typically defined as the take rate of grafts.[4]Without doubt, smoking adversely affects almost all tissues, organs and systems in the human body and still remains as the leading cause of preventable morbidity and mortality worldwide.[5] Current evidence concerning the direct negative effects of cigarette smoking on graft take rates in tympanoplasty are clear.[6] Cigarette smoking has also been associated with increased severity of middle ear disease in preoperative evaluations.[7] Therefore, extensive surgery is often required in smokers to overcome the disease and its results.
Hookah smoking is traditional in the Middle East and has gained popularity, particularly among the younger age groups[8]. Nemati et. al reported that , the prevalence of current daily tobacco use in Iranian, including cigarette and hookah, was estimated 23.7% for men and 3.0% for women.[9] The immigration wave resulting from the civil war in Syria has led to an increase in the popularity of hookah among persons in North America and Europe;[10] however, since the majority of immigrants have settled in Turkey (especially our region in the south-east of Turkey), their cultural habits have found wider acceptance; thus increasing the frequency of hookah smoking. The data addressing the role of hookah smoking in ear diseases and particularly in graft take rates in tympanoplasty are lacking. Recently, we have observed that tympanoplasty success rates have dropped among our patients, and we have hypothesized that this was associated with the increase in the frequency of hookah smoking.
The present study was conducted with an aim to investigate the impact of hookah smoking on graft success rate and hearing outcomes in tympanoplasty, and to compare the effects of hookah smoking and cigarette smoking in this regard.
Methods
Study design and patient inclusionThis study was carried out with the approval of the Ethics Committee of Harran University Faculty Of Medicine on 28/08/2019 with the following approval number: E-35547. Informed consent was obtained from all individual participants included in the study.
The present case-control study was conducted on 71 patients who underwent cartilage tympanoplasty at our tertiary referral center from January 2015 to April 2019. Patients with chronic diseases, those using regular medication, individuals who were ex-smokers, and patients who had a history of ear discharge within the last two months were excluded from the study. A homogeneous group was formed from young adults and the adult age group without any substance use except for smoking and hookah.
We performed power analysis using the frequencies reported in the study conducted by Becvarovski and colleagues.[11] At a level of 5% alpha error, 80% power and enrollment ratio of 1:3, it was found that the case group should be comprised of at least 16 patients, while the control group should include at least 48 patients. We set the enrollment ratio as 1:3 in order to account for the population-based frequency of smoking and to normalize variations in the control group that could be associated with passive exposure to smoking.
Patients who were operated in the ENT and Head and Neck Surgery Clinic of University of Health Sciences Mehmet Akif İnan Training and Research Hospital were included in the study. Patients were grouped according to success status after typmanoplasty. The case group consisted of patients who failed after their tympanoplasty operation, while the control group consisted of patients who had successful tympanoplasty.
Surgery
All surgical procedures were carried out by the same primary surgeon and the same surgical team. The surgical technique used in these procedures was the over-under tympanoplasty technique and tragal cartilage was used as graft material. In all patients, the tympanomeatal flap was elevated through the transcanal approach and the under-overlay graft from tragal cartilage was laid. The procedure was as follows: under general anesthesia, the patients were placed in the appropriate position and the operation site was cleaned and covered with respect to aseptic technique. The tympanomeatal flap was elevated with a transcanal approach under the microscope. The site was kept clean using adrenaline-impregnated thrush for bleeding control. The ossicular chain was checked to ensure that it was intact. Then, grafts of appropriate size were taken from tragal cartilage. Tragus was repaired with the appropriate procedures as per anatomic requirements. The graft was prepared and allowed to dry. The spongel was placed in the middle ear under the microscope and the graft was laid under-overlay. The operation was terminated without complications by supporting with lateral spongel.
Data collection
Detailed history concerning patients" cigarette or hookah smoking habits were obtained. All patients underwent a pure tone audiogram from 250 Hz to 8 KHz before and 6 months after the initial procedure. Audiological data were obtained and reported in accordance with the recommendations of the American Academy of Otolaryngology Committee on Hearing and Equilibrium. The tympanic membrane was inspected with an otomicroscope to assess surgical success and graft failure 6 months after tympanoplasty. Complete take of the graft at least 6 months after surgery was defined as surgical success and detection of perforation or atelectasis was defined as surgical failure. The primary outcome measures were the difference in hearing outcomes and surgical success among non-smokers, cigarette smokers or hookah smokers which were all evaluated 6 months after their respective surgeries.
Perforation type was divided into two groups, central and marginal. Perforation size was also assessed in two groups, small-moderate and large.
Smokers were defined as those who smoked at least 10 cigarettes per day for the last year. Hookah smokers were defined as those who reported hookah smoking at least 3 times a week for the last year. Those who consumed both (defined as at least 5 cigarettes a day and at least 2 hookahs a week) were the final group.
Statistical analysis
Statistical analyses were carried out using SPSS for Windows, version 17 (SPSS, Chicago, IL, USA). Distribution of quantitative variables were studied with the Kolmogorov-Smirnov test with Lilliefors correction. Continuous variables were given as mean ( standard deviation (SD)) and categorical variables as number (n) and percentage (%). Continuous variables which conformed to normal distribution were compared among groups using the Student t-test. The changes in hearing outcomes and surgical success from baseline to postoperative 6th months were compared with the paired samples t-test. Categorical variables were compared using chi-square tests. The Fisher's exact test was used to study the categorical differences between cigarette or hookah smoking and surgical outcome. Two-sided P ≤ .05 was interpreted to be statistically significant.
Results
The mean age of the study group was SD 29.83 (7.38) years. Case and control groups were found to be similar in terms of baseline characteristics including age (P= .084), gender (P= .628), perforation type (P= .229), perforation size (P= .142) and pre-operative hearing level (P= .484) (Table 1).Table 1: Baseline characteristics of the case and control groups
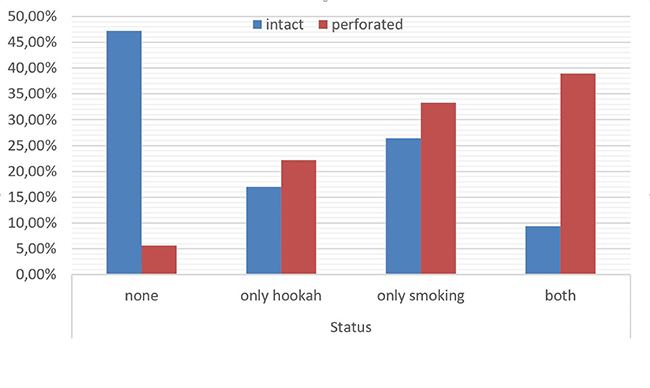
The frequency of smoking in the case group was 72.2%, while this value was 35.8% in the control group (P = .007). The frequency of hookah use in the case group was significantly higher compared to control group (61.1% vs 26.4%, P = .008). When compared to controls, only cigarette smokers and only hookah smokers had lower surgical success rates (P = .007 and P = .008, respectively). When we compared all smoking statuses with each other, those who reported both types of smoking (cigarettes and hookah) were also found to demonstrate a significant decrease in surgical success (P =.003). Among the 18 cases that had perforation, 7 patients had reported both types of smoking; whereas, only one of these patients did not have any history of smoking (Table 2, Figure 1).
Table 2: The status of substance use of case and control group
 Büyütmek İçin Tıklayın |
Figure 1: Comparison of primary surgery results with regard to smoking status groups |
Discussion
The present study demonstrates that cigarette smoking and hookah smoking lead to impairment in surgical success rate to a similar extent in patients undergoing cartilage tympanoplasty. Our findings indicate that surgical success rate was lowest in the subgroup consisting of patients smoking both cigarettes and hookah; whereas, success was highest in the non-smoker subgroup. Thus, although the number of patients in this study was low, it seems that smoking impairs hearing outcomes irrespective of the type of substance smoked.Several factors have been shown to influence graft take and surgical success rates in patients undergoing tympanoplasty. Disease severity, eustachian tube function and the condition of the residual ossicular chain have been recognized as the intrinsic factors associated with the actual severity of the disease and the status of the anatomical structures.[12] The adversities associated with cigarette smoking in tympanoplasty have been studied extensively. The particulate matter and the gas phase chemicals produced by tobacco smoke have been accused of various local and regional changes in the middle ear cleft and eustachian tube. In relation with these effects, it has been shown that patients with persistent otitis media have significant decline in ciliary beating frequency, velocity, and quantity of the mucous flow in the eustachian tube and the middle ear,[13] which are changes that may also be seen in smokers. Smoking also promotes the metaplasia of the middle ear cleft epithelium to a highly secretory type, and thus leads to an increase in the quality and quantity of the mucus.[14] In addition, mast cell-degranulation in adenoidal and lymphoid tissue due to smoking might give rise to the development of eustachian tube obstruction, which may, in turn, deteriorate the phagocytic defense mechanisms of the peritubal tissues, resulting in bacterial colonization in the eustachian tube.[15] Beyond the mentioned local and regional unfavorable changes, cigarette smoking also complicates the perioperative and postoperative period through its influence on the respiratory system. Severe coughing and other manifestations of smoking due to bronchitis, emphysema and asthma, might lead to graft dislocation during and after extubation. Furthermore, these local, regional and systemic elements may result in chronic suppurative ear which is associated with unfavorable surgical outcomes.
The relationship between smoking and hearing loss has also been subject to some research. Nakanishi et al. have demonstrated in 1554 non-hearing-impaired subjects that cigarette smoking was strongly correlated with the development of high-frequency hearing impairment.[16] Similar to these findings, in a retrospective cross-sectional study conducted by Sharabi et al., the incidence of hearing loss unrelated to noise exposure was found to be higher in cigarette smokers than non-smokers.[17]
Available data concerning the impact of smoking on postoperative surgical outcomes for tympanoplasty remains controversial. While some evidence indicates that cigarette smoking adversely affects surgical success, others have found that individual characteristics including smoking status had no impact on surgical outcomes and suggested the experience of surgeons as the leading prognostic factor on graft take.[18,19] In the same studies, surgical technique and graft materials were also shown to be influential on postoperative outcomes. Coelho et al. demonstrated in 128 patients that cartilage tympanoplasty provides comparable success rates and hearing outcomes in both smokers and non-smokers.[19] The authors concluded that the use of thicker cartilage grafts were likely to exert stronger resistance to the negative middle air pressure and consequently prevent atelectasis and adverse reactions.
Hookah tobacco smoking is gaining popularity among European and North American youth, most probably due to the increase in immigration rates within the last few years.[20] Recent data indicates that hookah smoking is associated with short- and long-term adverse health outcomes. Hookah smoke consists of various gases and particles, including glycerol, nicotine, tobacco-specific nitrosamines, carbon monoxide and polyaromatic hydrocarbons, which are similar to the content of cigarette smoke.[21] The chemical similarities between hookah smoke and cigarette smoke sufficiently explain the role of hookah smoking in coronary artery disease, chronic lung disease, altered immunity and malignancies.
Despite the considerable amount of data concerning the role of cigarette smoking on surgical success rate and hearing outcomes in patients undergoing tympanoplasty, data regarding the influence of hookah smoke in these subjects are limited. Nevertheless, the similarities in the gas and chemical content of hookah smoke and cigarette smoke give rise to the thought that these two substances would have similar impact on graft take rates in tympanoplasty. Our findings show that the surgical success rate in non-smokers is higher than that of hookah smokers and cigarette smokers. However, some studies have failed to show significant differences in surgical success rates with regard to smoking status. As shown in the study of Coelho et al., implementation of cartilage grafts which are resistant to the adverse effects of cigarette smoking might be responsible for the lack of difference in surgical success rates that have been reported in the aforementioned studies.[19] The results drawn from our study shows that hookah smoking is similar to cigarette smoking; however, those reporting both types of smoking seem to have even lower levels of success. To the best of our knowledge, the present study is the first to demonstrate adverse outcomes associated with hookah smoking following cartilage tympanoplasty.
There are some limitations to be mentioned. We did not use a prognostic scale in the determination of surgical success but utilized otomicroscopic evaluation. Lack of detailed information concerning the type of cigarette and hookah products, and the absence of data regarding the composition of hookah mixtures (due to lack of standardization of these products) are other limitations of this study. Finally, the lack of quantitative measurement of cigarette smoking intensity with urinary cotinine levels is also a limitation for this study. These results, therefore, need to be interpreted with caution.
In conclusion, hookah smoking leads to a significant impairment (similar to cigarette smoking) in surgical success rate compared to non-smokers in subjects undergoing tympanoplasty. In addition, despite the fact that statistical comparisons among subgroups were not possible due to limited patient numbers in these subgroups, it seems that smokers of both cigarettes and hookah seem to have an even greater decline in surgical success. We suggest that patients who are scheduled for tympanoplasty should be made aware that hookah smoking has similar effects with cigarette smoking, and therefore, should (at the least) be discontinued before and shortly after surgery.
FUNDING
This study was not supported by any institution.
DECLARATION OF INTERESTS
The authors declare no conflict of interest.
Reference
1) Wullstein H. Technic and early results of tympanoplasty. Monatsschr Ohrenheilkd Laryngorhinol. 1953;87(4):308-311. [ Özet ]
2) Zoellner F. Operations for the improvement of the hearing. Triangle. 1960;4:126-131. [ Özet ]
3) Kapadiya M, Tarabichi M. An overview of endoscopic ear surgery in 2018. Laryngoscope Investig Otolaryngol. 2019;4(3):365-373. [ Özet ]
4) Zhao YX, Yu LS. The application of cartilage in middle ear surgery. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2018;32(24):1912-1916. [ Özet ]
5) Campia U, Gerhard-Herman M, Piazza G. Peripheral Artery Disease: Past, Present, and Future. Am J Med. 2019. [ Özet ]
6) Kyrodimos E, Stamatiou GA, Margaritis E. Cartilage tympanoplasty: a reliable technique for smokers. Eur Arch Otorhinolaryngol. 2014;271(2):255-260. [ Özet ]
7) Etzel RA, Pattishall EN, Haley NJ . Passive smoking and middle ear effusion among children in day care. Pediatrics. 1992;90(2 Pt 1):228-232. [ Özet ]
8) Gardner K, Kearns R, Woodland L. A Scoping Review of the Evidence on Health Promotion Interventions for Reducing Waterpipe Smoking: Implications for Practice. Front Public Health. 2018;6:308. [ Özet ]
9) Nemati S, Rafei A, Freedman N, Fotouhi A, Asgary F, Zendehdel K. Cigarette and Water-Pipe Use in Iran: Geographical Distribution and Time Trends among the Adult Population; A Pooled Analysis of National STEPS Surveys, 2006?2009. Arch Iran Med.. 2017;20(5): 295-30. [ Özet ]
10) Waziry R, Jawad M, Ballout RA. The effects of waterpipe tobacco smoking on health outcomes: an updated systematic review and meta-analysis. Int J Epidemiol. 2017;46(1):32-43. [ Özet ]
11) Becvarovski Z, Kartush JM. Smoking and tympanoplasty: implications for prognosis and the Middle Ear Risk Index (MERI). Laryngoscope. 2001;111(10):1806-1811. [ Özet ]
12) Neudert M, Zahnert T. Tympanoplasty - news and new perspectives. GMS Curr Top Otorhinolaryngol Head Neck Surg. 2017;16:Doc07. [ Özet ]
13) Agius AM, Smallman LA, Pahor AL. Age, smoking and nasal ciliary beat frequency. Clin Otolaryngol Allied Sci. 1998;23(3):227-230. [ Özet ]
14) SADE J. Pathology and Pathogenesis of Serous Otitis Media. JAMA Otolaryngology?Head & Neck Surgery. 1966;84(3):297-305. [ Özet ]
15) Hinton AE, Buckley G. Parental smoking and middle ear effusions in children. J Laryngol Otol. 1988;102(11):992-996. [ Özet ]
16) Nakanishi N, Okamoto M, Nakamura K. Cigarette smoking and risk for hearing impairment: a longitudinal study in Japanese male office workers. J Occup Environ Med. 2000;42(11):1045-1049. [ Özet ]
17) Sharabi Y, Reshef-Haran I, Burstein M. Cigarette smoking and hearing loss: lessons from the young adult periodic examinations in Israel (YAPEIS) database. Isr Med Assoc J. 2002;4(12):1118-1120. [ Özet ]
18) Migirov L, Lipschitz N, Wolf M. Does smoking influence the surgical outcome of a myringoplasty? ORL J Otorhinolaryngol Relat Spec. 2013;75(4):207-210. [ Özet ]
19) Coelho DH, Peng A, Thompson M. Cartilage tympanoplasty in smokers. Ann Otol Rhinol Laryngol. 2012;121(10):657-663. [ Özet ]
20) Kim KH, Kabir E, Jahan SA. Waterpipe tobacco smoking and its human health impacts. J Hazard Mater. 2016;317:229-236. [ Özet ]
21) Shihadeh A, Schubert J, Klaiany J. Toxicant content, physical properties and biological activity of waterpipe tobacco smoke and its tobacco-free alternatives. Tob Control. 2015;24 Suppl 1:i22-i30. [ Özet ]




