THE ROLE OF THE GROWTH FACTORS IN THE PATHOGENESIS OF COMPENSATORY TURBINATE HYPERTROPHY
2Sağlık Bilimleri Üniversitesi Dışkapı Yıldırım Beyazıt SUAM, Kulak Burun Boğaz Kliniği, Ankara, Turkey
3Sağlık Bilimleri Üniversitesi Ankara Atatürk EAH, Patoloji Kliniği, Ankara, Turkey
Summary
Introduction: Inferior turbinate hypertrophy (ITH) is oftenly associated with contolateral nasal septal deviation.This counterbalanced mechanism protects nasal mucosa from excess airflow which may cause drying and crusting.Objectives: This study was designed to elucidate the roles of vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), basic fibroblast growth factor (b-FGF), nerve growth factor (NGF) and bone morphogenetic protein 2 (BMP-2) in the pathogenesis of compensatory contralateral turbinate hypertrophy accompanying nasal septal deviation in comparison between hypertrophied and normal turbinates.
Material and Methods: Forty nine cases with septal deviation and contralateral compensatory ITH who underwent septoplasty plus bilateral partial inferior nasal turbinate resection were included in this single center prospective study. Bilateral inferior turbinate specimens including tissue samples obtained from epithelium, submucosal duct, perivascular area and bone were collected for each patient to perform immuno-histochemical analysis of anti-VEGF, anti-EGF, anti-BMP-2, anti-b-FGF and anti-NGF positivity in the compensatory hypertrophied versus normal inferior turbinates.
Results: In both ITH group and normal turbinate group; tissue samples obtained from epithelium, submucosal duct, perivascular area and bone showed similar rates in anti-VEGF, anti-EGF, anti-b-FGF, anti-NGF and anti-BMP-2 scoring. There was no statistical significant difference between hypertrophied and normal inferior turbinates in terms of expression of growth factors. This study is one of the first to evaluate the contribution of growth factors in the compensatory ITH in patients with nasal septum deviation.
Conclusion: Present study revealed varying levels of expression for each growth factor in both turbinates, whereas no significant difference between hypertrophied and normal inferior turbinates in terms of expression of growth factors in tissue samples obtained from epithelium, submucosal duct, perivascular area and bone. Additional mechanisms and genetic alterations should be considered in further researches.
Introduction
Compensatory contralateral inferior turbinate hypertrophy (ITH) accompanying nasal septal deviation is a very common entity in otorhinolaryngology practice, while overgrowth of the contralateral inferior turbinate is considered to originate to protect the more patent nasal side from adverse effects of excess airflow [1,2].Despite its well-known clinical occurrence, ITH has received little attention in the literature with limited data on the composition and typical histological features of hypertrophic versus normal turbinates as well as on the role of tissue remodeling and underlying molecular mechanisms in turbinate hypertrophy [2,3]. While mucosal elements, venous sinusoids as well as bone have been considered to participate in the enlargement of turbinate, the exact pathogenesis of compensatory ITH has not yet been well-established [3-5].
Sino-nasal osteogenesis, mucosal hypertrophy, fibrosis, sub-epithelial collagen deposition and angiogenesis are considered amongst the progressive tissue remodeling changes that affect normal sinonasal physiology [6-8]. Hence, with advances in understanding the pathophysiological processes underlying diseases, growth factors attracted attention in the pathogenesis of sinonasal conditions with demonstration of the possible role of vascular endothelial growth factor (VEGF), epidermal growth factor (EGF), basic fibroblast growth factor (b-FGF), nerve growth factor (NGF) and bone morphogenetic protein 2 (BMP-2) in allergic rhinitis, nasal polyposis, chronic sinusitis and asthma [9-18]. To our knowledge, there is no study in the literature regarding the effects of the aforementioned growth factors on ITH. The present study was therefore designed to elucidate the roles of VEGF, EGF, BMP-2, b-FGF and NGF in the pathogenesis of compensatory contralateral ITH accompanying nasal septal deviation in comparison between hypertrophied and normal inferior turbinates.
Methods
Study populationA total of 49 patients with septal deviation and contralateral compensatory inferior turbinate hypertrophy who underwent septoplasty plus bilateral partial inferior nasal turbinate resection were included in this single-center prospective study. Patients aged ≥18 years; diagnosed with Mladina types 2, 3 and 4 septal deviation and contralateral compensatory ITH by both anterior rhinoscopy end endoscopic examination were included in the study. Patients with systemic diseases, acetylsalicylic acid allergy, asthma, nasal polyposis, and prior nasal turbinate or septal surgery were excluded.
Written informed consent was obtained from each subject following a detailed explanation of the objectives and protocol of the study which was conducted in accordance with the ethical principles stated in the Declaration of Helsinki and institutional ethical approval was obtained with a number of 09/46-18).
Study parameters
Following surgery, resected bilateral inferior turbinate specimens including tissue samples obtained from epithelium, submucosal duct, perivascular area and bone were collected for each patient to perform immuno-histochemical analysis of anti-VEGF, anti-EGF, anti-BMP-2, anti-b-FGF and anti-NGF positivity in the compensatory hypertrophied versus normal contralateral inferior turbinates. All histopathologic changes and immune-histochemical staining were performed by the same pathologist.
Classification of septal deviation
Septal deviation was classified based on deviation of nasal septum, side of deviation, bilaterality, and contact of inferior turbinate with septum according to classification system described by Mladina et al. in 2008 [9]. In accordance with inclusion criteria, patients with Mladina type 2 (a unilateral vertical septal ridge in the valve region that touches the nasal valve, thus diminishing the physiologic valve angle <15°), type 3 (a unilateral vertical ridge located more deeply in the nasal cavity opposite the head of the middle turbinate) and type 4 (a bilateral deformity consisting of type 2 on one side and type 3 on the other) septal deviations were selected.
Surgery
All patients were operated under general anesthesia by the same surgeon. Following septoplasty with submucosal resection, the deviated septum was corrected and then a bilateral inferior turbinate partial resection was performed. For study purposes, inferior turbinate resection material which includes mucosal and bony tissue samples was obtained during the turbinate partial resection.
Immuno-histochemical analysis
Immuno-histochemical analyses were performed using the streptoavidin-biotin method and commercial kits were employed (Universal LSAB kit- Scytek Laboratories UltraTek HRP anti Lab Pack, USA). All specimens were independently buffered and fixated with formaldehyde, and paraffin sections were obtained. Five micrometer sections were stained with hematoxylin- eosin followed by VEGF, EGF, b-FGF, NGF and BMP-2 antibody stain applications. Positive controls were colon cancer tissue for VEGF, EGF and b-FGF, thyroid tissue for NGF, and small intestine tissue for BMP-2. Negative controls were also added for each study. Stained samples were evaluated by a single pathologist in a single blind manner without notification of the clinical data. Cytoplasmic staining was evaluated for each antibody. The scoring system was based on the percentage of densely stained cells in the surface epithelium, submucosal ducts, perivascular area and bone with consideration of <50% cytoplasmic staining to be negative and ≥50% cytoplasmic staining to be positive for study purposes. Staining density were evaluated for all the antibodies as follows; negative (1), mild to moderate (2), dense (3). Percentage of stained cells were evaluated in 5 groups ;
1. Less than 10%
2. 10% to 24%
3. 25%to 49%
4.50%-74
5. More than 75%
For every case density and percentage were multiplied and a staining score was calculated. Scores less than 50% was accepted as negative staining and scores above 50% was accepted aspositive staining.
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences (SPSS version 17.0, Chicago, IL, USA). The difference between hypertrophied and normal turbinate groups was analyzed using Pearson Chi-square test. Statistical significance was accepted when p<0.05.
Results
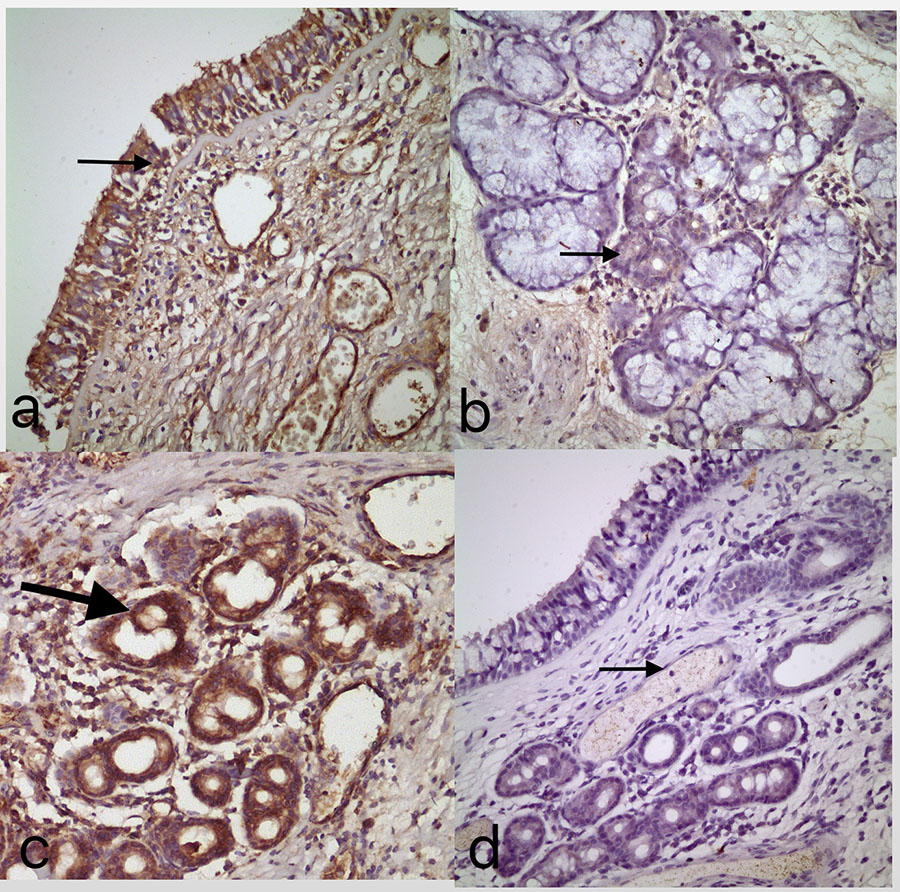
Mean age was 30.8 (±10.5) years that ranged from 18 to 61 years. There were 34 (69.4%) male and 15 (30.6%) female patients.Staining patterns of hypertrophied and normal inferior turbinates were summarized in Table 1, while Fig 1 shows staining patterns of hypertrophied inferior turbinate including anti-EGF staining of the turbinate epithelium (Fig 1a), anti-b-FGF staining of submucosal ductus area (Fig 1b), anti-NGF staining of the perivascular area (Fig 1c) and anti-BMP-2 staining of bone (Fig 1d).
 Büyütmek İçin Tıklayın |
Fig 1: Immuno-histochemical staining of inferior turbinate specimens a) Anti-EGF staining of the epithelium b) Anti-FGF staining of the submucosal ductus area c) Anti-NGF staining of the perivascular area d) Anti-BMP staining of the bone specimens; obtained from the resected hypertrophic turbinate |
In ITH cases; anti- VEGF expression was commonly encountered in perivascular area (49%) and bone (49%) while anti-EGF was predominant in the epithelial tissue (89.8%) as can be expected. Anti-FGF positivity was most common in epithelial tissue (59.2%). Anti-NGF positivity was in 73.5% in bone tissue and anti-BMP-2 positive in equal amounts both in submucosal and perivascular tissue In both groups, expression of anti-VEGF was higher in perivascular samples, anti-EGF and anti-b-FGF in perivascular and epithelial samples, anti-NGF in bone samples, and anti-BMP-2 in submucosal duct and perivascular samples as compared with other tissue samples analyzed for the same growth factor.
Anti-EGF was the most common growth factor expressed in epithelium, anti-EGF in perivascular area and anti-NGF in bone in both groups, whereas in submucosal duct BMP-2 in hypertrophied and anti-FGF in normal turbinate group was the most commonly expressed growth factor; as compared with other growth factors analyzed in the same tissue sample. The distribution of staining properties of examined tissues can be seen on Table 1.
Discussion
Nasal septal deviation is usually associated with controlateral inferior turbinate hypertrophy. The questions of how to treat patients with compensatory ITH and whether to add turbinate resection to septoplasty is an ongoing debate so far. Unilateral ITH coexistent with septum deviation on the concave side is frequently encountered sign during nasal examination clear developmental reasons have been documented for ITH, but it is assumed that this counterbalanced mechanism characterized by compensatory hypertrophy originates for protection of the more patent nasal side from excess airflow with its drying and crusting effects on nasal mucous membranes [10,11]. In a recent study of Aslan et al claim that bone hypertrophy evolves with age and is rather compensatory than congenital. They investigated septal deviation cases in two groups as pediatric cases and adults [12]. They found significant hypertrophy of the soft tissue component of the turbinate in adults with deviation compared with children with deviation, again supporting the claim that the soft tissue hypertrophy evolves with age and is compensatory and not congenital.In patients with compensatory ITH secondary to NSD, the underlying histopathological or molecular mechanisms of ITH is not well established yet. In present study we investigated mucosa, submucosal area, bone and perivascular tissues in terms of various growth factors. VEGF, a glycoprotein molecule produced in the endothelium, has been associated with increased vascular permeability, endothelial proliferation, growth and migration. The role of VEGF expression in the pathogenesis of nasal polyposis is well-establised [13,14]. Kirmaz et al. showed increased expression of VEGF in inferior turbinate biopsy samples from nasal mucosa in patients with seasonal allergic rhinitis (SAR) as compared with controls and emphasized the likely role of increased angiogenesis in the remodeling of nasal mucosa of subjects with SAR [15].
Although vascular tissue responsible for the congestion of the turbinate is expected to be denser on the hypertrophied side and VEGF was in fact more commonly expressed in perivascular (49%) than in other tissue samples in our cohort, no significant difference was noted between hypertrophied and normal turbinate samples in terms of VEGF expression. To best of our knowledge, there is no previous study comparing VEGF expression between turbinates of the same individuals with septal deviation and analyzing the effects of vascularization on nasal turbinate hypertrophy in the current literature. Hence our findings may suggest VEGF has no significant contribution to the mechanisms underlying the ITH.
EGF is known to stimulate epidermal and mesodermal-derived cellular proliferation and to act in synergy with VEGF[16]. Although VEGF expression was more common in perivascular area than in other tissue samples, the most commonly expressed growth factor in perivascular area was EGF in our study. In a previous study by Ding et al. EGF and EGF receptor expression was shown in the basal epithelium in nasal polyposis patients and indicated to be similar between patients with and without chronic sinusitis [17]. They concluded that chronic inflammation induces EGF and its receptor expression. In our study, we observed that EGF was expressed over 80% of the epithelium in both groups, yet demonstrated no significant difference between hypertrophied and normal turbinates.
BMP acts on differentiated perivascular connective tissue cells in adults and takes place in osteoinduction [18]. As a member of the family, BMP-2 is the one with greatest osteoinductive capacity and considered to act in synergy with b-FGF. BMP was more commonly expressed in submucosal duct (49%) than in other tissue samples in our study.
Maire et al. reported that increased expression of BMP was associated with increased differentiation through the respiratory epithelium[19]. We showed similar anti-BMP-2 staining in both turbinates, particularly in perivascular (49%) and submucosal duct (49%) samples. Notably, submucosal duct was the only area that differed between ITH and control groups in terms of the most commonly expressed growth factor in our study. BMP-2 in hypertrophied turbinates and b-FGF in normal turbinates were predominantly expressed growth factors. This seems notable given that tissue remodeling processes throughout the organism are considered to be largely governed by the FGF and BMP families of cytokines [3].
FGF causes proliferation, differentiation, migration, extracellular matrix production and vascularization, while b-FGF is known to be more potent than acidic FGF (20). The role of b-FGF has been studied previously in nasal polyps and olfactory mucosa and it was shown to be mitogenic on the respiratory epithelium [21,22]. No study regarding its role in inferior turbinate hypertrophy has been published up to date. In a past study on the effects of b-FGF on nasal polyps by Powers et al., b-FGF expression was shown in basal and suprabasal epithelial cells along with mast cells and suggested to play an important role in the pathophysiology of polyposis [23]. b-FGF was more commonly expressed in epithelium and perivascular space than in submucosal ducts and bone in our study, while it was the leading growth factor expressed in submucosal duct samples obtained from normal turbinates. This seems to emphasize the role of close contact between the normal turbinate and the deviated septum results in increased inflammatory response and b-FGF production and against chronic irritation [24].
Although not significant, lower expression of b-FGF in epithelial and NGF in perivascular samples of hypertrophied than normal turbinates seems to indicate the likelihood of increased inflammatory reactions and thus increased expression of growth factors in the normal turbinate due to its close contact with septum. This seems also to emphasize the need for more objective comparison of hypertrophied and normal turbinates in terms of inflammatory cell count in future studies.
Despite the studies that reveal increased levels of NGF in nasal and bronchoalveolar lavage fluids in patients with allergic rhinitis and asthma limited data are available on the role of NGF in rhinologic pathologies [25,26]. Analysis of human nasal turbinate sections by Wu et al. revealed submucosal glands, nasal epithelium, and eosinophils to be major sources of NGF in the human nasal mucosa [27]. Bresciani et al. studied showed dense staining with NGF in the mucosal epithelium and submucosal glands in patients with persistent allergic rhinitis [28]. In our study, expression of NGF was higher in bone than in other tissue samples. This seems consistent with the consideration of neurotrophins, including NGF, to be expressed in subchondral bone and by bone forming cells, and to have both autocrine and paracrine roles in bone formation [29]. The innovative study of Berger et al. Focused on the dimensions and composition of the compensatory ITH in patients with nasal septum deviation, enlargement of bony tissue was more than the enlargement of submucosal and mucosal tissue. They concluded that bone expansion rather than mucosal hypertrophy plays a crucial role in turbinate hypertrophy thickening so that their findings support the decision to excise the inferior turbinate bone at the time of septoplasty [2]. In that study histopathological evaluation of the three layers (medial and lateral mucosal layers and a central osseous tissue) were performed but it lacks further investigation such as immune-histochemical staining.
In our study in addition to previous studies all layers of inferior turbinate was stained immuno-histochemically.
Nonetheless, given that BMP-2, b-FGF and NGF in our cohort were the growth factors with highest expression in submucosal duct of hypertrophied turbinates, in submucosal duct of normal turbinates and in bone of both hypertrophied and normal turbinates, respectively; our findings emphasize that the role of bone expansion in turbinate hypertrophy should be studied more intensively. In fact, on the basis of evidence on outstanding growth of the bone rather than that of the mucosa in turbinate hypertrophy, an alternative hypothesis might be speculated unilateral growth of the turbinate bone that may exert pressure on the growing nasal septum during childhood and adolescence and eventually cause it to deviate to the contralateral side of the nose [2].
To our knowledge, this is the first study evaluating VEGF, EGF, BMP-2, b-FGF and NGF FGF expression in ITH in comparison to normal turbinates in same patients. Further investigation is required to determine the role of growth factor expressions in turbinate remodeling.
Possible limitations of this study include the semi-quantitative nature of immunohistochemistry, which is a well-known issue in the characterization of protein expression. Future studies may utilize additional quantitative techniques such as Western Blot or real time PCR to address such a problem. Another important point is the mean age of the patients included in the study. As the compensatory changes have already occurred in the hypertrophic turbinates of adult septoplasty cases, growth factor expressions may have returned to their basal levels compared to their pediatric counterparts. Another limitation is the lack of comparison between normal concha tissue and hypertrophied one. This limitation might be the cause of insignificant results in terms of growth factor levels. Future studies should consider these factors and focus on molecular mechanisms affecting growth factor expresssions in compensatory hypertrophy.
Conclusion
The present study is the first to evaluate the contribution of growth factors in the compensatory ITH in patients with nasal septum deviation. Our findings revealed varying levels of expression for each growth factor in both turbinates, whereas no statistical significant difference between hypertrophied and normal inferior turbinates in terms of expression of growth factors in epithelium, submucosal duct, perivascular area and bone samples. We believe that detailed studies with quantitative methods comprising capillary density examination, inflammatory cell count in the turbinate as well as growth factor expression and studies on younger patients whose nasal turbinates are still in the phase of growth might yield more conclusive results.Reference
1) Elahi MM, Frenkiel S, Fageeb N. Paraseptal structural changes and chronic sinus disease in relation to the deviated septum. J Otolaryngol 1997; 26: 236-240 [ Özet ].
2) Berger G, Hammel I, Berger R, Avraham S, Ophir D. Histopathology of the inferior turbinate with compensatory hypertrophy in patients with deviated nasal septum. Laryngoscope 2000; 110: 2100-2105 [ Özet ].
3) Sautter NB, Delaney KL, Hausman FA, Trune DR. Tissue remodeling gene expression in a murine model of chronic rhinosinusitis. Laryngoscope 2012; 122:711-717. [ Özet ].
4) Grymer LF, Illum P, and Hilberg O. Septoplasty and compensatory inferior trubinate hypertrophy: A randomized study evaluated by acoustic rhinometry. J Laryngol Otol 107:413417, 1993 [ Özet ].
5) Tombu S, Daele J, Lefebvre P. Rhinomanometry and acoustic rhinometry in rhinoplasty. B-ENT. 2010;6 Suppl 15: 3-11 [ Özet ]
6) Cho SH, Shin KS, Lee YS, Jeong JH, Lee SH, Tae K, Kim KR. Impact of chronic rhinosinusitis and endoscopic sinus surgery on bone remodeling of the paranasal sinuses. Am J Rhinol 2008; 22:537-541 [ Özet ]
7) Giacchi RJ, Lebowitz RA, Yee HT, et al. Histopathologic evaluation of the ethmoid bone in chronic sinusitis. Am J Rhinol 2001; 15: 193-197 [ Özet ]
8) Sobol SE, Fukaskusa M, Christodoulopoulos P, et al. Inflammation and remodeling of the sinus mucosa in children and adults with chronic sinusitis. Laryngoscope 2003; 113:410-414 9) Mladina R, Cujić E, Subarić M, Light JP, Jacobs JB. Nasal septal deformities in ear, nose, and throat patients: an international study. Am J Otolaryngol 2008; 29: 75-82 [ Özet ]
10) Vento SI, Wolff CH, Salven PJ, Hytönen ML, Ertama LO, Malmberg CH. Vascular permeability factor/vascular endothelial growth factor in nasal polyps. Acta Otolaryngol Suppl 2000; 543:170-174 [ Özet ]
11) Muluk NB, Atasoy P, Arikan OK, Koc C. Role of vascular endothelial growth factor in the pathogenesis of nasal polyps. J Otolaryngol 2007; 36: 357-366 [ Özet ]
12) Aslan G, Uzun L, Ugur MB, Uckurt YS, Sagun OF, Yazicilar O. Unilateral inferior turbinate bone hypertrophy: is it compensatory or congenital? Am J Rhinol Allergy 2013; 27: 255-259 [ Özet ]
13) Farmer SEJ, and Eccles R. Chronic inferior turbinate enlargement and the implications for surgical intervention. Rhinology 44:234238, 2006 [ Özet ].
14) Egeli E, Demirci L, Yazıcı B, and Harputluoglu U. Evaluation of the inferior turbinate in patients with deviated nasal septum by using computed tomography. Laryngoscope 114:113117, 200 [ Özet ].
15) Kirmaz C, Ozbilgin K, Yuksel H, Bayrak P, Unlu H, Giray G, Kiliccioglu B. Increased expression of angiogenic markers in patients with seasonal allergic rhinitis. Eur Cytokine Netw 2004; 15: 317-322 [ Özet ].
16) Ding GQ, Zheng CQ, Bagga SS. Up-regulation of the mucosal epidermal growth factor receptor gene in chronic rhinosinusitis and nasal polyposis. Arch Otolaryngol Head Neck Surg 2007; 133:1097-1103 [ Özet ].
17) Chen D, Zhao M, Mundy GR. Bone morphogenetic proteins. Growth Factors 2004;22: 233-241 [ Özet ].
18) Maire M, Chaubet F, Mary P, Blanchat C, Meunier A, Logeart-Avramoglou D. Bovine BMP osteoinductive potential enhanced by functionalized dextran-derived hydrogels. Biomaterials 2005; 26: 5085-5092 [ Özet ].
19) Kim HJ, Jung HH, Lee SH. Expression of acidic fibroblast growth factor and basic fibroblast growth factor in nasal polyps. Acta Otolaryngol 2006; 126:600-605 [ Özet ].
20) Barraud P, He X, Zhao C, Ibanez C, Raha-Chowdhury R, Caldwell MA, Franklin RJ. Contrasting effects of basic fibroblast growth factor and epidermal growth factor on mouse neonatal olfactory mucosa cells. Eur J Neurosci 2007; 26: 3345-3357 [ Özet ].
21) Sansoni ER, Sautter NB, Mace JC, Smith TL, Yawn JR, Lawrence LA, Schlosser RJ, Soler ZM, Mulligan JK. Vitamin D3 as a novel regulator of basic fibroblast growth factor in chronic rhinosinusitis with nasal polyposis. Int Forum Allergy Rhinol. 2015;5(3):191-6 [ Özet ].
22) Powers CJ, McLeskey SW, Wellstein A. Fibroblast growth factors, their receptors and signaling. Endocr Relat Cancer 2000; 7: 165-197 [ Özet ].
23) Qu Z, Huang X, Ahmadi P, Stenberg P, Liebler JM, Le AC, Planck SR, Rosenbaum JT.. Synthesis of basic fibroblast growth factor by murine mast cells. Regulation by transforming growth factor beta, tumor necrosis factor alpha, and stem cell factor. Int Arch Allergy Immunol 1998; 115: 47-54 [ Özet ].
24) Raap U, Braunstahl GJ. The role of neurotrophins in the pathophysiology of allergic rhinitis. Curr Opin Allergy Clin Immunol 2010; 10: 8-13 [ Özet ].
25) Scuri M, Samsell L, Piedimonte G. The role of neurotrophins in inflammation and allergy. Inflamm Allergy Drug Targets 2010;9: 173-180 [ Özet ].
26) Wu X, Myers AC, Goldstone AC, Togias A, Sanico AM. Localization of nerve growth factor and its receptors in the human nasal mucosa. J Allergy Clin Immunol 2006; 118: 428-433 [ Özet ].
27) Bresciani M, Lalibertè F, Lalibertè MF, Gramiccioni C, Bonini S. Nerve growth factor localization in the nasal mucosa of patients with persistent allergic rhinitis. Allergy 2009; 64: 112-117 [ Özet ].
28) Asaumi K, Nakanishi T, Asahara H, Inoue H, Takigawa M. Expression of neurotrophins and their receptors (TRK) during fracture healing. Bone 2000; 26: 625-633 [ Özet ].




