SMALL CELL NEUROENDOCRINE CARCINOMA OF THE NASAL CAVITY AND PARANASAL SINUSES: REPORT OF ONE CASE AND REVIEW OF THE LITERATURE
2İnönü Üniversitesi, Tıp Fakültesi, Tıbbi Onkoloji, Malatya, Turkey
3Medeniyet Üniversitesi, Tıp Fakültesi, Patoloji, İstanbul, Turkey
Summary
We reported an 85–year-old female who has a history of swelling on the left side of her face and neck. There was swelling and a red area on the anterior wall of left maxillary sinus. Moreover, her left eye pointed up and outwards and her downward eye movement was limited. Punch biopsy of the nasal tumor was performed. Histopathological diagnosis revealed a small cell neuroendocrine carcinoma of the sinonasal region. She refused operation and radiotherapy, therefore she was successfully treated with three cycles of Carboplatin and Etoposide.Introduction
Small cell neuroendocrin carcinoma (SNEC) of the sinonasal tract is a rare disease. SNEC is a distinct clinicopathologic entitiy that usually occurs in the lung, but can originate in extrapulmonary sites that accounts for 4% of all SNECs.[1] SNEC is the least prevalent type of sinonasal malignancies with neuroendocrine differentiation including esthesioneuroblastoma, undifferentiated carcinoma, and neuroendocrine carcinoma.[1,2] There are several isolated cases reported of small cell neuroendocrine carcinomas of the sinonasal tract.[1,3-10]In this report, we described a patient with nasal cavity and paranasal sinuses SNEC who was successfully treated with definitive chemotherapy. The clinical and pathologic features, including immunohistochemistry of the small cell neuroendocrine carcinoma affecting the sinonasal tract and the optimal treatment of this patient are discussed.
Case Presentation
An 85–year-old female presented with a history swelling of on the left side of face and neck in February 2009 (Figure 1). She had two months history of headache, nasal obstruction, spontaneous epistaxis, and swelling in the left side of her neck, left cheek and around the left eye. The physical examination of the patient, there was a swelling and redness on the anterior wall in the left maxillary sinus. Moreover, her left eye pointed upward and patient's downward eye movement was limited. But, the vision of patient was evaluated as normal. The endoscopic nasal examination of the patient presented a mass in the left nasal cavity. The mass was smooth and reaching to the choana. The size was approximately 3 cm x 2 cm, there were multiple lymphadenopathies on the left side of the patient's neck.
 Büyütmek İçin Tıklayın |
Figure 1: Patient's appearance before treatment |
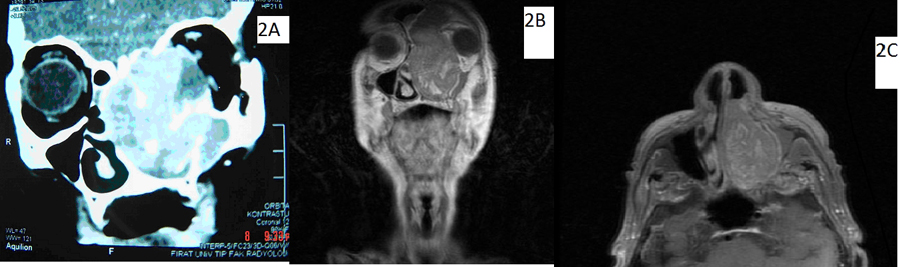
Computed tomography (CT) and magnetic resonance imaging (MRI) of the paranasal sinuses and nasopharynx on axial view revealed an expansive mass affecting the left lamina papyracea, medial orbit, ethmoid sinus, alveolar arch, and nasal cavity (Figure 2A). The coronal view demonstrated involvement of the left ethmoid, orbit, nasal cavity, and maxillary sinus with erosion thought the lateral wall of the maxillary sinus, medial orbital wall and posterior wall of the frontal sinus. The mass was in close contact with the nasal septum but not invading the midline area. The left lateral and inferior rectus muscles were infiltrated. The nasopharynx was normal (Figure 2B, 2C). Punch biopsy of the nasal tumor was performed.
 Büyütmek İçin Tıklayın |
Figure 2: Figure 2A Coronal computed tomography image showing expansive invasion of the left lamina papyracea, medial orbit, ethmoid sinus, alveolar arch, and nasal cavity. Figure 2B: Coronal magnetic resonance image showing of the left ethmoid, orbit, nasal cavity, and maxillary sinus, with erosion thought the lateral wall of the maxillary sinus, medial orbital wall and posterior wall of the frontal sinus. The mass was in close contact with the nasal septum but not invading the midline. The left lateral and inferior rectus muscles were infiltrated. Figure 2C: Axiel magnetic resonance image showing the nasopharynx was normal |
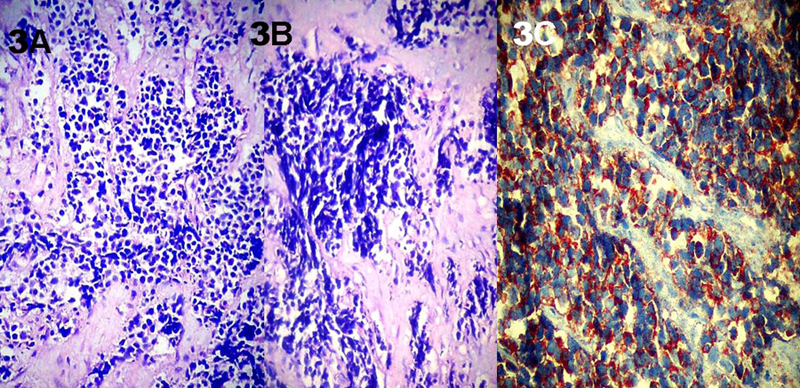
Microscopic examination (Hematoxylin-eosin–stained sections) showed nests and cords of small closely packed cells with scanty cytoplasm and indistinct cell borders. The nuclei were hyperchromatic with fine stippled chromatin and inconspicuous nucleoli (Figure 3A). Nuclear encrustation was present (Figure 3B). Several immunohistochemical stains were used, which included cytokeratin, desmin, chromogranin A, synaptophysin, LCA, CD20, S-100. All tumor cells showed diffused positivity for chromogranin A (Figure 3C), synaptophysin and cytokeratin. The tumor cells tested negative for desmin, LCA, CD20 and S-100 antibodies. The histological diagnosis was small cell neuroendocrine carcinoma of the sinonasal region.
 Büyütmek İçin Tıklayın |
Figure 3: Figure 3A Hematoxylin-eosin–stained sections showed nests and cords of small closely packed cells with scanty cytoplasm and indistinct cell borders (H-E X100). Figure 3B: Nuclear encrustation was present (H-E X100). Figure 3C: All tumor cells showed positive for diffused chromogranin A (Chromogranin A X 400). |
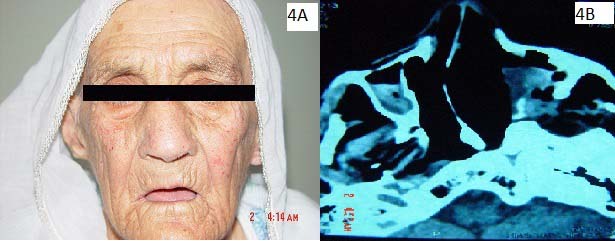
The informed consent was obtained from the patient, and left total maxillectomy and left orbital exentration was suggested to the patient as surgical procedure. But the patient refused surgery and radiotherapy, and therefore she was treated with combination chemotherapy using carboplatin and etoposide for 6 months after the diagnosis. The chemotherapy regimen consisted of 300 mg/m2 carboplatin and 120mg/m2 etoposide per day on for 3 consecutive days. After three cycles of intravenously chemotherapy the patient again had paranasal sinus CT scan to determine effectiveness of response. The mass had changed little (Figure 4A, 4B). She had no distant metastases on 58 months after the treatment.
 Büyütmek İçin Tıklayın |
Figure 4: Figure 4A Post treatment image of the patient's face Figure 4B. Post treatment axial computed tomographic image. |
Discussion
Primary small cell neuroendocrine carcinomas (SNEC) of the nasal cavity and paranasal sinuses are rare.[2,3,5,7,8] Small cell neuroendocrine carcinomas of the sinonasal tract are extremely uncommon tumors.[3] It was initially reported as a differentiated histological entity in the paranasal region by Raychowdhuri in 1965.[10] One hundred and five patients with this aggressive neoplasm of sinonasal region have been reported, both in small and in isolated case reports.[1,3-10]The clinical features of SNEC are nonspecific and are similar to those of other sinonasal tumors. The most common symptoms have been epistaxis, followed by pain, exophthalmos, and nasal obstruction. The nasal cavity has been the most commonly affected site, followed by the ethmoid and maxillary sinuses.[8,9] Our patient had 2 months history of headache, nasal obstruction, spontaneous epistaxis, and swelling in the left side neck, cheek, and around the left eye.
Microscopically, SNECs arising in the head and neck are indistinguishable from those of bronchogenic origin. Typically there are sheets, cords, and ribbons of small cells with little or no cytoplasm, which appear undifferentiated by light microscopy. Light microscopic and immunohistochemically findings of our patients were similar to current literature reports. Small cell non-neuroendocrine lesions of the sinonasal tract, which include malignant melanoma, non-Hodgkin's lymphoma, Ewing sarcoma, and rhabdomyosarcoma, can be excluded based on their morphological features and their immunoreactivity for S-100, HMB-45, lymphoid markers, vimentin, O13, actin, and desmin. Small cell neuroendocrine carcinoma should also be distinguished from other sinonasal neuroendocrine lesions, including sinonasal undifferentiated carcinoma, carcinoid tumor, pituitary adenoma, and paraganglioma. The combined histopathologic, immunohistochemical, and ultrastructural features of these lesions are different from those of SNEC.[3,8] Together with our patients, we looked at several immunohistochemical parameters (cytokeratin, desmin, chromogranin A, synaptophysin, LCA, CD20, S-100) using differential diagnosis with biopsy.
Small cell carcinoma is a highly aggressive neoplasm; extrapulmonary small cell carcinoma is usually a fatal disease with an expected 13%, 5-year survival rate.[4] Galanis et al[4] reported the median survival of 14 patients with extrapulmonary small cell carcinoma of the head and neck, including 7 paranasal cases, was on average 14.5 months. However, Fitzek et al[5] reported a 74%, 5- year survival rate and 88% probability of local control in a prospective study of 19 neuroendocrine tumors of the sinonasal tract. Similarly, Silva et al[12] reported 5-and 7-year survival rates of 100% and 88%, respectively for their chort of 20 patients with SNEC.
Systemic chemotherapy combined with surgery or radiation therapy is the most common treatment modality.[3] Small cell neuroendocrin carcinoma is radiosensitive, and combinations of surgery and irradiation are likely to achieve the most favorable outcome. Neoadjuvant and concomitant chemotherapy may play a role, particularly since these tumors are considered chemosensitive. Commonly used adjuvant agents include cyclophosphamide, cisplatin, doxorubicin, vincristine, carboplatin, etoposide, and methotrexate.[3,7,8] Fitzek et al's[5] chemotherapy response data showed a 68% response rate to cisplatin and etoposide. Smith et al[11] reported that two of four patients with sinonasal carcinoma treated with surgery and chemotherapy were alive with no evidence of disease at 31 and 108 months, respectively, while the other two patients died of the their disease at 14 and 41 months. Galanis et al[4] recommended adjuvant chemotherapy with a platinum-based regimen for extrapulmonary small cell carcinoma. Our patient did not accept surgery or radiotherapy, she has only been given chemotherapy. She was treated with combination chemotherapy using carboplatin and etoposide 6 months after the diagnosis. At this time the mass had changed little.
Small cell neuroendocrine carcinoma of the nasal cavity and paranasal sinuses has a propensity for multiple local recurrences, with direct extension into the cranial base and brain. The most frequent sites for distant metastases are the lungs, liver, and bone.[6] Galanis et al[4] reported an 80% incidence of distant failure and a median time of relapse or 30 months for those patients with paranasal tumors treated with surgry alone. Our patient refused surgical excision and the follow-up 58 months after her initial treatment showed that she had no distant metastases.
In conclusion, SNEC is an uncommon aggressive neoplasm which early diagnosis and local control is important for improved prognosis. It's treatment requires an aggressive approach, including chemotherapy, radiotherapy, and surgical resection.
Reference
1) Ma AT, Lei KI. Small cell neuroendocrine carcinoma of the ethmoid sinuses presenting with generalized seizure and syndrome of inappropriate antidiuretic hormone secretion. A case report and review of literature. Am J Otolaryngol Head Neck Medici Surg 2009; 30 (1): 54–7.
2) Rosenthal DI, Barker JL Jr, El-Naggar AK, Glisson BS, Kies MS, Diaz EM Jr et al. Sinonasal malignancies with neuroendocrine differentiation. Cancer 2004;101 (11): 2567–73. [ Özet ]
3) van der Laan TP, Bij HP, van hemel BM, Wedman J, van der Laan BF, Halmos GB. The importance of multimodality therapy in the treatment of sinonasal neuroendocrine carcinoma. Eur Arch Otorhinolaryngol 2013; 270 (9): 2565-8. [ Özet ]
4) Galanis E, Frytak S, Llyod RV. Extrapulmonary small cell carcinoma. Cancer 1997; 79 (9): 1729–36. [ Özet ]
5) Fitzek MM, Thornton AF, Varvares M, Ancukiewicz M, Mcintyre J, Adams J, et al. Neuroendocrine tumors of the sinonasal tract. Results of a prospective study incorporating chemotherapy, surgry, and combined proton-photon radiotherapy. Cancer 2002; 94 (10): 2623–34. [ Özet ]
6) Gonzalez-Garcia R, Fernandez-Rodriguez T, Naval-Gias L, Rodriguez-Campo FJ, Nam-Cha SH, Diaz-Gonzalez FJ. Small cell neuroendocrine carcinoma of the sinonasal region a propose of a case. Br J Oral Maxillofac Surg 2007; 45 (8): 676–8. [ Özet ]
7) Yadav SK, Shetty. Primary small cell undifferentiated (Neuroendocrine) carcinoma of the maxillary sinus. Case Rep Dent 2014;2014:463109. [ Özet ]
8) Khan M, Nizami S, Mirrakhimov AE, Maughan B, Bishop JA, Sharfman WH. Primary small cell neuroendocrine carcinoma of paranasal sinuses. Case Rep Med 2014;2014:874719. [ Özet ]
9) Krishnamurthy A, Ravi P, Vijayalakshmi R, Majhi U. Small cell neuroendocrine carcinoma of the paranasal sinus. Natl J Maxillofac Surg 2013; 4 (1): 111-3. [ Özet ]
10) Raychowdhuri RN. Oat cell carcinoma and paranasal sinuses. J Laryngol Otol 1965; 79: 253–5. [ Özet ]
11) Smith SR, Som P, Fahmy A, Lawson W, Sacks S, Brandwein M. A clinicopathological study of sinonasal neuroendocrine carcinoma and sinonasal undifferentiated carcinoma. Laryngoscope 2000; 110 (10 pt 1): 1617–22.
12) Silva EG, Butler JJ, MacKay B, Goepfert H. Neuroblastomas and neuroendocrine carcinomas of the nasal cavity: a proposed new classification. Cancer 1982; 50 (11): 2388–405. [ Özet ]




