INVESTIGATION OF THE EFFECT OF STRONTIUM ON THE RECOVERY OF EXPERIMENTAL SUBCONDYLAR MANDIBULAR FRACTURES BY USING A SPONGOSTAN AS A CARRIER
2Cumhuriyet üniversitesi, Eczacilik, Sivas, Turkey
3Cumhuriyet üniversitesi, Patoloji, Sivas, Turkey
4Cumhuriyet üniversitesi, Dermatoloji, Sivas, Turkey
Summary
Background: We aimed to investigate whether or not we achieved a bone recovery similar to or better than positive results we obtained in single dose local administration of strontium into fracture line we made previously by using spongostan as strontium carrier.Material and Methods: The study was conducted with 24 male Wistar-albino rats. They were randomly divided into three groups: group SC3 [receiving 3% SC-soaked spongostan ( n=8), group SC5 [receiving 5% SC-soaked spongostan (n=8); and group C [only spongostan (n=8)]. A full thickness surgical osteotomy was performed in the subcondylar area. A 0.5x0.5 cm spongostan soaked with 3% SC in group SC3 and 5% SC in group SC5 was placed in the fracture area and in group C, only spongostan was placed in fracture line.
Postoperative 21 day, the animals mandible was dissected and fractured hemimandibles were obtained for histopathological examination. The amount of the ossification was scored out of 10 for each section.
Results: There was significantly immature bone and small amount of cartilage in the group SC3, completely immature bone in the group SC5 and the group C. When the groups were compared in terms of bone healing scores, there was no statistical difference between the groups (p>0.05).
Conclusions: Because the efficiency of using strontium alone was revealed in our first study, we are of the opinion that it is required to conduct future studies in which repeating local strontium injections are tried or different carrier systems are used in order to increase the positive effect of strontium on bone recovery.
Introduction
A great majority of facial injuries are mandibular fractures. Prevalence of fractures of the mandibular condylar region is 2030% and this rate is high among all mandibular fractures[1,2].Treatment of mandibular condylar fractures is among the issues mostly discussed about maxillo-mandibular traumas. Various factors such as maximum mouth opening, movement to the left and right lateral directions, protrusion, localization of the fracture, and trend of formation of hypertrophic scar tissue play a role in the selection of the treatment method. Being administered for a long time the closed treatment has become an accepted system since it gives satisfactory results in the treatment of condylar fractures. As a result of development of fixation systems, open reduction and internal fixation have also become a preferred method[1]. Open reduction has some superiorities than closed technique such as better occlusion, anatomic fixation, and allowing for early mobilisation. However, it should be remembered that open technique has disadvantages such as postoperative infection, bleeding, facial paralysis and scars on the skin although rare[2,3]. Therefore, attention should be paid during selection of a method for the treatment of condylar and subcondylar fractures.
Strontium is an element carrying competitive properties with calcium by having its salts functioning as a second messenger in the organism. The involvement of strontium in bone mineral phase is its most important similarity with calcium. The positive effect of strontium on the bone construction has been revealed in the studies conducted on strontium in 1950[4]. In systemic application, the positive effect of strontium on bone recovery is in question by both increasing the osteoblastic activity and decreasing the osteoclastic activity.[5]. Such effects of strontium on the bone metabolism have drawn the attention of numerous researchers and many studies have been conducted regarding both its local and systemic usages[6-11]. The presence of positive effects on the peri-implant bone formation have directed the researchers to develop various methods for local administrations of strontium[12-16]. We are of the opinion that local administration of strontium in the fracture line in the patients with subcondylar mandibular fractures will accelerate the bone recovery and shorten the external fixation period; may cause a reduction in the prevalence of complications that are frequently observed in closed technique and as a result may cause an enhancement in the life qualities of the patients. From this point of view, we aimed to find an answer for the Can single dose local administration of strontium shorten the external fixation period in subcondylar mandibular fractures?' question with our previously planned study. The results obtained in this study showed us that bone recovery scores were statistically higher in the rats to which single dose 3% strontium was administered than the rats in the control group to which no administration was done; the presence of the rats showing mature (lamellar) bone formation was remarkable although there was no statistically significant difference between the group to which 5% strontium was administered and the control group in terms of the bone recovery scores[17].
Gelatin sponge (SURGİSPON; AEGIS LIFESCIENCES, Wellkang Ltd. London) is a common haemostatic agent but it does not have any positive effect on bone regeneration while it is used alone[18]. There are a limited number of studies examining its capacity to locally deliver bone growth factors[19].
In this study, we aimed to investigate whether or not we achieved a bone recovery similar to or better than positive results we obtained in single dose local administration of strontium into fracture line we made previously by using spongostan as strontium carrier.
Methods
Experimental animalsThe experiments were carried out based on the National Institute of Health (NIH) Guide for the care and use of Laboratory Animals (NIH Publications No. 80-23 Revised 1996). Approval of the Institutional Review and Animal Ethics Use Committee of Cumhuriyet University School of Medicine was obtained for the study protocol and the study was conducted based on accepted guidelines for the care and use of laboratory animals.
The randomized experimental protocol was used in the study. The study was conducted with 24 male Wistar-albino rats which were 16-18 weeks old and had an average body weight of 230±10 g. These rats (n=24) were randomly divided into three groups: group SC3 [receiving 3% SC-soaked spongostan (0.3 cc, n=8)], group SC5 [receiving 5% SC-soaked spongostan (0.3 cc, n=8)]; and group C [Control group, only spongostan (n=8)].
The rats were kept under standard laboratory conditions (12 h light/dark cycles, 24±2 °C, 35-60% humidity). Since all the animals had the broken jaws, they were fed by only soft food and water for the first 7 days of experiment. They started to eat their normal diets (a standard laboratory diet and available drinking water) following the first week.
Chemicals and materials
Strontium chloride (SC) was supplied from Sigma Chemical Co. (St. Louis, MO, USA). This reagent was dissolved in saline and the purity of all chemical reagents had at least analytical grade. Spongostan (SURGİSPON) was supplied from AEGIS LIFESCIENCES, Wellkang Ltd. (London).
Operation procedure and the study protocol
The aseptic procedure was used under general anaesthesia. The rats were anesthetized with intraperitoneal injections of ketamine (7.5mg/kg)(Ketalar®, Pfizer, Turkey) and xylazine 6 mg/kg IM (Rompun®, Bayer, Turkey). Their right buccal area was shaved and prepared with an antiseptic solution (povidone iodine). Following an approximately 10 mm incision made along the inferior border of the mandible and division of the masseter muscle, a full thickness surgical osteotomy was performed by using mosquito forceps in the subcondylar area. This was confirmed by condyle fragment mobility. Hemostasis occurred both on the fracture line and connected soft tissues. A 0.5x0.5 cm spongostan soaked with 3% SC (0.3 cc, n=8) in group SC3 and 5% SC (0.3 cc,n=8) in group SC5 was placed in the fracture area and in group C, only spongostan was placed and then the incision area was sutured.
All rats were administered with intramuscular penicillin injections for the postoperative first 3 days.
After postoperative 21 day, the animals were euthanatized by using Pentothal sodium 200-mg/kg intraperitoneal injections. Their mandible was dissected and all soft tissues were removed after sacrification. Then, fractured hemimandibles were obtained for histopathological examination.
Histopathological examination:
The histological analyses were performed by two (HO, ET) pathologists who were blind to the samples. All tissue samples were immediately fixed in 10% formalin. After fixation procedure, the samples were kept at 10% nitric acid, decalcification was completed in 4 days, and the samples were embedded in paraffin. The samples were cut in the sagittal sections into 5-µm thick sections, transferred to slides for conventional hematoxylin-eosin (H&E) staining and examined by using light microscopy (Nikon, Eclipse 80İ, Japan). Digital images of the sections were obtained by using digital camera and auxiliary equipment (Nikon USB (H) EXT 1/0 Japan) with microscope.
The amount of the ossification was scored out of 10 for each section as described by Huo and Troiano[20] (Table 1). Total score of the grading scale ranged from one point (Fibrous tissue) to 10 points (Mature bone).
Table 1: Histological scoring system for the evaluation of fracture healing
Statistical analysis
The Statistical Package of Social Science (SPSS Inc., Chicago, IL) for Windows version 22.0 was used to analyse the data. Sections of all samples stained with hematoxylin-eosin were scored. Mean scores of both groups were calculated and the difference between the groups was analysed statistically. The data were expressed as mean, median, and minimum-maximum. Firstly, all of the group differences were analysed by using the Kruskal-Wallis test. It was used to examine the reason of the difference (p<0.05) determined by using the Mann-Whitney U test.
Table 2: Histological scores of fracture healing for both groups
Results
Twenty-four rats were included in this study. And the administration was well tolerated by all the rats and there was no significant weight lost until the day of sacrificing.The mean bone recovery scores of the 3%-strontium applied group was 7.25±0.46; the control group 8.00±1.31 and the 5% strontium-applied group 8.00±1.07. The mean bone recovery scores of the control and %5 strontium-applied group showed similarity. They were higher than the 3%-strontium applied group. Even though they were not different statistically (P>0.005)
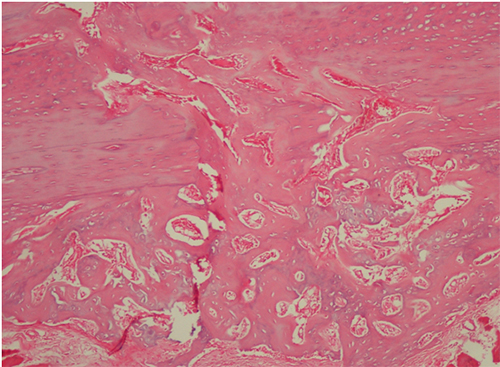
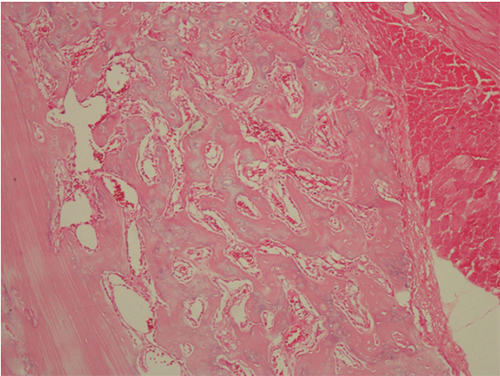
There was significantly immature bone and small amount of cartilage in the group SC3, with a median score of 7 (range 7-8) (Figure 1); completely immature (woven) bone in the group SC5, with a median healing score of 8 (range 7-10) and, completely immature (woven) bone in the group C, with a median healing score of 8 (range 6-10) (Figure 2). When the groups were compared in terms of bone healing scores, there was no statistical difference between the groups (p>0.05).
 Büyütmek İçin Tıklayın |
Figure 1: Histological section of the group SC3 significantly immature (woven) bone and small amount of cartilage formation in group SC3, score 7 (HE; X100). |
 Büyütmek İçin Tıklayın |
Figure 2: Histological section of the group SC5 and group C; completely immature (woven) bone formation in the group SC5 and group C, score 8 (HE; X200). |
Discussion
This study was conducted to examine the effect of a spongostan soaked with 3% and %5 SC on bone healing and the histologic characteristics of the new bone induced by these administrations. The results of the present study indicated that the controls and the group SC3 and SC5 rats did not show any statistically significant difference in terms of bone healing scores.The management of mandibular condylar fractures is variable throughout the literatures[21]. Some surgeons adopted a more aggressive surgical method by open reduction and internal fixation of condylar fractures [22]. However, some doctors prefer the treatment via closed technique due to the complex anatomic structure of this area, rarely seen surgical complications and scar formation. It should be remembered that treatment administered by closed technique may have serious complications such as chin deviation, trismus, malocclusion, prolonged physiotherapy, internal maxillary fixation, facial asymmetry, occlusal disturbance, chewing problems, the possible subsequent revision surgeries and temporomandibular joint discomforts[23,24]. Thus, there has been no common consensus in the treatment of condylar and subcondylar mandibular fractures, yet. The most important complication of the closed technique is the occurrence of ankylosis in the temporomandibular joint via 6-week arch-bar application in addition to reducing the life quality of the patient. In order to prevent this, various methods, that may reduce the fixation period, have been still tried. One of the studies conducted in this subject is the study of Carter et al.,[25]. In this study, they used a spongostane-soaked recombinant human bone morphogenetic protein-2 (rhBMP-2) as an alternative to the autogenous bone graft in a series including five cases with wide mandibular defects. In accordance with the results obtained from their study, they revealed that mandibular bone defects can be successfully reconstructed with rhBMP-2 soaked spongostans. Similarly, another study conducted to accelerate the recovery period is the study of Donneys et al.,[26]. In their study, they used deferoxamine as an angiogenic activator for accelerating the recovery period in the rats to which mandibular osteotomy was administered and revealed that local deferoxamine injection may accelerate bone recovery.
In the literature, there are studies conducted by using various medical agents with different carrier systems in order to reduce the recovery period of bone fractures. In these studies, both the effects of medical agents and the suitability of the carrier systems are examined. For this reason, one of the frequently used carrier systems is absorbable collagen spongostan. Because we revealed in our previous study that local 3% strontium chloride administration may have a positive effect on the recovery period of mandibular fractures, we used spongostan as a carrier system in the present study[17]. In the literature, there are studies indicating that spongostan may have both positive and negative effects on bone recovery. In their study, Sarban et al.,[27] examined the effect of absorbable collagen sponges containing recombinant human bone morphogenetic protein-2 on the recovery of osteoporotic bone fractures. They placed only absorbable collagen spongostan in fracture region in half of the rats included in the study and recombinant human bone morphogenetic protein-2 soaked spongostan to the remaining half. The results obtained revealed that bone recovery in the cases in which recombinant human bone morphogenetic protein-2 soaked spongostan was placed was better and quicker. Seo et al.'s[28] study revealed that the gelatin/β-tricalcium phosphate sponge with mesenchymal stem cells and bone morphogenetic protein-2 increased bone regeneration in an equine bone defect model.
On the other hand, in the study of Jeon et al.,[29], it was remarked that absorbable collagen sponge was not a suitable carrier system for bone morphogenetic protein-2. In the study of Hertzberg et al.,[30] they examined the effect of desferoxamine on bone recovery by using three different carrier agents and showed that calcium sulphate pellets can be a more efficient carrier despite that both collagen sponges and demineralized bone matrix increased angiogenesis more than the control group.
As understood from the above mentioned studies, there is no common consensus about these systems used for carrying drugs in the literature. In the present study, while the mean bone recovery scores of the control group and the 5% strontium-applied group showed similarity (8.00±1.31 and 8.00±1.07, respectively) they were higher than the 3%-strontium applied group (7.25±0.46) even though they were not different statistically. In our opinion, the reason behind why these results of this study both conflict with our first study and do not support our hypothesis is that spongostan is not a suitable carrier system for strontium. As remarked in the study of Hertzberg et al.,[30], when different carrier systems are used in such studies, the efficiency of the drug tested also varies. The weak point of the present study in this regard was that it was planned on using only one carrier system.
Conclusion
The efficiency of using strontium alone was revealed in our first study[17]. The results of the present study indicated that the controls and the group SC3 and SC5 rats did not show any statistically significant difference in terms of bone healing scores. These results do not support our hypothesis. However the mean bone recovery score of the group SC5 was similar to the group C but was higher than the group SC3. This point should not be missed. So that we are of the opinion that it is required to conduct future studies in which repeating local strontium injections are tried or different carrier systems are used in order to increase the positive effect of strontium on bone recovery before the studies that will examine the local administration of strontium on human subjects.Reference
1) Çimen E, Önder ME, Cambazoğlu M, Birant E. Comparison of Different Fixation Types Used in Unilateral Mandibular Condylar Fractures: An In Vivo Study With New Biomechanical Model. J Craniofac Surg. 2016 Jun 16. [Epub ahead of print] PubMed [ Özet ]
2) Aslan C, Hoşnuter M, Baş S, Tan O, Işık D, Durgun M. Retromandibular transparotid approach to mandibular subcondylar and high ramus fractures: two-point fixation. Ulus Travma Acil Cerrahi Derg. 2016 Jan;22(1):40-5. doi: 10.5505/tjtes.2015.21774. PubMed [ Özet ]
3) Lachner J, Clanton JT, Waite PD. Open reduction and internal rigid fixation of subcondylar fractures via an intraoral approach. Oral Surg Oral Med Oral Pathol 1991;71:25761.
4) Shorr E, Carter AC. The usefulness of strontium as an adjuvant to calcium in the remineralization of the skeleton in man. Bull Hosp Jt Dis 1952;13:56e66.
5) Yang F, Yang D, Tu J, Zheng Qixin, Cai L, Wang L. Strontium enhances osteo- genic differentiation of mesenchymal stem cells and in vivo bone formation by activating wnt/catenin signaling. Stem Cells 2011; 29: 981-91.
6) Maïmoun L, Brennan TC, Badoud I, Dubois-Ferriere V, Rizzoli R, Ammann P. Strontium ranelate improves implant osseointegration. Bone 2010; 46: 1436-41.
7) Li Y, Li X, Song G, Chen K, Yin G, Hu J. Effects of strontium ranelate on osseointegration of titanium implant in osteoporotic rats. Clin Oral Implants Res 2011; 23: 1038-44.
8) Ravi ND, Balu R, Sampath Kumar TS. Strontium-substituted calcium deficient hydroxyapatite nanoparticles: synthesis, characterization, and antibacterial properties. J Am Ceram Soc 2012; 95(9): 2700-8.
9) Goel A, Rajagopal RR, Ferreira JM. Influence of strontium on structure, sintering and biodegradation behaviour of CaO-MgO-SrO-SiO2-P2O5-CaF2 glasses. Acta Biomater 2011; 7(11): 4071-80.
10) Vestermark MT, Hauge EM, Soballe K, Bechtold JE, Jakobsen T, Baas J. Strontium doping of bone graft extender. Acta Orthop 2011; 82(5): 614-21.
11) Hamdy NA. Strontium ranelate improves bone microarchitecture in osteoporosis. Rheumatology 2009; 48(iv): 9-13.
12) Fu D-L, Jiang Q-H, He F-M, Yang G-L, Liu L. Fluorescence microscopic analysis of bone osseointegration of strontium-substituted hydroxyapatite implants. J Zhejiang Univ Sci B 2012; 13: 364-71.
13) Forsgren J, Engqvist H. A novel method for local administration of strontium from implant surfaces. J Mater Sci Mater Med. 2010 May;21(5):1605-9. doi: 10.1007/s10856-010-4022-8. Epub 2010 Feb 17. PubMed [ Özet ]
14) Zhao L, Wang H, Huo K, Zhang X, Wang W, Zhang Y, et al. The osteogenic activity of strontium loaded titania nanotube arrays on titanium substrates. Biomaterials 2013; 34: 19-29.
15) Gentleman E, Fredholma YC, Jell G, Lotfibakhshaiesh N, O'Donnell MD, Hill RG, et al. The effects of strontium-substituted bioactive glasses on osteoblasts and osteoclasts in vitro. Biomaterials 2010; 31: 3949-56.
16) Park J-W, Kim Y, Jang J, Song H. Positive modulation of osteogenesis- and osteoclastogenesis-related gene expression with strontium-containing microstructured Ti implants in rabbit cancellous bone. J Biomed Mater Res A 2013; 101: 298-306.
17) Durmuş K, Turgut HN, Doğan M, Tuncer E, Özer H, Altuntaş EE, Akyol M. Histopathological Evaluation of the Effect of Locally Administered Strontium on Healing Time in Mandibular Fractures: Experimental Study (ACEM-01397-2015-02), Advances in Clinical and Experimental Medicine. 2015; İn print
18) Jazayeri MA, Nichter LS, Zhou ZY, et al. Comparison of various delivery systems for demineralized bone matrix in a rat cranial defect model. J Craniof Surg 1994; 5: 172178.
19) Kos M, Staniszewska K, Matusiewicz M, et al. Tissue reaction after implantation of Spongostan, as the carrier of xenogenic bone morphogenetic protein: experimental study. Polim Med 2003; 33: 2533.
20) Huo MH, Troiano NW The influence of ibuprofen on fracture repair: biomechanical, biochemical, histologic, and histomorphometric parameters in rats. J Orthop Res. 9:3,383390, 1991.
21) Ho SY, Liao HT, Chen CH, Chen YC, Chen YR, Chen CT. The radiographic and functional outcome of bilateral mandibular condylar head fractures: a comparison between open and closed treatment. Ann Plast Surg. 2015 May;74 Suppl 2:S93-8.doi: 10.1097/SAP.0000000000000457. PubMed [ Özet ]
22) Baker AW, McMahon J, Moos KF. Current consensus on the management of fractures of the mandibular condyle. A method by questionnaire. Int J Oral Maxillofac Surg. 1998; 27: 258266.
23) Chen CT, Feng CH, Tsay PK, et al. Functional outcomes following surgical treatment of bilateral mandibular condylar fractures. Int J Oral Maxillofac Surg. 2011; 40: 3844.
24) Singh V, Bhagol A, Dhingra R. A comparative clinical evaluation of the outcome of patients treated for bilateral fracture of the mandibular condyles. J Craniomaxillofac Surg. 2012; 40: 464466.
25) Carter TG, Brar PS, Tolas A, Beirne OR. Off-label use of recombinant human bone morphogenetic protein-2 (rhBMP-2) for reconstruction of mandibular bone defects in humans. J Oral Maxillofac Surg. 2008 Jul;66(7):1417-25. doi: 10.1016/j.joms.2008.01.058. PubMed [ Özet ]
26) Donneys A, Deshpande SS, Tchanque-Fossuo CN, Johnson KL, Blough JT, Perosky JE, Kozloff KM, Felice PA, Nelson NS, Farberg AS, Levi B, Buchman SR. Deferoxamine expedites consolidation during mandibular distraction osteogenesis. Bone. 2013 Aug;55(2):384-90. doi: 10.1016/j.bone.2013.04.005. Epub 2013 Apr 15.PubMed [ Özet ]; PubMed Central PMCID: PMC4162399.
27) Sarban S, Senkoylu A, Isikan UE, Korkusuz P, Korkusuz F. Can rhBMP-2 containing collagen sponges enhance bone repair in ovariectomized rats?: a preliminary study. Clin Orthop Relat Res. 2009 Dec;467(12):3113-20. doi:10.1007/s11999-009-1004-6. Epub 2009 Aug 4. PubMed [ Özet ] PubMed Central PMCID: PMC2772906.
28) Seo JP, Tsuzuki N, Haneda S, Yamada K, Furuoka H, Tabata Y, Sasaki N. Osteoinductivity of gelatin/β-tricalcium phosphate sponges loaded with different concentrations of mesenchymal stem cells and bone morphogenetic protein-2 in an equine bone defect model. Vet Res Commun. 2014 Mar;38(1):73-80. doi: 10.1007/s11259-013-9587-5. Epub 2014 Jan 18. PubMed [ Özet ]
29) Jeon O, Song SJ, Kang SW, Putnam AJ, Kim BS. Enhancement of ectopic bone formation by bone morphogenetic protein-2 released from a heparin-conjugated poly(L-lactic-co-glycolic acid) scaffold. Biomaterials. 2007 Jun;28(17):2763-71. Epub 2007 Mar 12. PubMed [ Özet ]
30) Hertzberg BP, Holt JB, Graff RD, Gilbert SR, Dahners LE. An evaluation of carrier agents for desferoxamine, an up-regulator of vascular endothelial growth factor. J Biomater Appl. 2013 May;27(8):1046-54. doi: 10.1177/0885328211433137. Epub 2012 Jan 19. PubMed [ Özet ]




