ARE THE NEUTROPHIL/LYMPHOCYTE RATIO (NLR) AND PLATELET/LYMPHOCYTE RATIO (PLR) VALUES USEFUL TO DETERMINE THE PROGNOSIS OF IDIOPATHIC SUDDEN SENSORINEURAL HEARING LOSS?
Summary
Introduction: The aim of the present study was to investigate the usefulness of the neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR) as predictive markers for idiopathic sudden sensorineural hearing loss (ISSHNL).Methods: In this retrospective, case-controlled, clinical study, 48 patients who were diagnosed with and treated for the idiopathic sudden sensorineural hearing loss were compared to 40 healthy individuals who applied to hospital for routine health checks. In addition, the patients with ISSNHL who responded to the treatment and those who did not were compared and evaluated using statistical methods. The laboratory analyses on blood samples from the patients taken before the treatment and from healthy individuals were used. NLR, PLR, White blood cell count (WBC) and its subgroups were calculated separately for the patient and control groups.
Findings: NLR and PLR were significantly higher in the ISSNHL group than in the control group (p<0.0001 and p<0.01, respectively). On the other hand, the NLR values of groups responding and non-responding to treatment were not statistically different (p>0.05). Likewise, PLR values were not statistically different between responding and non-responding groups (p> 0.05)
Conclusion: While the NLR and PLR increases in ISSNHL support the inflammatory theory in ISSNHL, NLR is not an effective marker for prognosis. However, PLR can be used as a marker, albeit a weak one, to determine prognosis.
Introduction
Idiopathic sudden sensorineural hearing loss (ISSNHL) is a sensorineural hearing loss that develops suddenly within three days and occurs in three consecutive frequencies in the audiogram. The annual incidence rate is 5-20/100,000. It is more common after 40 years of age [1]. In terms of etiology, retrocochlear pathologies are responsible in approximately 1% of the cases, while 15% are caused by Meniere's syndrome and autoimmune diseases. The etiology is unknown in 85% of the cases. The cases with unknown etiology are defined as idiopathic sudden sensorineural hearing loss. It is believed that this condition could be caused by the inflammatory process or vascular occlusion at the vascular level in cochlea [2]. The vascular feeding of the cochlea is provided by the labyrinthine artery. Higher incidence of the sudden hearing loss in patients with conditions such as hypertension and diabetes mellitus are associated with events such as vasospasm, thrombosis and hemorrhage at microvascular level, and this supports the vascular theory in sudden hearing loss. The role of viral agents in ISSNHL has also been discussed. Especially mumps virus, varicella zoster, Epstein Barr virus and cytomegalovirus are responsible for etiology [3,4]. However, studies show that sudden sensorineural hearing loss could also be linked with chronic inflammatory condition, one of the most important causes of microvascular ischemia [5,6].White blood cells (WBC) and its subtypes have been described as markers of inflammatory events, especially in cardiovascular diseases and cerebrovascular events [7,8]. In recent years, the neutrophil/lymphocyte ratio (NLR) and platelet/lymphocyte ratio (PLR) have been used as predictors of many diseases as easy and cheap inflammatory response parameters [9]. NLR has been investigated as a marker for systemic inflammatory response, especially in cardiovascular diseases, atherosclerosis and cerebrovascular events [7,8]. It was found that PLR increase was only a poor marker in diseases such as atherosclerosis [10].
The aim of the present study was to investigate the usefulness of the NLR and PLR as predictive markers for sudden sensorineural hearing loss.
Methods
The study was approved by the local ethics committee and conducted in accordance with the ethical principles described by the Declaration of Helsinki.This retrospective case-control study included patients who were treated for sudden sensorineural hearing loss in the period between April 2010 and April 2017 in Tokat State Hospital and healthy individuals who applied to our hospital for routine health checks (Control group). For the definition of sudden sensorineural hearing loss, the hearing loss which occurred in the last three days and hearing loss more than 30 dB in three consecutive frequencies in the audiogram were taken as criteria. Routine otologic examinations and hematological analyzes were performed during the patient admissions. In addition, the retrocochlear pathologies were evaluated with MRI.
Patients who were diagnosed with systemic diseases such as diabetes mellitus, hypertension, chronic kidney and liver disease, patients with arteriovenous thrombosis and patients younger than 18 years were excluded from the study. In addition, patients who had otosclerosis, Meniere's disease, retrocochlear pathology, active or chronic middle ear disease and internal or middle ear anomalies were excluded from the study. The control group consisted of healthy individuals who applied to the hospital for routine health checks, had no active or chronic disease, had no active or chronic internal or middle ear disease, and had normal hearing levels in pure tone audiometry (air-conduction hearing threshold 0-20 dB). Forty-eight patients and 40 healthy individuals who met the criteria were included in the study. Before treatment, the consent forms were taken from all patients. Blood samples were taken from all patients before the treatment. NLR was calculated by dividing the amount of neutrophils by the amount of lymphocytes, and PLR was calculated by dividing the amount of platelet by the amount of lymphocytes. The complete blood count was determined by a fully automatic blood cell counter (BC-6800, Mindray, Guangdong, China).
Before the treatment, pure tone audiometry test was performed on patients during their admission. The air and bone conduction levels in both ears were evaluated at 250 Hz, 500 Hz, 1 kHz, 2 kHz, 4 kHz and 8 kHz frequencies. After medical treatment, control audiometry was performed at the first month of admission. Siegel's criteria were used to evaluate the hearing levels of patients before and after the treatment (Table 1) [11]. According to this criteria, the patient group was divided into two subgroups as treatment responder (complete + partial + slight) and non-responder (no improvement). Based on the Siegel's criteria, 25 patients were concluded to be in the treatment responder group and 23 patients allocated to the treatment non-responder group.
All patients were treated with oral methylprednisolone at a dose of 1 mg/kg (Prednol L 16 mg tb® and 4 mg tb®, Mustafa Nevzat, Istanbul, Turkey). Steroid therapy was terminated in two weeks with gradual dose reduction.
Statistical Analyses
Mean, standard deviation, median, minimum and maximum values were given for the statistical definition of the groups. The Kolmogorov-Smirnov test was used to determine whether the groups had normal distribution. For comparison of the groups, independent t-test, which is a parametric test, was used for the variables with normal distribution. Mann-Whitney U test, which is a non-parametric counterpart of independent t-test, was used for variables with non-normal distribution. Significance of the difference between the groups was evaluated at p<0.05 level. All statistical analyses were performed using Medcalc software v.16.4.3 (Ostend, Belgium).
Results
The mean age of the patient and control groups were 49.7±14.4 and 47.8±12.5, respectively. Twenty-eight of the patients in the patient group were female and 20 were male. Twenty-three of the individuals in the control group were female while 17 were male. There was no significant difference between the two groups in terms of age and gender (Table 2).Table 2: The Demographic and Clinical Characteristics of the Patients and Controls
The laboratory results of the patient and control groups were shown in Table 2. The mean NLR value was 4.22±2.52 in ISSNHL patients and 1.86±0.69 in control group. It was found that two groups were not significantly different for NLR (p< 0.0001) (Figure 1, Table-2). Neutrophil values were 6.88±2.68 in the patient group and 4.59±1.64 in the control group. A significant difference was found between the two groups for neutrophil values (p< 0.0001) (Table 2). Lymphocyte levels were significantly higher in control group (p< 0.0001) (Table 2). The mean PLR value was 151±87.2 in patient group and 106±41.0 in control group. PLR was significantly higher in patient group (p< 0.05) (Figure 2).
 Büyütmek İçin Tıklayın |
Fig 1: Mean NLR values of the patient and control groups. |
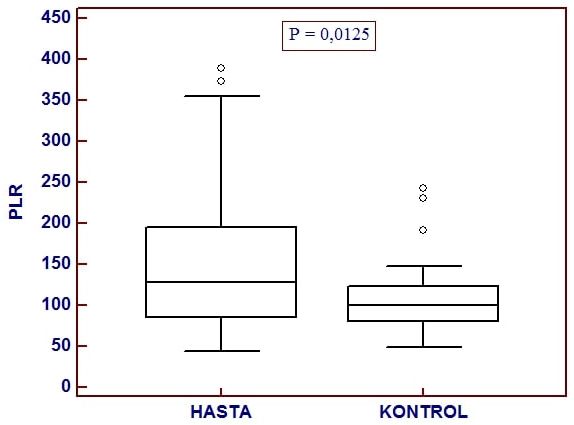 Büyütmek İçin Tıklayın |
Fig 2: Mean PLR values of the patient and control groups. |
Mean NLR level was 3.76±2 in the treatment responder group and 4.74±2.98 in the treatment non-responder group (p> 0.05) (Table 3). Mean PLR level was 134±77 in treatment responder group and 171±94 in treatment non-responder group. Mean PLR was not different between treatment non-responder and treatment responder groups (p> 0.05) (Table 3). Although the neutrophil and platelet values were higher in treatment non-responder group compared to treatment responder group, difference was not significant (p> 0.05 and p> 0.05, respectively) (Table 3).
Table 3: Statistical data between the recovered and unrecovered groups.
Discussion
The present study aimed to investigate a possible role of inflammation in ISSNHL using inflammation markers such as NLR and PLR and to determine the usefulness of NLR and PLT as markers to evaluate the prognosis of ISSNHL. Forty eight patients with unilateral ISSNHL treated with standard treatment modalities were evaluated. NLR was significantly higher in ISSNHL groups compared to healthy control. On the other hand, the group of patients who responded to the treatment was not significantly different from the group of patients who did not for inflammation markers such as NLR and PLR.Although the acute or chronic inflammation, viral infections and vascular events are considered in the etiology of sudden sensorineural hearing loss, the precise causes have not been fully identified yet. Atherosclerotic microvascular circulatory disorders, inflammatory and infectious causes are the most frequently blamed factors for ISSNHL [12]. There is also viral theory about the possible causes of ISSNHL. According to this theory, the herpes simplex virus is involved in the etiology of ISSNHL. However, the inability to obtain adequate responses to antiviral treatment weakens this theory [13]. Because of the higher incidence of ISSNHL in diseases with impaired microcirculation such as hypertension and diabetes, the microvascular dysfunction has been brought to the foreground in the etiology [14]. Ciccone et al. found that the ISSNHL was more common in patients with increased carotid intima-media thickness [15]. However, in some other studies new markers linking chronic inflammation with cochlear injury were investigated [16]. The increased amount of neutrophils increases the production of cytokines such as IL-6, IL-8, and tumor necrosis factor-?, thereby playing a role in inflammation. Increased platelet numbers were also found to be associated with microvascular occlusion and perfusion defects [17,18]. In recent years, PLR and NLR have been used as a new thrombo-inflammatory markers in the evaluation of the prognosis and mortality of different cerebrovascular and cardiovascular diseases [19,20]. In some studies, use of NLR and PLR increases as markers for systemic inflammatory response in autoimmune diseases, acute pancreatitis and malignancies has been investigated [21-23].
Platelets are an important factor in the provision of thrombosis, coagulation, development and progression of atherosclerosis. Elevated PLR values accompanied with higher platelet count are thought to be secondary to vascular ischemia. Increased PLR values in extremity ischemia support this hypothesis [24]. A number of prognostic indicators have been investigated for ISSNHL for a long time. These include tinnitus, vertigo, grade of hearing loss, presence of diabetes and audiogram shape [25,26]. Recently, some studies have proposed certain blood test parameters of complete blood count test (CBC) such as NLR and PLR as markers for the prognosis of ISSNHL. These studies reported that low levels of NLR and PLR were associated with good prognosis of ISSNHL [16,17,27]. In line with the previous studies, NLR and PLR in ISSNHL group were higher compared to healthy control group in the present study. Interestingly, although NLR was higher in treatment non-responder group compared to the treatment responder group, the difference was not significant. Likewise, PLR values in the treatment responder and non-responder groups were not significantly different.
Recently, ISSNHL has been reported to be associated with chronic inflammation [28]. In a study conducted by Masuda et al., associations were reported between prognosis in the ISSNHL patients and high-sensitivity C-reactive protein (hsCRP) and tumor necrosis factor (TNF) [29]. Neutrophil and lymphocyte counts, NLR and PLR are parameters related to inflammation [30]. Seo et al. [17] suggested that ISSNHL induces systemic stress and that the resulting endothelial damage and inflammation increase NLR and PLR. Elevated NLR and PLR values of ISSNHL patients in the present study support a possible association between SSNHL and inflammation. On the other hand, although NLR value of the ISSNHL patient group who did not respond to the treatment was higher than that of ISSNHL patient group who responded to treatment, the difference was not significant. This finding shows that NLR is not an effective marker for determining the prognosis of ISSNHL.
Oral methylprednisolone was administered for the treatment of all patients. On the other hand, only systemic steroid was used in some studies dealing with the use of NLR and PLR to evaluate the prognosis of ISSNHL [16,31]. Some other studies used intratympanic dexamethasone in addition to systemic steroid for the treatment of patients with SSNHL [17,32]. Twenty-five of the 48 patients (52%) with SSNHL in the present study responded to treatment. In their study about the prognostic value of NLR and PLR in patients with SSNHL, Ulu et al. [16] found that 21 of the 47 patients (44.6%) had response to treatment. On the other hand, Seo et al. [17] used intratympanic dexamethasone in addition to systemic steroid for the treatment of 348 patients with SSNHL and achieved response in 78.6% of the patients. In another study, pentoxifylline and oral vitamin B1 (250 mg thiamine hydrochloride) and B6 (250 mg pyridoxine hydrochloride) were used along with systemic steroid for the treatment of patients with SSNHL, and a response rate of 59.2% was observed [33]. These findings showed that different treatment modalities could affect the success rates in recovery of patients with SSNHL.
Main limitations of the present study were its retrospective nature and relatively limited number of patients included. There were only 48 patients meeting the study criteria in the eight-year period covered by the study based on medical records. Prospective studies with larger cohorts could be more useful for evaluating the prognostic value of NLR and PLR in SSNHL.
Conclusion
While the NLR and PLR increases in ISSNHL support the inflammatory theory in ISSNHL, NLR is not an effective marker for prognosis. However, PLR can be used as a marker, albeit a weak one, to determine prognosis.Financial Disclosure: The authors declare that the present study received no financial support. Conflict of Interest: The authors have no conflicts of interest to declare.
Reference
1) Rauch SD. Idiopathic sudden sensoneurinal hearing loss. N Eng J Med 2008; 359:833-40. [ Özet ]
2) Mom T, Gilain L, Avane P. Cochlear ischemia: from fundamental data to clinical hope. Ann Otolaryngol Chir Cervicofac 2008;125:301-8. [ Özet ]
3) Wackym PA. Molecular temporal bone pathology: II. Ramsay Hunt syndrome (herpes zoster oticus). Laryngoscope 1997;107:1165-75. [ Özet ]
4) Wilson WR, Veltri RW, Laird N, Sprinkle PM. Viral and epidemiologic studies of idiopathic sudden hearing loss. Otolaryngol Head Neck Surg. 1983;91:653-8 [ Özet ]
5) Ryan AF, Harris JP, Keithley EM. Immune-mediated hearing loss: basic mechanisms and options for therapy. Acta Otolaryngol 2012;122:38-43. [ Özet ]
6) Hiramatsu M, Teranishi M, Uchida Y, Nishio N, Suzuki H, Kato K, et al. Polymorphisms in genes involved in inflammatory pathways in patients with sudden sensorineural hearing loss. J Neurogenet 2012;33:387-96. [ Özet ]
7) Tamhane UU, Aneja S, Montgomery D, Rogers EK, Eagle KA, Gurm HS. Association between admission neutrophil to lymphocyte ratio and outcomes in patients with acute coronary syndrome. Am J Cardiol. 2008;102:653-7 [ Özet ]
8) Balta S, Ozturk C. The platelet-lymphocyte ratio: a simple, inexpensive and rapid prognostic marker for cardiovascular events. Platelets. 2015;26:680-681. [ Özet ]
9) Huang W, Huang J, Liu Q, Lin, F., He, Z., Zeng, Z, et al. Neutrophil-lymphocyte ratio is a reliable predictive marker for early-stage diabetic nephropathy. Clinical Endocrinology.2015; 82: 229-33. [ Özet ]
10) Kwon H, Kim SH, Oh SY, Lee S, Lee JH, Choi HJ, et al. Clinical significance of preoperative neutrophillymphocyte versus platelet-lympohocyte ratio in patient with operable colorectal cancer. Biomarkers 2012;17:216-22. [ Özet ]
11) Siegel LG. The treatment of idiopathic sudden sensorineural hearing loss. Otolaryngol. Clin N. Am. 1975; 8: 467-73. [ Özet ]
12) Ryan AF, Harris JP, Keithley EM. Immune-mediated hearing loss: basic mechanisms and options for therapy. Acta Oto-Laryngologica. 2002;548:38-43. [ Özet ]
13) Merchant SN, Durand ML, Adams JC. Sudden deafness: is it viral? Journal of Oto-Rhino-Laryngology. 2008; 70: 52-62. [ Özet ]
14) Rudack C, Langer C, Stoll W, Rust S, Walter M. Vascular risk factors in sudden hearing loss. Thrombosis and Haemostasis. 2006;95:454-61. [ Özet ]
15) Ciccone MM, Cortese F, Pinto M, Di Teo C, Fornarelli F, Gesualdo M, et al. Endothelial function and cardiovascular risk in patients with idiopathic sudden sensorineural hearing loss. Atherosclerosis. 2012;225: 511-16. [ Özet ]
16) Ulu S, Ulu MS, Bucak A, Ahsen A, Yucedag F, Aycicek A. Neutrophil-to-lymphocyte ratio as a new, quick, and reliable indicator for predicting diagnosis and prognosis of idiopathic sudden sensorineural hearing loss. Otol Neurotol 2013; 34: 1400-4 [ Özet ]
17) Seo YJ, Jeong JH, Choi JY, Moon IS. Neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio: novel markers for diagnosis and prognosis in patients with idiopathic sudden sensorineural hearing loss. Dis Markers. 2014;2014:702807 [ Özet ]
18) Moodley D, Mody GM, Chuturgoon AA. Initiation but no execution modulation of peripheral blood lymphocyte apoptosis in rheumatoid arthritis - a potential role for heat shock protein 70. J Inflamm 2011; 8: 30. [ Özet ]
19) Lee JH, Kwon KY, Yoon SY, Kim HS, Lim CS. Characteristics of platelet indices, neutrophil-to-lymphocyte ratio and erythrocyte sedimentation rate compared with C reactive protein in patients with cerebral infarction: a retrospective analysis of comparing haematological parameters and C reactive protein. BMJ Open 2014; 4: e006275 [ Özet ]
20) Azab B, Shah N, Akerman M, McGinn JT Jr. Value of platelet/lymphocyte ratio as a predictor of all-cause mortality after non-ST-elevation myocardial infarction. J Thromb Thrombolysis 2012;34:326-34. [ Özet ]
21) Chandrashekara S, Mukhtar Ahmad M, Renuka P, Anupama KR, Renuka K. Characterization of neutrophil-to-lymphocyte ratio as a measure of inflammation in rheumatoid arthritis. Int. J. Rheum. Dis. 2017; 20: 1457-67. [ Özet ]
22) Wang Y, Fuentes HE, Attar BM, Jaiswal P, Demetria M. Evaluation of the prognostic value of neutrophil to lymphocyte ratio in patients with hypertriglyceridemiainduced acute pancreatitis. Pancreatology .2017;17;893-97. [ Özet ]
23) Zheng J, Cai J, Li H, Zeng K, He L, Fu H, et al. Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio as Prognostic Predictors for Hepatocellular Carcinoma Patients with Various Treatments: a Meta-Analysis and Systematic Review. Cell Physiol Biochem. 2017;44:967-81. [ Özet ]
24) Gray T, Pichler M, Belaj K, Hafner F, Gerger A, Froehlich H, et al. Platelet to lymphocyte ratio: a novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. PLoS ONE 2013;8:7-12. [ Özet ]
25) Schreiber BE, Agrup C, Haskard DO, Luxon LM. Sudden sensorineural hearing loss. Lancet 375 (9721), 1203-1211. [ Özet ]
26) Michel O. The revised version of the german guidelines "sudden idiopathic sensorineural hearing loss". Laryngorhinootologie 2011;90:290-3. [ Özet ]
27) Bulğurcu S, Dikilitaş B, Arslan İB, Çukurova İ. Neutrophil-to-lymphocyte and platelet to-lymphocyte ratios in pediatric patients with idiopathic sudden hearing loss. J. Int. Adv. Otol. 2017;13: 217-220. [ Özet ]
28) Svrakic M, Pathak S, Goldofsky E, Hoffman R, Chandrasekhar SS, Sperling N, et al. Diagnostic and prognostic utility of measuring tumor necrosis factor in the peripheral circulation of patients with immune-mediated sensorineural hearing loss, Arch. Otolaryngol. Head Neck Surg. 2012;138:1052-58. [ Özet ]
29) Masuda M, Kanzaki S, Minami S, Kikuchi J, Kanzaki J, Sato H, et al. Correlations of inflammatory biomarkers with the onset and prognosis of idiopathic sudden sensorineural hearing loss. Otol. Neurotol. 2012;33:1142-50. [ Özet ]
30) Hao X, Li D, Wu D, Zhang N. The relationship between Haematological indices and autoimmune rheumatic diseases (ARDs), a meta-analysis. Sci. Rep. 2017;7:10833.
31) Özler GS. Increased Neutrophil-Lymphocyte Ratio in Patients With Idiopathic Sudden Sensorineural Hearing Loss. Journal of Craniofac. Surg. 2014;25:260-3. [ Özet ]
32) Kocak HE, Elbistanli MS, Acipayam H, Alakras WME, Kiral MN, Kayhan FT. Are neutrophil/lymphocyte and platelet/lymphocyte ratios related with formation of sudden hearing loss and its prognosis? Eur Ann Otorhinolaryngol Head Neck Dis 2017; 134: 383-6. [ Özet ]
33) Durmuş K, Terzi H, Karataş TD, Doğan M, Uysal IÖ, Şencan M, et al. Assessment of hematologicalfactors involved in development and prognosis of idiopathic sudden sensorineural hearing loss. J Craniofac Surg 2016: 1: 85-91. [ Özet ]




