COMPARISON OF NEEDLE-TIP MONOPOLAR AND COLD-KNIFE DISSECTION FOLLOWED BY BIPOLAR HEMOSTASIS TONSILLECTOMY: SIDE-BY-SIDE COMPARISON OF TECHNIQUES WITH RANDOMIZED, SINGLE-BLINDED AND PROSPECTIVE STUDY DESIGN
2Sağlık Bilimleri Üniversitesi, Okmeydanı Eğitim ve Araştırma Hastanesi, KBB Bölümü, İstanbul, Turkey
Summary
Aim and Study Design: Comparison of different tonsillectomy interventions in terms of operation duration, postoperative pain, tonsillar fossa healing and postoperative hemorrhage rate. Study was randomised, prospective, single-blinded and controlled with side-by-side design. One side was operated with monopolar needle-tip electrocautery (MNE) and the other side was operated with cold-knife dissection followed by bipolar hemostasis (CKB).Methodology: Patients with tonsiller hypertrophy and obstructive symptoms were enrolled in the study. Inclusion criteria consisted of patients aged 13-or-above who had tonsillar hypertrophy and obstructive symptoms that indicated tonsillectomy. Duration of dissection and duration of hemostasis was recorded; these two values were added to calculate the total operative duration for each side. Postoperative pain was evaluated with patient reported pain visual analogue scale (VAS) scores. Tonsillar fossa healing was evaluated single-blindedly.
Results: Total of forty-four tonsils were removed from twenty-two patients with a mean age of 26.5±11.6. Total time for removal of tonsil was shorter for CKB side, but hemostasis was shorter in MNE side. Total overall operative time required for surgery was significantly lower for MNE-operated side. Postoperative pain VAS scores on the MNE side was always lower compared to CKB side. Fossa healing scores were better on postoperative day #1 and #5 in MNE side compared to CKB side, but were similar on postoperative day #10. Postoperative hemorrhage rate was the same (4.5%, 1/22) for both interventions.
Conclusion: MNE is an affordable and cost-effective alternative. Utilization of MNE does not prolong surgical time. Postoperative pain is considerably lower compared to the latter technique. Therefore MNE can be a viable option for surgeons looking for affordable solutions to monopolar electrocautery.
Introduction
Tonsillectomy techniques are mainly divided into cold steel knife dissection and hot techniques that utilize electrocautery and other contemporary technological devices. Advantages and disadvantages of hot and cold techniques have been long-debated [1,2]; main parameters are: cost, surgical time, postoperative bleeding rate and posteropative pain [3-5]. Among all other techniques, monopolar electrocautery is ideal in terms of cost effectiveness and postoperative bleeding rate[6]; trade-off with electrosurgery is the variable amount of tissue necrosis due to thermal injury which consequently results with increased postoperative pain [7]. Reports of reduced thermal injury, hence, lower postoperative pain have been published with utilization of finer/thinner electrocautery tips [8]. Utilization of Colorado needle with superior results have been reported [9,10], monopolar needle-tip electocautery (MNE) tips are also considerably thinner cost-effective alternatives to bovie tips (Figure 1).
 Büyütmek İçin Tıklayın |
Figure 1: Standard (Bovie) versus needle-tip monopolar electracautery Close- up photograph comparing the standard-size (Bovie) needle electrocautery and the needle-tip electrocautery. |
Our aim in this study is to evaluate the effectiveness of MNE in comparison to cold-knife dissection and bipolar diathermy hemostasis tonsillectomy. This comparison was based on following parameters: surgical time, postoperative tonsillar fossa healing score and postoperative patient reported pain.
METHODOLOGY
Twenty-two (n=22) patients aged 13-or-above who referred to our clinic with tonsiller hypertrophy and obstructive symptoms from February 1, 2017, to July 31, 2017, were enrolled in the study. Data were collected from February 1, 2017, to August 15, 2017, and follow-up was completed on June 31, 2017. Inclusion criteria consisted of patients aged 13-or-above[5] who had tonsillar hypertrophy and obstructive symptoms that indicated bilateral tonsillectomy. Suspection of malignancy, bleeding diathesis, history of fibromyalgia or pain-related disorders and other comorbidities constituted exclusion criteria. The ethics committee of Bakirkoy Research and Education Hospital (Bakırköy, Istanbul, Turkey) approved the study, which conformed to the Declaration of Helsinki. All patients individually provided written informed consent prior to study.
1. Study design: Study design was prospective, randomised, single-blinded and control was established with side-by-side comparison. Either right tonsil was operated with MNE, contralateral side was operated with cold-technique; or vice-versa, which side received which treatment was randomly assigned as previously described in the literature [3].
2. Surgical Technique: Both tonsils were injected with local anesthetic infiltration to anterior tonsillar plica before the operation. All surgeries were performed by the primary author (BO) under x2.5 loupes. Force 2 Electrosurgical Generator (The Valley Lab, Boulder,CO) was used to power both the monopolar and bipolar electrocautery. Bipolar cautery settings were used (25 Watts) in accordance with the literature. Monopolar electrocautery settings were adjusted to Blend 1' which is a summation of the coagluation and cutting waveforms (75% cutting, 25% coagulation). Cut power was adjusted to 10W, whereas coagulation power was set to 12 Watts.
2.1. Cold-knife dissection and bipolar group (Group CKB): Incision was made to anterior tonsillar plica and subcapsular dissection was carried out. The inferior pole of the tonsil was bipolarized. The tonsil bed was abundantly irrigated with saline. Bleeding points were cauterized with bipolar electrocautery for hemostasis. Tonsil bed was abundantly irrigated numerous times to see any sign of bleeding.
2.2. Monopolar Needle-tip Electrocautery group (Group MNE): Incision was made to anterior tonsillar plica. The mucosal covering was retracted with assistance and all micro-vessels between the capsule and tonsil was cauterized under direct vision (with loupes). The inferior pole of the tonsil was also cauterized by the MNE. Following abundant irrigation, the hemostasis was ensured.
3. Assessment of Outcomes: Four parameters were evaluated:
3.1. Surgical time was measured intraoperatively in minutes. The stopwatch of the operating room was utilized for measurement of each side seperately as follows: dissection/resection time (a) was noted as the time period between first plica incision to the time tonsil was given to the surgical nurse as pathology. Haemostasis duration was calculated seperately (b) and total surgical time was (a+b) the time between first incision until complete haemostasis of the side being operated.
3.2 Postoperative pain: Postoperative patient reported pain was evaluated with Visual Analogue Scale (VAS) as previously described in the literature [11]. All patients were given a follow-up form for evaluation of their postoperative pain. They were asked to assess their pain on either side (right and left) seperately and note on the follow-up form. Patients were asked to rate their pain 0 (no pain) and 10 (maximum pain). This evaluation was carried out for the first ten postoperative days (POD), twice daily, by the patient.
3.3 Assessment of tonsillar fossa healing was performed by the secondary author (MED) on postoperative day (POD) #1,5 and 10 according to previously described > methodology by Magdy et al. [12](Table 1). Evaluator (MED) was blind to the procedure carried out on either side.
Table 1: Scoring system introduced by Magdy EA for evaluating tonsillar fossa wound healing12
3.4. Prevelance of post-operative hemorrhage: any occurrence of postoperative bleeding was noted : postoperative day/hour and which side was bleeding. Oozing or active bleeding that required re-operation for haemostasis.
4. Statistical Analysis: All statistical analyses were carried out using the Statistical Package for the Social Sciences (SPSS software version 20.0; SPSS, Inc). Descriptive statistics (mean, standard deviation, minimum and maximum values) were calculated for numerical and categorical variables. The Mann Whitney U test was utilized for comparison of means for inter-group analysis. Significance of intra-group repeated measures were analysed with non-parametric Friedman test. P <0.05 was considered statistically significant.
Results
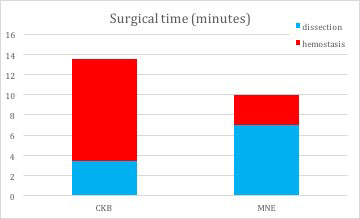
Total of twenty-two patients were operated with a mean age of 26.5±11.6 (Range, 13-43). Patients comprised 12 females (age: 25,0±10,2 mean±SD) and 10 males (age: 28,3±13,5 mean±SD).1 Operative time The mean operative time required to remove one tonsil was 7,0±1,9 minutes for the MNE side and mean hemostasis duration was 3,0±1,4 minutes, the total surgical time for this side was 10,0±2,2 minutes. The mean operative time required to remove one tonsil was 3,5±0,7 minutes for CKB side and mean hemostasis duration was 10,1±4,9 minutes, the total surgical time for this side was 13,5±4,8 minutes. Total time for removal of tonsil was statistically shorter for CKB side, but hemostasis was shorter in MNE side. Total overall operative time required for surgery was statistically less for MNE-operated side. (Table 2)(Figure 2)
Table 2: Required mean surgical time required for each side
 Büyütmek İçin Tıklayın |
Figure 2: Mean surgical time required for surgery for each surgical technique Values show surgical time required in minutes. Times required to dissect and remove the tonsil (a) blue and hemostasis (b) red are given seperately. These two values are added up to calculate the total surgical time (a+b) required for completion of surgery for each side. |
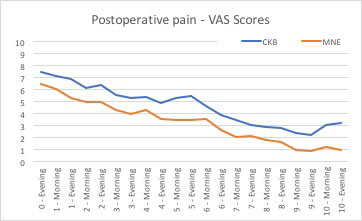
2. Posteroperative pain: Postoperative pain VAS scores on the MNE side was always lower compared to CKB side. Detailed depiction of the analysed data can be seen in Figure 3.
 Büyütmek İçin Tıklayın |
Figure 3: Postoperative pain, VAS score The graph shows the number of postopertive days (X axis). 44 tonsils removed in total. Maximum score is 10 (Y axis), which indicates maximum possible pain, whereas minimum score of 0 indicates no pain at all. |
3. Tonsillar fossa healing scores: Tonsillar fossa healing was evaluated thrice. Fossa healing scores were better on postoperative day #1 and #5 in MNE side compared to CKB side. Healing scores were similar on postoperative day #10 (Table 3)
Table 3: Tonsillar fossa healing
4. Postoperative hemorrhage: Following surgery 4,5% (2 tonsils out of 44) returned with oozing. One of the tonsils were operated with CKB technique and the other was operated with MNE technique. Both patients had history of crispy oral intake although suggested otherwise. None of the patients required reoperation for hemostasis. Therefore postoperative hemorrhage rate for both techniques was the same (4.5%) in our series and similar.
Discussion
Tonsillectomy with monopolar electrocautery is a widely used surgical technique with many advantages [1]. The main trade-off with electrosurgery is heat generated hence the thermal injury- to neighboring tissues which consequently causes variable amount of tissue necrosis. The concept of power density' in electrosurgery is defined as watts per surface area' [8]. A finer/thinner electrocautery tip concentrates the electrical current to a smaller point which results with tissue seperation with lesser dissipation of energy as heat into the surrounding tissues. Less heat dissipation translates into a smaller zone of tissue necrosis and more accuracy during dissection. Current literature shows that a finer tip can give greater precision in dissection and can also affect the dispersion characteristics of the energy used to perform the dissection [8] The implication of this for tonsillectomy is that greater precision in dissecting the tonsil from the underlying muscle can potentially lead to less post-operative discomfort [8,13].For those surgeons who choose to use an electrocautery technique for tonsillectomy, the greater precision of the thinner needles may enhance their results [13] Bovie-tip standard monopolar electrocautery is used around 25 watts. Finer-tip monopolars have a smaller surface area and according to the study carried out by Farnworth et al. [8] and power density (energy per centimeter-squared) is similar to that of Bovie tip with lower values. Therefore MNE was utilized with 10 watts (cut) and 12 watts (coagulation).
The drawback of the microdissector Colorado needle is its cost. Therefore our study's aim was to combine the advantage of finer monopolar electrocautery tip and avoid the high cost of disposable tips. Our preliminary results look promising and we suggest routine utilization of MNE. The cost of MNE is trivial in comparison to Colorado tips. The main disadvantages of MNE is neccesity of good assistance and retraction. Burried tonsils are also technically more demanding. Otherwise MNE offers a controlled and blood-free surgical site. It gives the surgeon precision and control. Following a meticulous and patient dissection with MNE, duration of hemostasis is much more predictable and short - always.
Conclusion
Disposable needle-tip monopolar electrocautery is an affordable and cost-effective alternatife for tonsillectomy. Utilization of MNE does not prolong surgical time: MNE is superior compared to cold-knife dissection followed by bipolar hemostasis in terms of operative duration. Postoperative pain is considerably lower compared to latter technique. Therefore MNE can be a viable option for surgeons looking for costly monopolar electrocautery technique that allows more precision.Reference
1) Leinbach RF, Markwell SJ, Colliver JA, Lin SY. Hot versus cold tonsillectomy: A systematic review of the literature. Otolaryngol - Head Neck Surg. 2003;129(4):360-364. doi:10.1016/S0194-5998(03)00729-0. [ Özet ]
2) Wexler DB. Recovery after tonsillectomy: electrodissection vs. sharp dissection techniques. Otolaryngol Head Neck Surg. 1996;114(4):576-581. http://www.ncbi.nlm.nih.gov/pubmed/8643267. Accessed March 13, 2016. [ Özet ]
3) Aksoy F, Ozturan O, Veyseller B, Yildirim YS, Demirhan H. Comparison of radiofrequency and monopolar electrocautery tonsillectomy. J Laryngol Otol. 2010;124(2):180-184. doi:10.1017/S0022215109991642. [ Özet ]
4) Saravakos P, Hartwein J. Surgical technique and post-tonsillectomy hemorrhage: a single institution's retrospective study. Eur Arch Otorhinolaryngol. 2017 Feb;274(2):947-952. doi: 10.1007/s00405-016-4271-3. Epub 2016 Aug 20. [ Özet ]
5) Ozkiriş M, Kapusuz Z, Saydam L. Comparison of three techniques in adult tonsillectomy. Eur Arch Otorhinolaryngol. 2013 Mar;270(3):1143-7. doi: 10.1007/s00405-012-2160-y. Epub 2012 Aug 22. [ Özet ]
6) Cunningham LC, Chio EG. Comparison of outcomes and cost in patients undergoing tonsillectomy with electrocautery and thermal welding. Am J Otolaryngol - Head Neck Med Surg. 2015;36(1):20-23. doi:10.1016/j.amjoto.2014.08.016. [ Özet ]
7) Hetzler D. In reference to histologic assessment of thermal injury to tonsillectomy specimens: a comparison of electrocautery, coblation, harmonic scalpel, and tonsillotome. Laryngoscope. 2010;120(5):1077. doi:10.1002/lary.20882. [ Özet ]
8) Farnworth TK, Beals SP, Manwaring KH, Trepeta RW. Comparison of skin necrosis in rats by using a new microneedle electrocautery, standard-size needle electrocautery, and the Shaw hemostatic scalpel. Ann Plast Surg. 1993;31(2):164-167. http://www.ncbi.nlm.nih.gov/pubmed/8215134. Accessed March 10, 2016. [ Özet ]
9) Al-Qahtani AS. Post-tonsillectomy hemorrhage. Monopolar microdissection needle versus cold dissection. Saudi Med J. 2012 Jan;33(1):50-4. [ Özet ]
10) Perkins J, Dahiya R. Microdissection needle tonsillectomy and postoperative pain: a pilot study. Arch Otolaryngol Head Neck Surg. 2003;129(12):1285-1288. doi:10.1001/archotol.129.12.1285. [ Özet ]
11) Arbin L, Enlund M, Knutsson J. Post-tonsillectomy pain after using bipolar diathermy scissors or the harmonic scalpel: a randomised blinded study. ≈ Eur Arch Otorhinolaryngol. 2017 May;274(5):2281-2285. doi: 10.1007/s00405-017-4451-9. Epub 2017 Feb 17. [ Özet ]
12) Magdy EA, Elwany S, el-Daly AS, Abdel-Hadi M, Morshedy MA. Coblation tonsillectomy: a prospective, double-blind, randomised, clinical and histopathological comparison with dissection-ligation, monopolar electrocautery and laser tonsillectomies. J Laryngol Otol. 2008;122(3):282-290. doi:10.1017/S002221510700093X. [ Özet ]
13) Modi VK, Monforte H, Geller KA, Koempel JA. Histologic assessment of thermal injury to tonsillectomy specimens:a comparison of electrocautery, coblation, harmonic scalpel, and tonsillotome. Laryngoscope 2009;119:22482251 [ Özet ]




