THE PROTECTIVE EFFECT OF THYMOL AGAINST CISPLATIN-INDUCED OTOTOXICITY: AN EXPERIMENTAL ANIMAL STUDY
2Bezmialem Vakıf Üniversitesi, Kulak Burun Boğaz , İstanbul, Turkey
3Marmara Üniversitesi, Histoloji ve Embriyoloji, İstanbul, Turkey
4Bezmialem Vakıf Üniversitesi, Biyokimya, İstanbul, Turkey
Summary
Objective: The aim of this study is to investigate the protective effect of thymol against cisplatin- induced ototoxicity by evaluating audiological, biochemical and histopathological parameters.Materials and methods: Thirty-two male rats were divided into four groups (control, cisplatin, thymol + cisplatin and thymol) including eight rats each. 150 mg/kg/day thymol was given for 5 days orally. Single dose cisplatin(16 mg/kg) was also given via intraperitoneal route. Distortion product otoacoustic emission(DPOAE) and auditory brainstem response(ABR) tests from both ears were performed in all groups at the beginning of the study and also on days 6. Intracardiac blood samples and their cochleas were taken on day 6 for assessment of biochemical and histopathological(including TUNEL) parameters.
Results: In audiological assessment, in group 2(cisplatin), there were significant decreases in DPOAE values and significant increases in ABR thresholds on days 6 as compared with other groups. In Groups 1(control), 3(thymol + cisplatin) and 4(thymol) there was no significant difference between the pre- and posttreatment DPOAE and ABR results.
In biochemichal analyses, the total oxidant status(TOS) value was significantly higher in group 2(cisplatin) than in the other groups. The total antioxidant status(TAS) value was significantly higher in group 3(thymol+cisplatin) than in group 2.
In the histopathological examinations, there was significant reduction of the number of TUNEL-positive cells in the group 3(thymol+cisplatin) compared to the group 2(cisplatin).
Conclusions: The audiologic tests, biochemical results and histologic findings revealed that thymol may have protective effect against cisplatin ototoxicity by increase antioxidant levels and reduce oxidative stress parameters.
Introduction
Cisplatin (cis-diamine-dichloroplatinum) is an effective antineoplastic drug that is frequently used in the treatment of cancer of the lungs, the head and neck, the ovaries, and the bladder. Cisplatin exerts its anticancer effect by inhibiting the synthesis of deoxyribonucleic acid and increasing the level of reactive oxygen radicals. In addition, it leads to a reduction of intracellular glutathione, which is a cause of mitochondrial damage, resulting in lipid peroxidation[1].However, cisplatin has dose-dependent side effects, such as nephrotoxicity, ototoxicity, neurotoxicity, and bone marrow toxicity. Although nephrotoxicity can be controlled using hydration treatment and diuretics, no routine treatment modality is currently available for ototoxicity[2], which may manifest itself hours or days after cisplatin treatment. Cisplatin-induced ototoxicity develops as bilateral, progressive, and irreversible sensorineural hearing loss, initially at high frequencies, but subsequently at all frequencies[3].
The cellular and molecular mechanism of cisplatin ototoxicity is not yet fully understood. It has been stated that cisplatin causes an excessive production of free oxygen radicals in the organ of Corti, the stria vascularis, the spiral ligament, and the spiral ganglionic cells, leading to oxidative damage to the cochlea and outer hair cells (OHCs), resulting in apoptosis[4,5]. Furthermore, cisplatin reduces antioxidant enzymes in the cochlea. A number of studies examining the protective effect of antioxidant agents, such as lipoic acid, resveratrol, curcumin, Gingko biloba extract, and thymoquinone, against the ototoxicity of cisplatin, have been published[5-9]. However, to date, no FDA-approved product has shown effectiveness in the prevention of cisplatin-induced ototoxicity[5].
Thymol (5-methyl-2-isopropylphenol) is a natural monoterpene phenolic compound that is found in various herbs, such as thyme, zataria, and oregano[10]. It has a wide range of uses in the pharmaceutical, cosmetics, and perfume industries, as well as in sweetening and spicing comestibles[10,11]. Thymol also has significant antimicrobial, anti-inflammatory, and antioxidant effects, protecting the liver, erythrocytes, and kidneys from oxidative stress[12-17]. This protection against oxidative stress is related to its being an antioxidant, thereby scavenging free oxygen radicals and preventing lipid peroxidation[14,18-20].
In addition, it has been reported that thymol is cytoprotective against radiation-induced damage[21], and is effective as a chemotherapeutic agent in the treatment of cancer[22-26]. Previous studies have also shown that thymol is protective against cisplatin-induced nephrotoxicity[15,16]. However, the effectiveness of thymol with regard to the ototoxicity of cisplatin has not yet been studied. We therefore investigated whether thymol is protective against cisplatin ototoxicity, via an evaluation of audiological, biochemical, and histopathologic parameters.
Methods
The study was conducted at the Experimental Animal Studies Laboratory of Istanbul University, Istanbul, Turkey, following approval by the Ethics Committee on Animal Research of Istanbul University.
Animals
A total of 32 adult male Sprague Dawley rats weighing 280 300 g, and with a positive Preyer reflex, were used, and a 2.7mm 0° endoscope was used to examine their tympanic membranes and external ear canals. Rats with cerumen in the ear canal and those showing signs of otitis media or tympanic membrane perforation were excluded. The animals were maintained at a constant temperature of 25°C in separate cages in a temperature-controlled room with a 12 h light/dark cycle. They had access to food and water, ad libitum. Rats with normal hearing defined as distortion product otoacoustic emission (DPOAE) values of 6 decibels sound pressure level (dB SPL) above the signal-to-noise (SNR) ratio were included.
Chemicals
Cisplatin was obtained from Hospira (50 mg/50mL, Warwickshire, UK), and thymol and corn oil were purchased from the Sigma-Aldrich Chemical Co. (St Louis, Missouri, USA). The thymol was dissolved in the corn oil, and the thymol doses were selected on the basis of previously published data[15].
Experimental groups
The experimental animals were randomly divided into four groups (groups 14) of eight (n=8) rats:
_ Group 1: control; the rats received oral corn oil (1 ml/day) via a gastric tube for 5 days.
_ Group 2: cisplatin; the rats received a single intraperitoneal dose of cisplatin (16 mg/kg) two days after corn oil administration.
_ Group 3: thymol+cisplatin; the rats received oral thymol (150 mg/kg/day, dissolved in 1ml corn oil) via gastric tube two days prior to cisplatin injection; a single intraperitoneal dose of cisplatin (16 mg/kg) was administered on day 3, and thymol administration was continued on day 5.
_ Group 4: the rats received oral thymol (150 mg/kg/day, dissolved in 1ml corn oil) via a gastric tube for 5 days.
All rats were anesthetized via an intra¬peritoneal administration of ketamine hydrochloride (40 mg/kg, Ketalar, Eczacibasi, Istanbul, Turkey) and xylazine hydrochloride (5 mg/kg, Rompun, Bayer, Istanbul, Turkey) at the beginning of the study and again on day 6. DPOAE and auditory brainstem response (ABR) measurements were taken following anesthesia. On day 6, the rats were sacrificed using ketamine and xylazine; blood samples were obtained by intracardiac puncture, and biochemical parameters were determined. In addition, their cochleas were harvested for histopathological observations on day 6, placed in 10% buffered formaldehyde and sent for pathological examination. All surgical procedures were performed under a dissecting microscope, using sterilized instruments. The individuals who carried out the audiological and biochemical measurements, as well as the histopathological examination, were unaware of to which group each individual animal belonged.
Audiological evaluation
Distortion-product oto-acoustic emission
A Neurosoft Neuro-audio device (Ivanova, Russia) was used to measure DPOAEs. An infant probe was placed in the external ear canal and measurements were taken from both ears in a silent room. DPOAEs were measured at different frequencies ranging from 988 to 11429 Hz (988, 2222, 3200, 4444, 5000, 6154, 8000, 8889, 10000, and 11429) and the intensity levels were recorded as L1 for the f1 frequency (65 dB SPL) and L2 for the f2 frequency (55 dB SPL) (f1/f2 ratio = 1.22). The results were evaluated as SNR ratio values and compared according to frequency and group.
Auditory brainstem response
ABR measurements were taken from both ears of each rat, using a Neurosoft Neuro-audio device (Ivanova, Russia) and an ER-2 ear phone, and the recordings were acquired through two channels. The ABR responses were recorded by subdermal needle electrodes that were placed under the skin. A tone-burst stimulus of 16 kHz was used as an auditory stimulus, with the following settings: band-pass filters of 30-2000 Hz and a repeat rate of 21/second; in addition, the stimuli were calibrated. The threshold was determined by starting at 100 dB SPL, and decreasing by increments of 10 dB until the threshold was reached. Repeatability was confirmed, and the threshold determination was developed over two tests. The ABR threshold was defined on the fifth wave.
Biochemical evaluation
Blood samples obtained from all of the rats were centrifuged for 15 minutes at 3000 rpm, and the serum was separated and stored at -80°C. Total antioxidant status (TAS) and total oxidant status (TOS) were measured using the Rel Assay Diagnostics kit (Mega Tip San. ve Tic. Ltd. Sti., Gaziantep, Turkey), and the oxidative stress index (OSI) was calculated from the TAS and TOS results (OSI: TOS/TASx100).
TAS measures the combined activity of antioxidants and the total antioxidant level, thus producing the resulting antioxidant status[27], while TOS is an indicator of the total oxidant levels[28]. The OSI provides a more accurate indicator of oxidative stress in the body, as this ratio accounts for the sum of all oxidant and antioxidant activities.
Histopathological examination
Light microscopic preparation
All animals were sacrificed by decapitation under deep anesthesia, and their temporal bones were immediately removed. The cochleas were dissected under a dissecting microscope and fixed with 10% buffered formalin. Following decalcification with 10% EDTA 2Na (pH 7.4), distilled water was used to wash away the decalcification solution, and the tissues were processed for evaluation under light microscopy. They were then dehydrated in graded concentrations of ethanol series (70%, 90%, 96%, and 100%) and cleaned in xylene. Finally, the samples were embedded in paraffin blocks. Longitudinal 5 µm thick sections passing parallel to the modiolus were deparaffinized, hydrated, and stained using the terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick-end labeling (TUNEL) method for determining apoptotic cells.
The TUNEL method
TUNEL staining was used to evaluate the extent of apoptosis in the organ of Corti and the stria vascularis of the rats in all groups. The TUNEL staining assay kit was used in accordance with the manufacturers user manual (Millipore ApopTag Plus Peroxidase In Situ Apoptosis Kit S7101, Temecula, CA, USA). After staining with Mayer's hematoxylin, sections were coverslipped with Entellan mounting medium. TUNEL-positive cells in the organ of Corti and stria vascularis were counted in randomly chosen fields of each sample under a light microscope (Olympus BX51, Tokyo, Japan) with a 40x objective lens, and photographed with a digital camera (Olympus DP72, Tokyo, Japan). Three of the 5 cochlear sections (2 basal turns, 2 medial turns and 1 apical turn) were evaluated in each slide. The mean number of TUNEL-positive cells . in the stria vascularis and organ of Corti were recorded for each slide.
All of the histological examinations was carried out by two researchers (D. Akakin and K. Koroglu), who were blinded to the drug administration groups.
Statistical analysis
Statistical analysis was carried out using Statistical Package for the Social Sciences software, version 22.0 (SPSS Inc, Chicago, IL, USA). All quantitative variables were estimated using measures of central location (i.e., mean and median) and measures of dispersion (i.e., standard deviation), and data normality was checked using the Kolmogorov-Smirnov test.
One-way analysis of variance (ANOVA) was used for intergroup comparisons of DPOAE and ABR values (the differences between groups were considered statistically significant at p<0.05). The Tukey honest significant difference (HSD) post hoc test was used to determine the differences between groups.
A paired-samples t-test was used to compare the DPOAE and ABR values before and after drug administration in each group (differences were considered statistically significant at p<0.05).
One-way ANOVA was used in the evaluation of between-groups differences in biochemical parameters (the differences between groups were considered statistically significant at p<0.05). The Tukey HSD post hoc test was used to determine which groups differed.
The Kruskal-Wallis test was used to compare the differences in the number of TUNEL-positive cells (the differences between groups were considered statistically significant at p<0.05). The Dunn's test was used to determine the differences between the groups.
Results
One animal from the cisplatin group and one animal from the thymol group died under anesthesia, and 30 animals completed the study without any complications.
Distortion product oto-acoustic emission
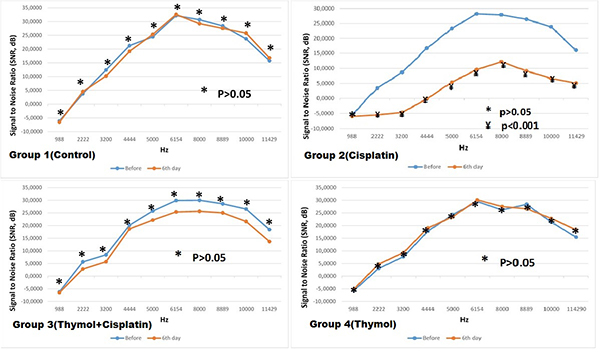
In group 2 (cisplatin), the SNR ratio values (SNR, dB) were significantly lower than the initial values on day 6, with the exception of the 998 frequency (p<0.001). In groups 1 (control), 3 (thymol+cisplatin), and 4 (thymol), no significant difference was found between the SNR values initially observed and those measured on day 6 (p>0.05) (Fig. 1). In the comparison between the groups, although there was no difference in the initial values, the values were significantly lower (p<0.008) in group 2 (cisplatin) for all frequencies, with the exception of 998, on day 6.
 Büyütmek İçin Tıklayın |
Figure 1: Variations in SNR (signal-to-noise ratio) values of distortion products otoacoustic emissions (DPOAEs) in all groups at before and after treatment on day 6. *For the comparison within group, paired samples t test was applied (P<0.05 was accepted as statistically significant). |
Auditory brainstem response
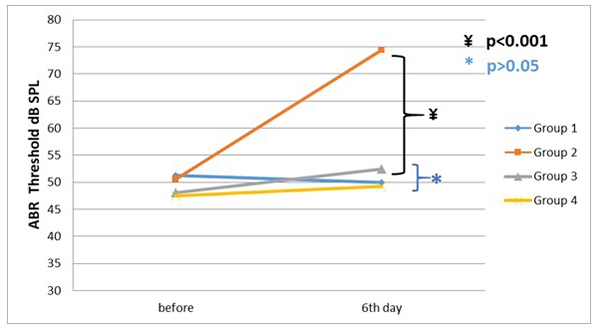
Although there was no significant difference between the groups in the initial ABR thresholds (p>0.05), the ABR thresholds in group 2 were significantly higher than in groups 1, 3, and 4 (p<0.001) on day 6. In group 2 (cisplatin), the ABR thresholds were significantly higher than the initial values (p<0.001) on day 6. In groups 1 (control), 3 (thymol+cisplatin), and 4 (thymol), no significant differences were found between the initial ABR threshold values and those obtained on day 6 (p>0.05) (Fig. 2).
 Büyütmek İçin Tıklayın |
Figure 2: Variations in auditory brainstem response (ABR) threshold values in all groups at before and after treatment on day 6. For the com¬parison between groups, the one-way analysis of variance test was used (P<0.05 was accepted as statistically significant). Tukey HSD significant difference was administrated as post hoc test to identify within-group differences (P<0.008 was accepted as statistically significant). |
Biochemical parameters
The TOS and OSI values were significantly higher in group 2 compared to the other groups (p<0.001). No significant differences were observed between the TOS and OSI values of groups 1, 3 , and 4 (p>0.05) (Table 1).
Table 1: Biochemical parameters
The TAS value was significantly higher in groups 3 and 4 than in group 2 (p=0.001) (Table 1).
Histopathological analysis
Some cochleas were lost as a result of fracture during preparation (three specimens from group 1, one from group 2, and two from each of groups 3 and 4).
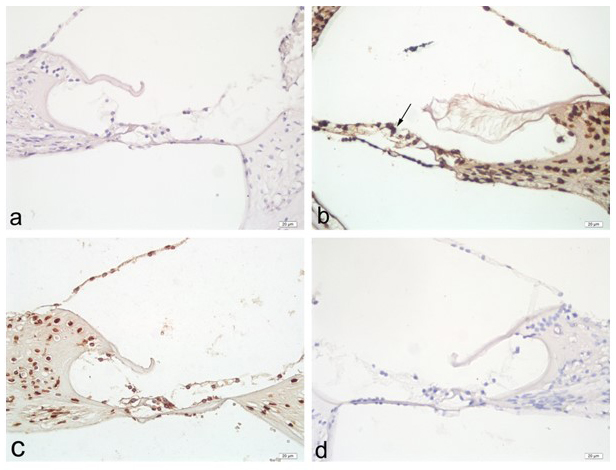
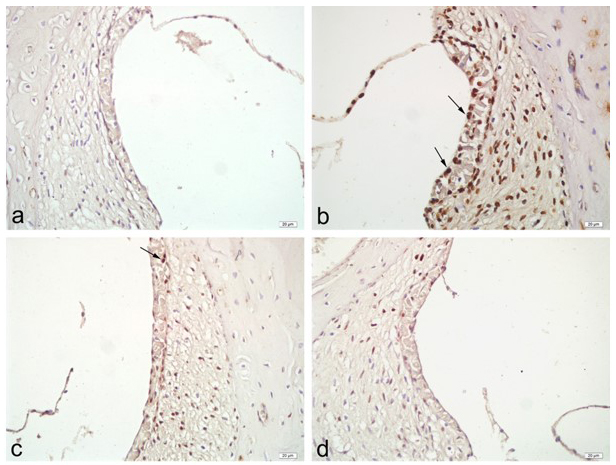
The numbers of TUNEL-positive cells are presented in Table 2. The number of such cells was higher in groups 2 than in the other groups (p<0.001) and was significantly decreased in group 3 (thymol+cisplatin), compared to group 2 (cisplatin) (p<0.05) (figs. 3,4).
 Büyütmek İçin Tıklayın |
Figure 3: Histological micrographs of organ of Corti in the cochlear sections of study groups. a: Control group. b: Cisplatin group. c: Thymol-Cisplatin group. d: Thymol group. Arrows indicate TUNEL-positive cells. Rats in group 2 showed increased TUNEL-positive cells compared to group 1, 3 and 4. Fewer TUNEL-positive cells compared to group 2 was observed in group 3. (TUNEL staining method, Bar: 20 µm). |
 Büyütmek İçin Tıklayın |
Figure 4: Histological micrographs of stria vascularis in the cochlear sections of study groups. a: Control group. b: Cisplatin group. c: Thymol-Cisplatin group. d: Thymol group. Rats in cisplatin group displayed notable TUNEL-positive cells (arrow, b) in the irregular organ of corti. In Thymol-Cisplatin group fewer TUNEL-positive cells was observed compared to cisplatin group. (TUNEL staining method, Bar: 20 µm). |
Discussion
Cisplatin is a chemotherapeutic agent that is widely used in the treatment of several cancers. Unfortunately, it produces serious adverse effects, including nephrotoxicity, neurotoxicity, and ototoxicity. Ototoxicity is bilateral, permanent, and sensorineural, and while it initially affects only high frequencies, eventually low frequencies are also affected. Cisplatin primarily destroys the cochlea, particularly the OHCs, from the base to the apex. DPOAE and ABR testing are objective methods for examining the OHCs and the auditory pathways, from proximal to distal. In the present study, DPOAE responses were significantly decreased and ABR thresholds increased in group 2 (cisplatin) on day 6, compared to the initial values obtained. Our findings are in accordance with those of previous studies. We found that DPOAE responses and ABR thresholds were preserved in group 3 (thymol+cisplatin) compared with group 2 (cisplatin) (Figs. 1, 2). Overall, our results showed that treatment with thymol may play a protective role against cisplatin-induced ototoxicity.The cellular and molecular mechanisms of cisplatin ototoxicity are not yet fully understood. However, previous studies have shown that the mechanism underlying the pathogenesis of ototoxicity may be oxidative stress. Cisplatin results in an excessive production of free oxygen radicals in the organ of Corti, the stria vascularis, the spiral ligament, and spiral ganglionic cells, leading to oxidative damage to the cochlea and OHCs, causing apoptosis[4,5]. Cisplatin reduces the level of antioxidant enzymes, via the excessive production of free oxygen radicals. Once the stability between free oxygen radical production and antioxidative defense mechanisms is impaired, oxidative stress can occur, which can result in cochlea cell injury or death[8]. It is well established that cisplatin treatment can lead to a decrease in antioxidant enzymes (such as TAS), and an increase in the level of oxidative stress products (such as TOS and OSI)[29,30]. In accordance with previous studies, we found that TOS and OSI levels were significantly higher in group 2 (cisplatin) than in the other groups, which shows that cisplatin increases oxidative stress by increasing free oxygen radicals (Table 1).
Thymol has significant antimicrobial, anti-inflammatory, and antioxidant effects, protecting the liver, erythrocytes, and kidneys from oxidative stress[12-17]. This protection against oxidative stress is related to its being an antioxidant, thereby scavenging free oxygen radicals and preventing lipid peroxidation[14,18-20]. In addition, previous experimental animal studies have shown that thymol might be protective against cisplatin-induced nephrotoxicity[15,16]. It also increases the level of antioxidant enzymes, such as glutathione and superoxide dismutase[16]. In the present study, the TAS values of groups 3 (cisplatin+ thymol) and 4 (thymol) were significantly higher than those of group 2 (cisplatin) (Table 1). This indicates the antioxidant effect of thymol against the oxidative stress caused by cisplatin.
Apoptosis, a type of controlled cell death, also plays an important role in cisplatin-induced ototoxicity. Previous studies have shown that apoptosis occurs in cochlea hair cells following administration of cisplatin,[31,32]. TUNEL is accepted as a marker of apoptosis, and TUNEL-positive staining indicates nuclear degeneration and apoptosis. In the present study, TUNEL staining revealed apoptosis in the organ of Corti and stria vascularis; the number of apoptotic cells was significantly higher in the cisplatin group than in the other groups. Further, there was a significant reduction of the number of TUNEL-positive cells in the thymol+cisplatin group compared to the cisplatin group (Figs. 3,4). These findings reflect the fact that thymol inhibited apoptosis in cisplatin-induced ototoxicity.
Another mechanism proposed for cisplatin ototoxicity is the activation of the pathways for mitogen-activated protein kinase (MAPK) and nuclear factor-κB (NF- κB). MAPK and NF-kB are important components of the signal transduction pathways that are involved in proinflammatory cytokine production. The activation of the MAPK and NF-κB pathways results in the expression of proinflammatory cytokines (such as tumor necrosis factor [TNF]-α and interleukin [IL]-6), which have been reported to play a critical role in cisplatin-induced ototoxicity[33]. In a study conducted in mice, it was shown that thymol reduces the cycle of proinflammatory cytokines (such as TNF-α and IL6) by inhibiting the MAPK and NF-κB signaling pathways[34]. These data are also evidence of the protective effect of thymol against cisplatin ototoxicity.
The strengths of the present study are the use of DPOAE and ABR tests in the total audiological evaluation, the use of biochemical parameters in the assessment of oxidative stress, and the histopathologic examination. A limitation is the fact that the effect of thymol on the antitumoral activity of cisplatin is not known. However, it has been shown that thymol has a therapeutic effect in several types of cancer[22-26]. Although the antitumoral activity of thymol has been shown in previous studies, further investigations are required to evaluate the effect of thymol on the antitumoral activity of cisplatin.
We only made one audiological control measurement after drug administration. Therefore, an absence of repetition of the measurements is another limitation of this study. In addition, although statistically sufficient, the small number of animals in each group is a limitation.
Conclusion
In conclusion, no drug for the prevention of cisplatin-induced ototoxicity is currently in clinical use. The present study showed that thymol could prevent cisplatin ototoxicity by increasing antioxidant enzymes and reducing oxidant parameters. However, it must be remembered that this was an experimental animal study; before thymol can be considered for routine clinical use, the relevant beneficial effects must be confirmed in large, prospective, randomized studies.No conflict of interest was declared by the authors.
Funding
This study was not funded.
Reference
1) Kuhlmann MK, Burkhardt G, Kohler H. Insights into potential cellular mechanisms of cisplatin nephrotoxicity and their clinical application. Nephrol Dial Transplant. 1997;12(12):24782480
2) K. Muraki, R. Koyama, Y. Honma, S. Yagishita, T. Shukuya, R. Ohashi, F. Takahashi, K. Kido, S. Iwakami, S. Sasaki, A. Iwase, K. Takahashi, Hydration with magnesium and mannitol without furosemide prevents the nephrotoxicity induced by cisplatin and pemetrexed in patients with advanced non-small cell lung cancer, J. Thorac. Dis. 4 (2012) 562568.
3) Nagy JL, Adelstein DJ, Newman CW, Rybicki LA, Rice TW, Lavertu P (1999) Cisplatin ototoxicity: the importance of baseline audiometry. Am J Clin Oncol 28:305308
4) Laurell G, Bagger-Sjoback D (1991) Dose-dependent inner ear changes after I.V. administration of cisplatin. J Otolaryngol 20:158167
5) Yumusakhuylu AC, Yazici M, Sari M, Binnetoglu A, Kosemihal E, Akdas F, Sirvanci S, Yuksel M, Uneri C, Tutkun A (2012) Protective role of resveratrol against cisplatin induced ototoxicity in guinea pigs. Int J Pediatr Otorhinolaryngol 76:404408
6) Mendonca LM, da Silva Machado C, Teixeira CC, et al. Curcumin reduces cisplatin-induced neurotoxicity in NGF-differentiated PC12 cells. Neurotoxicology 2013;34:205211
7) Ozkul Y, Songu M, Basoglu MS, et al. Evaluation of the protective effect of a-lipoic acid on cisplatin ototoxicity using distortion-product otoacoustic emission measurements: an experimental animal study. J Craniofac Surg 2014;25:15151518
8) M. Sagit, F. Korkmaz, A. Akcadag, M.A. Somdas, Protective effect of thymoquinone against cisplatin-induced ototoxicity, Eur. Arch. Otorhinolaryngol. 270 (2013) 2231e2237
9) Huang X, Whitworth CA, Rybak LP (2007) Ginkgo biloba extract (EGb 761) protects against cisplatin-induced ototoxicity in rats. Otol Neurotol 28:828833
10) Burt, S., 2004. Essential oils: their antibacterial properties and potential applications in foodsa review. Int. J. Food Microbiol. 94, 223253.
11) Bauer, K., Garbe, D., and Surburg, H. 1997. Common fragrance and flavor materials: preparation, properties and uses, 3rd ed. Weinheim, Germany: Wiley-VCH.
12) Cosentino, S.; Tuberoso, C.; Pisano, B.; Satta, M.; Mascia, V.; Arzedi, E.; Palmas, F. In vitro antimicrobial activity and chemical composition of Sardinian Thymus essential oils. Lett. Appl. Microbiol. 1999, 29 (2), 130−135.
13) Braga PC, Dal Sasso M, Culici M, Bianchi T, Bordoni L, Marabini L. Anti-inflammatory activity of thymol: Inhibitory effect on the release of human neutrophil elastase. Pharmacology. 2006;77(3):130136.
14) Alam K, Nagi MN, Badary OA, Al-Shabanah OA, Al-Rikabi AC, Al-Bekairi AM. The protective action of thymol against carbon tetrachloride hepatotoxicity in mice. Pharmacol Res. 1999; 40(2):159163.
15) Hosseinimehr SJ, Asadian R, Naghshvar F, Azizi S, Jafarinejad M, Noaparast Z, Abedi SM, Hosseini SA. Protective effects of thymol against nephrotoxicity induced by cisplatin with using 99mTc-DMSA in mice. Ren Fail. 2015 Mar;37(2):280-4 [ Özet ]
16) El-Sayed EM, Abd-Allah AR, Mansour AM. Thymol and Carvacrol Prevent Cisplatin-Induced Nephrotoxicity by Abrogation of Oxidative Stress, Inflammation, and Apoptosis in Rats. J Biochem Mol Toxicol. 2015 Apr;29(4):165-72. [ Özet ]
17) H. Mahmud, D. Mauro, M. Foller, F. Lang, Inhibitory effect of thymol on suicidal erythrocyte death, Cell. Physiol. Biochem. 24 (2009) 407414. [ Özet ]
18) Meeran MF, Prince PS. Protective effects of thymol on altered plasma lipid peroxidation and nonenzymatic antioxidants in isoproterenol-induced myocardial infarcted rats. J Biochem Mol Toxicol 2012;26(9):368373.
19) Loziene, K., Venskutonis, P.R., Sipailiene, A., and Labokas, J. 2007. Radical scavenging and antibacterial properties of the extracts from different Thymus pulegioides L. chemotypes. Food Chem. 103(2): 546559.
20) Aeschbach, R.; Loliger, J.; Scott, B. C.; Murcia, A.; Butler, J.; Halliwell, B.; Aruoma, O. I. Antioxidant actions of thymol, carvacrol, 6- gingerol, zingerone and hydroxytyrosol. Food Chem. Toxicol. 1994, 32 (1), 31−36. [ Özet ]
21) P.R. Archana, B. Nageshwar Rao, Mamatha Ballal, B.S. Satish Rao, Thymol, a naturally occurring monocyclic dietary phenolic compound protects Chinese hamster lung fibroblasts from radiation-induced cytotoxicity, Mutat. Res. 680 (2009) 7077.
22) P.C. Braga, M. Dal Sasso, M. Culici, L.Galastri, M.T. Marceca, E.E. Guffanti, Antioxidant potential of thymol determined by chemiluminescence inhibition in human neutrophils and cell-free systems, Pharmacology 76 (2006) 6168.
23) A.Jaafari, H.A. Mouse, E.M. Rakib, L.A. Mbarek, M. Tilaoui, C. Benbakhta, A. Boulli, A. Abbad, A.Zyad, Chemical composition and antitumor activity of different wild varieties of Moroccan thyme, Braz. J. Pharmacogn 17 (2007) 477491.
24) Kang SH, Kim YS, Kim EK, Hwang JW, Jeong JH. Anticancer Effect of Thymol on AGS Human Gastric Carcinoma Cells. J Microbiol Biotechnol. 2016 Jan;26(1):28-37
25) Deb, D.D., Parimala, G., Saravana Devi, S. and Chakraborty, T. Effect of thymol on peripheral blood mononuclear cell PBMC and acute promyelotic cancer cell line HL-60. Chem. Biol. Interact. 193: 97-106, 2011.
26) Chang, H.T., Hsu, S.S., Chou, C.T., Cheng, J.S., Wang, J.L., Lin, K.L., Fang, Y.C., Chen, W.C., Chien, J.M., Lu, T., Pan, C.C., Cheng, H.H., Huang, J.K., Kuo, C.C., Chai, K.L. and Jan, C.R. Effect of thymol on Ca2+ homeostasis and viability in MG63 human osteosarcoma cells. Pharmacology 88: 201-212, 2011
27) Erel O. A novel automated direct measurement method for total an¬tioxidant capacity using a new generation, more stable ABTS radical cation. Clin Biochem. 2004 Apr;37(4):277-85. [ Özet ]
28) Erel O. A new automated colorimetric method for measuring total oxidant status. Clin Biochem. 2005 Dec;38(12):1103-11. [ Özet ]
29) Toplu Y, Parlakpinar H, Sapmaz E, Karatas E, Polat A, Kizilay A. The protective role of molsidomine on the Cisplatin-induced ototoxicity. Indian J Otolaryngol Head Neck Surg. 2014 Sep;66(3):314-9. [ Özet ]
30) Kelle I, Akkoc H, Tunik S, Nergiz Y, Erdinc M, Erdinc L. Protective effects of ethyl pyruvate in cisplatin-induced nephrotoxicity. Biotechnol Biotechnol Equip. 2014 Jul 4;28(4):674-680.
31) M.R. De Freitas, A.A. Figueiredo, G.A. Brito, R.F. Leitao, J.V. Carvalho Junior, R.M. Gomes Junior, A. Ribeiro, The role of apoptosis in cisplatin-induced ototoxicity in rats, Braz. J. Otorhinolaryngol. 75 (2009) 745e752.
32) Soyalıç H, Gevrek F, Koç S, Avcu M, Metin M. Intraperitoneal curcumin and vitamin E combination for the treatment of cisplatin-induced ototoxicity in rats. Int J Pediatr Otorhinolaryngol. 2016 Oct;89:173-8 [ Özet ]
33) So H, Kim H, Lee JH, Park C, Kim Y. Cisplatin cytotoxicity of auditory cells requires secretions of proinflammatory cytokines via activation of ERK and NF-kappaB. J Assoc Res Otolaryngol. 2007 Sep;8(3):338-55 [ Özet ]
34) Dejie Liang, Fengyang Li, Yunhe Fu, Yongguo Cao. Thymol Inhibits LPS-Stimulated Inflammatory Response via Down-Regulation of NF-κB and MAPK Signaling Pathways in Mouse Mammary Epithelial Cells. Inflammation. 2014 Feb;37(1):214-22 [ Özet ]




