LONG-TERM HEARING RESULTS OF PATIENTS TREATED WITH COMBINED ORAL STEROID, INTRATYMPANIC STEROID AND HYPERBARIC OXYGEN FOR SUDDEN SENSORINEURAL HEARING LOSS
2Department of Otorhinolaryngology/Head and Neck Surgery, Fatih Sultan Mehmet Educational and Research Hospital, Istanbul, Turkey
Summary
Aim: to evaluate short and long-term hearing outcomes of the patients treated with combined intratympanic, systemic steroids and hyperbaric oxygen therapy for Idiopathic Sudden Sensorineural Hearing Loss (ISSHL).Materials and Methods: The study was a retrospective case review. The study group consisted of 125 consecutive adult patients diagnosed with ISSHL who underwent combined intratympanic steroid, systemic steroid and hyperbaric oxygen treatment between 2005 and 2011 in tertiary referral center. 500, 1000, 2000, 4000 Hz and pure tone average ( PTA) at these frequencies were used to evaluate hearing characteristics at baseline, 1 month after the end of treatment and in the long-term (mean: 3.03±1.49; range: 1-6 years). Hearing recovery rates were classified using Siegel's criteria.
Results: Complete recovery was observed in 18,4% of the patients after combined treatment and in 23,2% of the patients in the long-term. 55,2% and 49,6% of the patients had no hearing improvement either after the treatment or in the long-term. Long-term Siegel recovery rate was very significantly worse in patients with tinnitus. Patients who recovered completely in the long-term was significantly younger than those with partial, slight and no improvement.
Conclusion: Multimodal approach has no cumulative effect on the outcome of ISSHL in the long-term.
Introduction
Idiopathic Sudden Sensorineural Hearing Loss (ISSHL) is defined as the idiopathic loss of hearing of at least 30 dB over at least three contiguous frequencies occurring within 3 days[1].Numerous treatments such as systemic and intratympanic steroids, antiviral drugs, osmotic diuretics, anticoagulants, vasodilators, hyperbaric oxygen, and carbogen have been applied in the treatment of this condition. From these, oral steroids which are thought to reduce inflammation and edema in the inner ear are reported to be the preferred treatment by 98% of the otolaryngologists in U.S.A[2,3]. Based on the spontaneous recovery rate which varies from 32 to 65%, there are some who assert not to treat ISSHL regarding the long-term complications and adverse effects of systemic steroids.
With the recent knowledge of the round window being the main access to inner ear for the drugs injected into middle ear cleft, the otologists adopted ways to administer steroids into inner ear spaces, for bypassing the systemic circulation[4]. Recent studies, although with contrasting results, reported promising outcomes with intratympanic steroids in restoring the hearing[5,6]. However, the effectiveness of a specific treatment still lacks the support of scientific evidence.
Many factors like vascular occlusion, viral infections, labyrinthine membrane breaks, immune associated mechanisms abnormal stress response in the cochlea have been suggested in the etiopathogenesis of ISSHL. However, identifiable causes are found for 7% to 45% of the patients[7,8]. The uncertainty about etiology and the prediction in prognosis of this disease explains the diversity in its management.
Several scientific studies on benefits of single or combined treatment regimen for ISSHL in the short term are reported in the literature. However, there is a paucity of information about the effectiveness of these modalities on hearing outcome in the long-term.Within this context, we aimed to investigate the long-term recovery of ISSHL treated with combined systemic and intratympanic steroid and hyperbaric oxygen.
Methods
1. Study DesignThis was a retrospective cohort study comparing short and long-term hearing results of the patients who received combined systemic steroid, intratympanic steroid and hyperbaric oxygen for ISSHL. Ethics approval was obtained from the institutional local ethics committee with the study ID#HNEAH-KAEK 2012/20.
2. Patients
125 consecutive adult patients diagnosed with ISSHL after clinical, physical, audiologic examination and magnetic resonance imaging, who underwent combined intratympanic steroid, systemic steroid and hyperbaric oxygen treatment between 2005 and 2011 were included in the study.
Patients were excluded if they had a history of previous chronic otitis, ototoxic drug use, travma, fluctuating hearing loss, underlying immunologic or neoplastic disease that may cause hearing loss, a known systemic disease contraindicating the use of systemic steroids or any comorbidity that interfered with hyperbaric oxygen treatment. Patients, whose treatment started longer than 2 weeks after onset of sudden deafness were dropped out of the study.
3. Treatment Regimen
Patients were all given systemic steroid (injection of methylprednisolone 1 mg/kg/day intravenously for five days) followed by tapered doses. In addition 0.2 to 0.4 mL of intratympanic dexamethasone sodium phosphate (4 mg/mL) was injected through the tympanic membrane into the tympanic cavity every other day for a total of three times. Patients were instructed to avoid swallowing and to keep a supine position with their heads turned 45° to the opposite side for 30 minutes after injection. Hyperbaric oxygen at a pressure of 2.5 ATA for 120 minutes, once daily, was started on all patients for a total of 20 sessions.
4. Evaluation of Hearing Outcome
Pure tone average ( PTA) of 500, 1,000, 2,000 and 4,000 Hz was used to evaluate hearing characteristics at the baseline , 1 month after the end of treatment and in the long-term. The arithmetic mean of the hearing levels at these frequencies were recorded according to the considerations of minimal standard for reporting hearing loss[9].
Hearing recovery rate was classified using Siegel's criteria[10]. This is a system based on the average gain in dB in 500 Hz, 1000 Hz, 2000 Hz, and 4000 Hz evaluating the degree of hearing improvement from no improvement: less than 15 dB of gain, final hearing poorer than 75 dB; slight recovery:more than 15 dB of gain and a final hearing poorer than 45 dB; moderate recovery: more than 15 dB of gain and final hearing level between 25 and 45 dB to complete recovery: hearing level better than 25 dB regardless of the size of the gain. Posttreatment and long-term hearing recovery rates were noted and compared in regard to patients' vertigo and tinnitus symptoms and age.
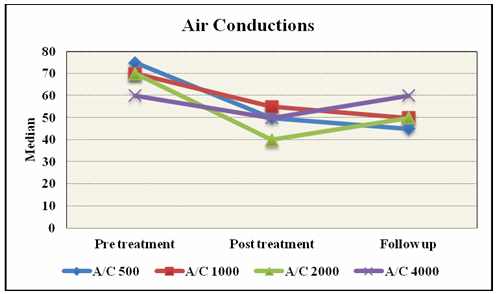
Frequency specific analyses of air and bone conduction hearing levels at the baseline, 1 month after the treatment and in the long-term were also done for observing the course of hearing levels at 500, 1000, 2000 and 4000 Hz.
5. Statistics
All the statistical analyses were performed using NCSS (Number Cruncher Statistical System) 2007&PASS (Power Analysis and Sample Size) 2008 Statistical Software (Utah, USA). Data were expressed by means of descriptive (mean, standard deviation, frequency, median, minimum, maximum) and quantitative methods. Student T test and Mann Whitney U test were used as quantitative analyses for comparison of two groups with parameters that showed normal or non-normal distribution. Kruskal Wallis Test was applied for the comparison of three or more groups with data that did not show normal distribution and Mann Whitney U for defining the group that differed from the others. Repeated measures of data that did not show a normal distribution were evaluated using Friedman Test. Wilcoxon Signed Ranks Test was used when comparing two groups with parameters with non-normal distribution.Qualitative data were compared using Pearson χ² and Yates Continuity Correction Tests as appropriate. Statistical significance was accepted at p levels <0,01 and <0.05.
Results
1. Profile of Patients125 patients (70 male, 56%; 55 female,44%) who have received combined treatment, attended the clinic for 1 month post treatment evaluation and 1 year follow-up. The age of the patients was ranging from 25 to 76 years with a mean age of about 49.40±14.03 years.
The time interval between the start of ISSHL and the long-term follow-up visit ranged from 1 to 6 years with a mean of time interval about 3.03±1.49 years.
Tinnitus was present in 62.4% (n=78) of the patients at the onset of the disease. 52% (n=65) of the patients described short lasting vertigo associated with the start of ISSHL.
2. Hearing Outcomes in the Short and Long-term
Mean PTAs (500, 1000, 2000 and 4000 Hz) of all patients at the initial diagnosis, 1 month after the end of the treatment and in the long-term were accordingly: 73.14±23.32dB; 54.24±32.35dB and 53.50±32.55dB. The differences between mean pretreatment and posttreatment PTAs and between pretreatment and long-term PTAs were very significant (p=0.001; p=0.001). However no significant difference was seen between mean posttreatment and long-term PTAs (p=0.876) [Table 1].
Hearing recovery rates were classified according to Siegel criteria [Table 2]. Complete recovery was observed in 23 (18.4 %) patients after combined treatment and in 29 (23.2%) patients in the long-term.There was an increase of about 4.8% in the percentage of patients who recovered completely on long-term. 33 (26.4%) patients in the posttreatment group and 21 (16.8%) patients in the long-term group recovered partially. There was a drop of about 9.6% in the partially recovered group.No slight improvement was seen after the treatment while 13 (10.4%) patients were in the slight improvement category in the long-term. Therefore overall improvement rates were 44.8% after treatment and 50.4% on 1 year follow-up. 69 (55.2%) and 62 (49.6%) patients had no hearing improvement either after the treatment or in the long-term. 5.6% of the patients in the no improvement group on 1month gained some hearing in the long-term [Table 2]. However,the difference between the cure rates after the treatment and in the long-term was not statistically significant (Wilcoxon Signed Ranks Test; p=0.903; p>0.05) [Table 3].
Table 2: Posttreatment and Long-term Recovery Rates of Patients According to Siegel Criteria.
Mean pre, post-treatment and long-term PTAs of the patients who recovered completely in the long-term were: 64.05dB±18.69; 24.18dB±16.08 and 13.75dB±4.42 respectively. Mean pre, posttreatment and long-term PTAs of the patients who recovered partially in the long-term were accordingly: 61.90dB±12.42; 38.69dB±9.10 and 31.73dB±4.60. The difference between long-term complete, partial, slight and no recovery groups were very significant with regard to mean baseline PTAs.Mean baseline PTAs levels of the complete and partial recovery groups were significantly better than those with slight or no improvement groups (Kruskal Wallis Test,**p<0.01;p= 0.005**;0.001**;0.001**Table 4).Patients whose recovery rate was complete and partial in the posttreatment period ,continued to have significantly better PTA levels in the long term while patients with slight improvement displayed significantly worse PTAs in the long-term than in the posttreatment period. (Wilcoxon Signed Rank test, *p <0.05;p= 0,035*; p= 0,005**; p= 0,008**) [Table 4].
Long-term Siegel hearing recovery and overall hearing improvement rates were compared according to patients' age and to the presence of vertigo and tinnitus symptoms.No statistically significant difference was seen between patients' age with regard to overall improvement (p>0,05).However, there was a very significant difference between Siegel recovery rates in the long-term with regard to patient's age (p=0.001; p<0.01). Patients who recovered completely in the long-term were very significantly younger than those with partial, slight or no improvement (Kruskal Wallis, p=0.001; p=0.006; p=0.001; p<0.01) [Table 5]. There was no significant difference between overall improvement of the patients in the long-term with regard to the presence or absence of vertigo. Although not statistically significant Siegel complete recovery rate which was found to be poorer on long-term in patients who experienced symptoms of vertigo at the start of ISSHL, was close to a level of significance (p=0.059). However, there was a very significant difference between patients' long-term overall hearing improvements with regard to tinnitus.Overall improvement rates were very significantly worse in patients with tinnitus in the long term (p<0.01).Furthermore patients with tinnitus at the start of the disease had worse improvement scores in the long-term than those without (Pearson χ², p<0.01).
Table 5: Siegel Long-term Hearing Recovery Rates according to Patient's Age, Vertigo and Tinnitus.
Frequency specific analyses of air conductions at baseline, 1 month after the treatment and on long-term were in line with PTAs results. Hearing at 500, 1000, 2000 and 4000Hz have all significantly responded to treatment in early post-treatment period. Furthermore hearing levels at 500Hz went on to improve significantly on long-term.However, there was no statistically significant difference between post-treatment and long-term mean hearing thresholds at 1000, 2000 and 4000Hz [Table 6, Fig.1]
 Büyütmek İçin Tıklayın |
Figure 1: Air Conduction Levels at 500, 1000, 2000and 4000Hz at Baseline , Post-treatment and Long-term Follow-up. |
Discussion
Despite the undetermined pathogenesis of the disease, steroids are widely accepted for the treatment of ISSHL. Eventhough their effect on the inner ear still remains unclear, they are supposed to increase labyrinthine circulation or influence the cochlear fluid homeostasis, possibly by attenuating an inflammatory process[11-13].Although the optimal dose of administration is currently unknown, higher concentrations of steroids in the cochlea have been observed to be associated with better hearing recovery in the past decades. However, regarding the serious side effects of systemic corticosteroids the possibility of direct intracochlear application of these pharmaceutic agents has been of interest recently.
Intratympanic administration of these medications was demonstrated in animal models to yield a much higher perilymphatic concentrations than intravenous use[14].
Intratympanic steroids are used in 3 different ways: as an initial treatment, as a complementary treatment to systemic steroids, or after failure of systemic steroids[15].
Early studies have demonstrated good results with transtympanic injections used concomitantly with systemic steroids, ranging from 66 to 80%[16,17].
Similar results were obtained in the randomized,double blinded, controlled study of Battaglia in 2008. 63% of the patients had complete hearing recovery, whereas 25% of the patients yielded partial recovery and 12% no hearing recovery with IT dexamethasone combined to high dose systemic steroids with tapered dose[18]. The authors notified that combination therapy had a longer therapeutic window (6 weeks), better hearing outcome with a faster recovery than systemic steroids alone.
However, studies reported on intratympanic steroid injections used in addition to systemic steroids present highly variable success results ranging from 12 to 100% and there are some who assert that the combination of IT and systemic steroids do not have additional benefits compared with systemic steroids alone in the treatment of ISSHL[19]. Likewise, regarding data extracted from the English literature there is still ongoing heterogeneity in its use as an initial, as an adjunctive or as a salvage treatment after failure of initial systemic steroids in refractory ISSHL[20].
Our study differs from previous ones in terms of treatment protocol. A combination therapy including IT steroids, systemic steroids and Hyperbaric Oxygen therapy was preferred for all patients expecting to gain better hearing outcomes. However, our success results were worse than what we have anticipated to be and were not in line with the authors who reported high success rates[16,17,18,21]. Success results did not exceed 18.4% of the patients in the complete recovery group and 44.8% in the overall improvement, in the short- term. This was even worse than the observed spontaneous recovery rate that was reported to range from 32 to 70% within two weeks after onset[21].
An explanation to our low success rate may be the possible deficiency in the glucocorticoid receptors of outer hair cells' plasma membrane of the patients that may have prevented the steroids effecting the cochlear hair cells[22].
However,despite the small ratio (18.4% ) of cases who recovered completely the difference between the overall mean pretreatment and posttreatment PTAs was very significant (p=0.001). Furthermore, when compared to studies conducted to assess the efficacy of combined systemic steroids with IT steroids or with HBO treatment; our overall improvement scores were not worse than these others[23]. In addition, the frequency specific analysis of air conductions at the baseline and in the post-treatment period demonstrated a significant response to treatment in all frequencies (Friedman Test;p<0.05).Moreover, hearing levels at 500 Hz went on to improve significantly in the long-term.
The time of commencement or time of stabilization of hearing improvement has been the focus of recent researches in the literature.However, there are ongoing debates between judgements about the follow-up period of these patients. Some experts who conducted follow-up studies for a maximum period of 6 months after treatment, emphasized the need for a follow-up longer than 2 months in cases with incomplete recovery, expecting persistent delayed improvement after treatment[24].
In line with these decisions, results drawn from a long-term follow-up of 156 patients with ISSHL have shown final hearing levels to be reached by 1 month in 78% and by 3 months in 97% of patients. The authors stated that in case of failure to complete recovery it would make sense to follow patients with sudden deafness for 3 months[25].
In contrast to the advised short –term follow-up period, there are also previous studies comprising larger size of patients treated for ISSHL ,that reported the hearing results to be the same in 44%, deteriorated in 28% and improved in 10% of the patients after a follow-up period of 8–15 years. According to their statements, the improvement was most marked at 0.5 kHz (17 dB), and at 1 kHz (16 dB)[26].
Later on, in a study in 2013, hearing levels of 44 patients were found to be very significantly better in the long-term (mean follow- up : 17.5 ± 5.7 months). Complete improvement was observed in 45.5%, partial improvement in 13.6% of the patients whose mean time from onset of symptoms to treatment start was 2,5 days[27]. Regarding this short time interval from the start of ISSHL to treatment, it remains questionable to determine whether this high complete cure rate originated from the therapeutic intervention or was it a consequence of the natural history of high spontaneous recovery rate of the disease[28].
Given the wide variance in treatment protocols , benefits and contradictions in follow-up periods in ISSHL, we intended to verify the effectiveness of a shotgun approach incorporating IT steroids, systemic steroids and HBO treatment modalities on hearing outcomes in the short and long-term. Complete cure rate which was 18.4% at post- treatment 1 month increased of about 4.8% and raised to 23.2% in the long-term. No improvement rate which was 55.2% in the posttreatment period decreased to 49.6% in the long-term. 5.6% of the patients in the no improvement group gained some hearing long-term follow-up. However,the difference between post- treatment and long-term cure rates was not statistically significant (p=0.903, Table 3). Regarding low cure rates of the present study we may not suggest that multimodal approach has cumulative effect on the outcome of ISSHL either in the post treatment or on long-term follow-up. Derived from our results we may assume that combined therapy presents no superiority over IT steroids, systemic steroids or HBO administration used as single or dual therapy in the treatment of ISSHL.
Recently pre-treatment severe and profound hearing losses have been identified as a negative prognostic indicator for hearing recovery following ISSHL[29].
Mean pretreatment hearing levels of the groups with complete, partial , slight and no recovery in the long-term were accordingly: 64.05dB±18.69 (median 61.2dB); 61.90dB±12.42 (median 52.5dB); 83.56dB±16.80 (median:83.7dB); 79.01dB±6.41 (median:75dB). Pretreatment hearing levels which were moderately severe( 56–70dB) according to the guidelines of the American Speech–Language–Hearing Association's hearing assessment (ASHA) recovered completely or partially; whereas pretreatment hearing levels which were severe (71–90dB) showed slight improvement or no improvement at all[30]. Furthermore, patients whose recovery rate was complete and partial continued to have better hearing levels in the long term while patients with slight improvement and no improvement displayed worse PTAs in the long-term than in the posttreatment period [Table 4].
Comorbid tinnitus and vertigo on presentation have been identified as indicators of a poor prognosis for ISSHL[31]. Similar to recent studies, tinnitus was a significant long-term accompanying complaint in our patients with poor prognosis. However, the presence of vertigo in our study did not reduce the chance of recovery[32]. Additionally younger age (mean: 39.41±13.80y) was found to be a factor influencing complete recovery.
Within the limitations of a retrospective analysis we aimed to present our clinical experience with a multimodal approach covering IT steroids,systemic steroids and HBO therapy for ISSHL. Except for 500 Hz we were not able to achieve significant differences between short and long-term outcomes in 1000, 2000, 4000Hz with this combined therapy.Another issue to consider was the lack of a control group treated with IT, systemic steroids or HBO alone for comparing the cumulative effects of these modalities on hearing recovery. However,hearing thresholds in 500,1000, 2000 and 4000Hz were all significantly better than baseline thresholds. We hope these results would be better strenghtened with further controlled randomized studies in future.
Conclusion
Complete recovery in ISSHL was observed in 18.4% of the patients in the post-treatment period and in 23.2% of the patients in the long-term, treated with combined IT steroids, systemic steroids and HBO treatment. Multimodal approach presented no significant effect on hearing recovery on long-term. There was an increase of about 4.8% in the percentage of patients who recovered completely in the long-term.Failure rate was 55.2% and 49.6% in the short and long-term respectively. 5.6% of the patients gained some hearing in the long-term. Patients Siegel recovery rate in the long term was very significantly worse in patients with tinnitus.Younger age (median:32.0 y) was found to be a factor influencing complete recovery on long-term. Hearing levels at 500, 1000 , 2000 and 4000Hz all significantly responded to treatment in post-treatment period. 500Hz was the only frequency that improved significantly in the long-term.Reference
1) National Institute of Health. Sudden Deafness. Bethesda, Md:National Institutes of Health; 2000. NIH publication 00-4757.
2) Shemirani, N. L., Schmidt, M., & Friedland, D. R. Sudden sensorineural hearing loss: An evaluation of treatment and management approaches by referring physicians. Otolaryngology–Head and Neck Surgery 2009; 140: 86-91.
3) Merchant, S. N., Durand, M. L., & Adams, J. C. Sudden deafness: is it viral? ORL; ORL; Journal of Oto-rhino-laryngology and its Related Specialities 2008; 70: 52-60; discussion 60-52.
4) Mattox DE, Simmons FB Natural history of sudden sensorineural hearing loss. Ann Otol Rhinol Laryngol 1977; 86:463–480
5) Dallan, I., De Vito, A., Fattori, B. et al. Intratympanic methylprednisolone in refractory sudden hearing loss: A 27-patient case series with univariate and multivariate analysis. Otology &Neurotology 2010; 31: 25-30.
6) She, W., Dai, Y., Du, X. et al. Hearing evaluation of intratympanic methyl prednisolone perfusion for refractory sudden sensorineural hearing loss. Otolaryngology–Head and Neck Surgery 2010; 142: 266-271.
7) Chau, J. K., Lin, J. R., Atashband, S., Irvine, R. A., & Westerberg, B. D. Systematic review of the evidence for the etiology of adult sudden sensorineural hearing loss. Laryngoscope 2010; 120: 1011-1021.
8) Huy, P. T., & Sauvaget, E. Idiopathic sudden sensorineural hearing loss is not an otologic emergency. Otology & Neurotology 2005; 26: 896-902.
9) Gurgel RK, Jackler RK, Dobie RA, Popelka GR. A new standardized format for reporting hearing outcome in clinical trials. Otolaryngol Head Neck Surg 2012;147:803-807.
10) Siegel LG. The treatment of idiopathic sudden sensorineural hearing loss. Otolaryngol Clin North Am 1975 ; 8:467-73.
11) Silverstein H, Choo D, Rosenberg S, Kuhn J, Seidman MD, Stein I . Intratympanic steroid treatment of inner ear disease and tinnitus (preliminary report). Ear Nose Throat J 1996; 75: 468–471
12) Shirwany NA, Seidman MD, Tang W Effect of transtympanic injection of steroids on cochlear blood flow, auditory sensitivity, and histology in the guinea pig. Am J Otol 1998;19: 230–235
13) Fukushima M, Kitahara T, Uno Y, Fuse Y, Doi K, Kubo T. Effects of intratympanic injection of steroids on changes in rat inner ear aquaporin expression. Acta Otolaryngol 2002 ;122:600–606
14) Chandrasekhar, S. S., Rubinstein, R. Y., Kwartler, J. A. et al. Dexamethasone pharmacokinetics in the inner ear: Comparison of route of administration and use of facilitating agents. Otolaryngology–Head and Neck Surgery 2000 ; 122: 521-528.
15) Seggas I, Koltsidopoulos P, Bibas A, Tzonou A, Sismanis A. Intratympanic steroid therapy for sudden hearing loss: a review of the literature. Otol Neurotol. 2011; 32:29-35. Review.
16) Gianoli G, Li J. Transtympanic steroids for treatment of sudden hearing loss. Otolaryngol Head Neck Surg 2001 ; 125:142-146.
17) Kopke R, Hoffer M, Wester D, O'leary M, Jackson R. Targeted topical steroid therapy in sudden sensorineural hearing loss. Otol Neurotol 2001; 22:475-479.
18) Battaglia A, Burchette R, Cueva R. Combination therapy (intratympanic dexamethasone + high-dose prednisone taper) for thetreatment of idiopathic sudden sensorineural hearing loss. Otol Neurotol; 2008; 29:453-460.
19) Ahn JH, Yoo MH, Yoon TH, Chung JW. Can intratympanic dexamethasone added to systemic steroids improve hearing outcome in patients with sudden deafness? Laryngoscope 2008; 118:279–282
20) Lee JB, Choi SJ, Park K, Park HY, Choo OS, Choung YH. The efficiency of intratympanic dexamthasone injection as a sequential treatment after initial systemic steroid therapy for sudden sensorineural hearing loss.Eur Arch Otorhinolaryngol. 2011; 268 :833-839.
21) Kuhn M, Heman-Ackah SE, Shaikh JA, Roehm PC. Sudden sensorineural hearing loss: a review of diagnosis,treatment, and prognosis. Trends Amplif. 2011; 15:91-105.
22) Hargunani CA1, Kempton JB, DeGagne JM, Trune DR. Intratympanic injection of dexamethasone: time course of inner ear distribution and conversion to its active form.
Otol Neurotol. 2006; 27:564-569.
23) Arslan N, Oğuz H, Demirci M et al. Combined intratympanic and systemic use of steroids for idiopathic sudden sensorineural hearing loss. Otol Neurotol. 2011; 32:393-397.
24) Moon IS, Kim J, Lee SY, Choi HS, Lee WS. How long should the sudden hearing loss patients be followed after early steroid combination therapy? EurArch Otorhinolaryngol. 2009 ; 266:1391-1395.
25) Yeo SW, Lee DH, Jun BC, Park SY, Park YS. Hearing outcome of sudden sensorineural hearing loss: long term follow up.Otolaryngol Head Neck Surg. 2007; 136:221-224.
26) Kallinen J, Laurikainen E, Bergroth L, Grénman R. A follow-up study of patients suffering from sudden sensorineural hearing loss.Acta Otolaryngol. 2001; 121:818-822.
27) Akdag M, Gul A, Bakir S et al. Long-term Follow-up Results of the Patients Suffering from Sudden Hearing Loss Int. Adv. Otol. 2013; 9: 203-210.
28) Chen CY, Halpin C, Rauch SD. Oral steroid treatment of sudden sensorineural hearing loss: a ten year retrospective analysis. Otol Neurotol. 2003; 24:728–733.
29) Nosrati-Zarenoe R, Hansson M, Hultcrantz E. Assessment of diagnostic approaches to idiopathic sudden sensorineural hearing loss and their influence on treatment and outcome. Acta Otolaryngol. 2010; 130: 384-391.
30) American Speech–Language–Hearing Association Guidelines for manual pure-tone threshold audiometry. Available from www.asha.org.http://asha.org/docs/html/GL200500014. html. 2005; Accessed July12, 2012.




