EVALUATION OF CLINICAL AND MICROBIOLOGICAL RELATIONS OF POSTOPERATIVE THROAT FINDINGS IN PATIENTS UNDERWENT GENERAL ANESTHESIA
2Erciyes Universitesi Tıp Fakültesi, KBB Hastalıkları, Kayseri, Turkey
3Erciyes Universitesi Tıp Fakültesi, Tıbbi Mikrobiyoloji, Kayseri, Turkey
Summary
Objective: To evaluate clinical and microbiological relations of postoperative throat findings in patients underwent general anesthesia.Methods: Patients undergoing surgery apart from oropharyngeal, laryngotracheal or nasal regions were included in the study; those with chronic laryngopharyngitis, smokers, those with sore throat before surgery, those requiring multiple trial of intubation and those with delayed extubation after surgery were excluded. Age, gender, duration of intubated state, tube size and anesthetic agents used were recorded in all patients. In addition, endoscopic oropharyngeal and laryngeal examinations were performed on the before surgery and postoperative hour 24. symptoms of sore throat were questioned and pain scale was recorded on the hour 24 before surgery. Smear sample was obtained from nasopharynx wall before and after surgery. Samples were evaluated by Multiplex PCR assay which can detected 33 respiratory microorganisms. The relationship between microorganisms detected in preoperative and postoperative period, sore throat score and endoscopic examination findings were assessed and compared statistically.
Results: There were 40 patient who had inclusion criteria, aged between 18 - 65 years. There were abnormal examination findings in 55% and microorganism growth in 17.5% at postoperative period. No significant correlation was detected between abnormal postoperative examination findings and duration of intubated state while a significant correlation with postoperative sore throat score. No significant correlation was found between postoperative pain scoring and microorganism growth.
Conclusion: In this study, a relationship was found between postoperative throat findings and sore throat score but not in microbiological context.
Introduction
Today, many health issues have been addressed using surgical procedures; thus, general anesthesia with intubation might be required. The intubation, which is easy and uncomplicated procedure in most patients, may cause mild complications and, less frequently, severe complications.The complications due to intubation, including sore throat due to laryngeal and pharyngeal trauma, dryness, hoarseness and dysphagia, are commonly seen following surgical procedures performed under general anesthesia with intubation [1,2]. The incidence of postoperative sore throat (POST) has been reported as 30-70% in various studies [3,4]. Although POST is a minor complication, it results in patient dissatisfaction.
Although many studies have been conducted to evaluate etiology of postoperative throat complications, there is no study regarding likelihood of contamination and infection in the literature. In this study, it was aimed to evaluate symptoms and findings related to throat at postoperative period in clinical and microbiological manner.
Methods
The study was planned as a prospective study and approved by local ethical committee (Decision Number: 2017/307).
Patient selection
The study included 40 patients (aged 18-65 years) scheduled for surgery not involving oropharyngeal, laryngotracheal or nasal regions under general anesthesia via endotracheal route, who had normal preoperative pharynx and larynx examination and no history of chronic pharyngolaryngeal disorder, tonsillectomy, difficult intubation or were not candidate for difficult intubation. All patients gave written informed consent.
Preoperative period
In all patients, standard, endoscopy-assisted examination findings were recorded at ENT outpatient clinic on day before surgery. A swab sample was taken from pharyngeal wall in all patients before surgery and transferred to UTM 330C viral transport media (Copan Diagnostics, CA, USA). The samples were stored at -80 °C in microbiology laboratory.
Perioperative period
Following standard monitorization in operating room, anesthesia induction was achieved using 2 mg/kg propofol. The fentanyl was given at dose of 2 mcg/kg. Neuromuscular blockage was performed using rocuronium (0.6 mg/kg). All patients were intubated at first attempt by an experienced anesthesia team (at least 2 years). No additional procedure was undertaken for sterilization of laryngoscopes which were washed with soap and alcohol routinely before intervention. For intubation, a 7.5 non-spiral intubation tube was used in women whereas 8.0 non-spiral intubation tube in men. Endotracheal tube cuff pressure was set as 25-30 mmH2O. At time of extubation, appropriate airway device was inserted in all patients and a nelaton catheter was used to aspirate oronasal secretions.
Postoperative period
In all patients, endoscopic examination was repeated on the hour 24 after surgery and the findings were recorded. Again, a swab sample was taken from pharyngeal wall and transferred to same media. The samples were stored at -80 °C in microbiology laboratory.
Assessment
In all patients, age, gender, intubated time and surgical interventions performed were recorded. Sore throat score was rated using 4-points verbal rating scale within first 24 hours after surgery [5].
Sore throat scale was that, 0: No sore throat, 1: Mild sore throat (less than common cold), 2: Moderate sore throat (similar to common cold), 3: Severe sore throat (more than common cold).
Preoperative and postoperative endoscopy recordings of patients were assessed by an otolaryngologist blinded to timing of recordings.
In the samples obtained from pharyngeal wall and transferred to viral transport media, nucleic acid isolation was performed initially in order to detect nucleic acid originating from any infectious agent if present. Then, isolates obtained were amplified by Multiplex Polymerase Chain Reaction (PCR) Technique and visualized as graphics. In this stage, EZ1 virus min kit v2.0 (QUAGEN, Benelux, B.V., Netherlands) were used, which can detect 33 microorganisms (Table 1), and any of 33 microorganisms were displayed as a graphic, if present. The results were recorded as electronic media. Both samples obtained by 48-hours interval were assessed.
Table 1: Spectrum of microorganisms scanned by multiplex polymerase chain reaction test kit.
Statistical analysis
Data were analyzed using TURCOSA statistics software (Turcosa Ltd Co., www.turcosa.com.tr). The normal distribution was assessed using histogram, Q-Q plots and Shapiro-Wilk test. The variance homogeneity was assessed using Levene test. For inter-group comparisons, Mann Whitney U and Independent sample t tests were used in quantitative variables. One way analysis of variance and Kruskal Wallis test were used in comparisons including more than 2 groups. When p value was <0.05 it was considered as statistically significant.
Results
The study included 40 patients (aged 18-65 years, 15 men and 25 women) fulfilling inclusion criteria. Mean age was 47.05 years. No patient was excluded during follow-up.The patients had no otolaryngologic symptom and their physical examinations were normal at preoperative period. However, in preoperative samples analyzed using PCR technique, microorganism was isolated in 12 patients including rhinovirus in 2 patients, S. pneumonia in 3 patients, S. aureus in 2 patients, RSV A/B in one patient, coronavirus in 2 patients and H. influenza in 2 patients.
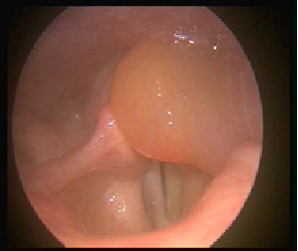
At postoperative period, all patients had postoperative sore throat at varying degrees (Table 2). Together with sore throat, there was dysphagia in 10 patients and dysphagia plus hoarseness in one patient. In postoperative examination, edema was detected at arytenoid in the patient with hoarseness (Picture 1a). (An informed consent form was gathered from the patient about publishing of his image).
 Büyütmek İçin Tıklayın |
Figure 1: Edematous mucosa of the left arytenoid |
 Büyütmek İçin Tıklayın |
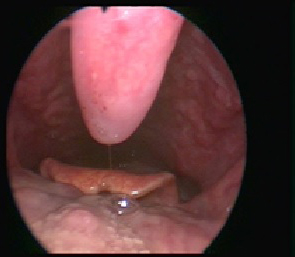
Figure 2: Erythema and thick mucus on the vocal cords |
 Büyütmek İçin Tıklayın |
Figure 3: Uvular erythema and edema. |
 Büyütmek İçin Tıklayın |
Figure 4: Erythema on the right anterior tonsillar plica. |
A significant correlation was detected between presence of abnormal examination finding and sore throat scoring on postoperative hour 24 (p<0.05; Table 2). When postoperative examination findings were assessed, there was uvular edema or erythema in 5 patients, oropharyngeal hyperemia and purulent discharge in 5 patients, glottic hyperemia in 10 patients, arytenoid edema in one patients and laryngeal mucus in one patients (Picture 1b, 1c and 1d). Intubation most commonly caused injury in glottic area.
In postoperative PCR analysis, rhinovirus was isolated in 2 patients whereas S. pneumonia in 2 patients, RSV A/B in one patient, coronavirus in one patient and adenovirus in one patient. Of 7 patients with positive postoperative sample, preoperative samples were negative in 2 patients where coronavirus and adenovirus isolated. In remaining 5 patients, same microorganisms were isolated in preoperative and postoperative samples. Moreover, no microorganism was detected in 7 of 12 patients with positive preoperative PCR analysis.
No significant correlation was observed between microorganism growth and sore throat scoring on postoperative hour 24 (p>0.05). Again, correlation was detected between presence of abnormal postoperative examination finding and microorganism growth (p>0.05) (Table 3).
A significant increase was detected in POST scores by prolonging intubated time (p<0.05). However, no significant correlation was detected between abnormal postoperative examination findings and intubated time (p<0.05). In addition, no significant correlation was found between microorganism growth and intubated time (p>0.05) (Table 4).
Discussion
In general anesthesia with endotracheal intubation, minor adverse events such as postoperative sore throat (POST) secondary to airway intervention and severe complications can be seen at airway at postoperative period [6,7]. Such complications often results from mucosal injury, inflammation, edema (laryngoscopy, aspiration, foreign body irritation (endotracheal tub, laryngeal mask, oral airway etc.) occurring secondary to airway intervention and its nature [3]. Local trauma causing aseptic inflammation of pharyngeal mucosa is implied as underlying mechanisms of POST [8]. Edema and congestion caused by inflammation contribute to formation and continuation of pain [9,10].In our study, various abnormal examination findings were observed in 7 patients with POST score of 3. A significant correlation was detected between POST score and abnormal examination finding.
When duration of anesthesia was assessed, Biro et al. found that mean duration of anesthesia was 180±88 min in patients with POST and 158±77 min in those without POST. Authors suggested that POST frequency was significantly increased by prolonging anesthesia time [11]. In our study, a significant correlation was observed between POST and intubated time in consistent with above-mentioned findings. The POST scores were significantly increased by increasing intubated time.
In some studies, it has been proposed that cuff pressure of intubation tube should be maintained at 25-40 cmH2O. It was reported that pathological changes such as ischemia, ulceration, perforation, granulation tissue or stenosis could develop at high pressures and that POST frequency is increased [12,13]. In a study using intubation tube of 6 or 7 mm in women, Jaensson et al. reported that smaller tube use decreased POST symptoms [14]. In our study, 7.5 mm intubation tube was used in women whereas 8.0 mm intubation tube in men and cuff pressure was maintained at 25-30 cmH2O in all patients; thus, these were not used as a variable for POST.
Kloub et al. evaluated how experience of anesthesiologist and repeated intubation attempts affect POST [15]. Authors found that both factors had no association with POST but they found that prolonged duration of intubation and nasogastric catheter use were associated with increased POST. In addition, use of pharyngeal heat probe was also found to be associated with POST [16]. Although experience of anesthesiologist or ETE intervention has not been linked to POST, all patients were intubated by an anesthesia team with minimum 2 years of experience in our study. Only patients intubated at first attempt were included to the study given that repeated attempts may cause airway trauma.
Although there are many studies evaluating etiology of postoperative complications at throat, there is no study on likelihood of contamination and infection in the literature. In our study, it was aimed to investigate whether postoperative complications at throat are due to infection caused by contamination and to evaluate causality by microbiological test and examination data.
In operating room, the patients are exposed to several interventions involving devices and tools that may contact with their intact skin, mucosa or sterile tissues. Inadequate disinfection or sterilization of equipment can cause cross-contamination.
In a study assessing level of knowledge about infection control measures among anesthesiologists in two academic hospitals in Egypt (2018), it was found that there was an inadequacy regarding sterilization. In the study, gram negative bacilli, gram positive bacilli and gram positive cocci growth was detected in 68.2% of samples obtained from ready-to-use laryngoscopes in operating rooms and intensive care units [16]. In 2007, effects of classical endotracheal intubation on contamination were investigated in a Chinese study. Ninety patents were randomly assigned into 2 groups and intubation was performed using classical protection-free endotracheal tubes while using endotracheal tubes with sterile, transparent cover. It was observed that the difference in bacterial counts obtained before intubation and extubation was lower in the group intubated using endotracheal tube with sterile cover. It was predicted that endotracheal bacterial contamination could be reduced by sterile endotracheal intubation [17].
In our study, microorganism growth was observed in the samples from 5 of 25 patients with POST score of 2 or 3. In addition, microorganism growth was detected in the samples from 5 of 22 patients with abnormal postoperative examination finding. Postoperative examination was normal in 2 patients with microorganism growth. Of 40 patients included, several microorganisms including rhinovirus, S. pneumonia, RSV A/B, coronavirus and H. influenza were detected in the preoperative samples obtained from 12 patients. Higher proportion of viruses suggest that PCR can detect microorganisms even they are present in the patient flora or inactive.
In postoperative period, rhinovirus, S. pneumonia, RSV A/B, coronavirus and adenovirus growth were detected in 7 patients. Of these, preoperative samples were negative in 2 patients with coronavirus and adenovirus growth. In remaining 5 patients, same microorganisms were isolated in preoperative and postoperative samples. Detection of novel pathogens in 2 patients at postoperative period can be considered as significant regarding contamination. It is likely that respiratory pathogens detected in 12 patients at preoperative period turned to negative in patients at postoperative as a result of effects of antibiotics given at preoperative period.
In 2 of 7 patients with negative growth at postoperative period, detection of viral pathogens in preoperative PCR analysis was attributed to contamination during sampling. However, given that PCR can detect DNA residues from living or death pathogens, DNA residues detected in the patient may be due to recent viral infection before surgery.
This is the first study investigating sore throat and contamination risk using PCR analysis.
Conclusion
In our study, it was seen that POST score was associated to intubated time and presence of abnormal postoperative examination finding. No significant association was detected between pain score and postoperative microorganism detection. Again, no significant relationship was found abnormal postoperative findings and intubated time or postoperative microorganism growth. Changing of microbiological pattern in throat could related to contamination. It was not significant clinically. Equipments such as laryngoscope, aspiration catheter or oropharyngeal airway used in intubation and extubation are potential sources for direct and cross-contamination if optimal sterilization standards are failed. It can be suggested that postoperative sore throat is associated to intubated time rather than microogranism.
Conflict of interest
Authors declare no commercial or conflict of interest.
Main Points
- Postoperative sore throat is associated with operation time.
- Postoperative sore throat is not related to microorganisms.
- There are pathological endoscopic findings in patients with postoperative sore throat.
Reference
1) Zuccherelli L. Postoperative upper airway problems. Southern Afr J Anaesth Analg. 2003 ;9:12-6.
2) Edomwonyi NP, Eluwa B, Osaigbovo EP, Omo NE, Rupasinghe A. Intraoperative and recovery room outcome. East Afr Med J. 2005 ;82:66-72 [ Özet ]
3) Tanaka Y, Nakayama T, Nishimori M, Tsujimura Y, Kawaguchi M, Sato Y. Lidocaine for preventing postoperative sore throat. Cochrane Datebase Syst Rev. 2015 ;14:CD004081 [ Özet ]
4) El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a Systematic review. Anaesthesia. 2016 ;71:706-17 [ Özet ]
5) Tazeh-Kand NF, Eslami B, Mohammadian K. Inhaled fluticasone propionate reduces postoperative sore throat, cough, and hoarseness. Anesth Analg. 2010 ;111:895-8 [ Özet ]
6) Mehta S, Mickiewicz M. Pressure in large volume, low pressure cuffs: its significance, measurement and regulation. Intensive Care Med. 1985 ;11:267-72 [ Özet ]
7) Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G ,et al. Intracuff pressure and tracheal morbidity: influence offilling with saline during nitrous oxide anesthesia. Anesthesiology. 2001 ;95:1120-4 [ Özet ]
8) Canbay O, Celebi N, Sahin A, Celiker V, Ozgen S, Aypar u. Ketamine gargle for attenuating postoperative sore throat. Br J Anaesth. 2008 ;100:490-3 [ Özet ]
9) Hung NK, Wu CT, Chan SM, Lu CH, Huang YS, Yeh CC ,et al. Effect on postoperative sore throat of spraying the endotracheal tube cuff with benzydamine hydrochloride, 10% lidocaine, and 2% lidocaine. Anesth Analg. 2010 ;111:882-6 [ Özet ]
10) Agarwal A, Nath SS, Goswami D, Gupta D, Dhiraaj S, Singh P. An evaluation of the efficacy of aspirin and benzydamine hydrochloride gargle for attenuating postoperative sore throat: a prospective, randomized, single-blind study. Anesth Analg. 2006 ;103:1001-3 [ Özet ]
11) Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur J Anaesthesiol. 2005 ;22:307-11 [ Özet ]
12) Stewart SL, Secrest JA, Norwood BR, Zachary R. A comparison of endotracheal tube cuff pressures using estimation techniques and direct intracuff measurement. AANA J. 2003 ;7:443-7 [ Özet ]
13) Mandoe H, Nikolajsen L, Lintrup U, Jepsen D, Molgaard J. Sore throat after endotracheal intubation. Anesth Analg. 1992 ;74:897-900 [ Özet ]
14) Jaensson M, Olowsson LL, Nilsson U. Endotracheal tube size and sore throat following surgery: a randomized-controlled study. Acta Anesthesiol Scand. 2010 ;54:147-53 [ Özet ]
15) Kloub R. Sore throat following tracheal intubation. Middle East J Anaesthesiol. 2001 ;16:29-40 [ Özet ]
16) Tash RME, Wegdan AA, Amer FA, Bassyouni RHA, Botros JM. Pattern of anaesthetic equipment contamination and infection prevention in anaesthesia practice at university hospitals. Indian J Anaesth. 2018 ;62:786-92 [ Özet ]
17) Xu JQ, Zhu B, Ye TH, Ren HZ. Protective endotracheal intubation to reduce endotracheal bacterial contamination. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2007 ;29:510-3 [ Özet ]




