COMPARISON OF THE TYMPANOMETRY AND BINOCULAR MICROSCOPY WITH RESULTS OF MYRINGOTOMY IN THE DIAGNOSIS OF OTITIS MEDIA WITH EFFUSION IN CHILDREN
Summary
Objective: To investigate the preoperative sensitivity and specificity of binocular microscopy in the diagnosis of otitis media with effusion (OME).Methods: By reviewing the retrospective findings of preoperative tympanometry, intraoperative binocular microscopy and middle ear fluid features which was aspirated during myringotomy, we evaluated 800 ears in total in 400 children who had myringotomy in our clinic.
Results: The average age of patients was 6.28 (± 2.99) and the ages ranged between ages 1 and 17. Tympanometry sensitivity was 93.6%, specificity was 21.3%, the positive predictive value (PPV) was 73.9% and the negative predictive value (NPV) was found to be 58.1%. Binocular microscopic examination's sensitivity was identified as 94.5%, specificity as 22.6%, PPV as 74.4% and NPV as 63.1%
Conclusions: In our study we found that binocular microscopy is the most specific and sensitive diagnostic tool in the diagnosis of OME.
Introduction
Otitis media with effusion (OME), refers to the accumulation of fluid in the middle ear cavity without any signs of acute infection[1]. OME is a common health problem especially in the pediatric age groups. The etiology of these disease is multi-factorial. There are environmental risk factors like smoke exposure and attending to a daycare center[2].There are also risk factors of like; age, gender, hypertrophy of the adenoid tissue, allergy, immunologic status, cleft palate and mucocilliary dysfunction. These factors may constitute in the development of OME[2].
Many diagnostic procedures are used to detect middle ear effusion; using a simple otoscopy, pneumatic otoscopy, tympanometry and acoustic reflectometry[3]. The sensitivity and specificity of pneumatic otoscopy and tympanometry in the diagnose of middle ear effusion have been showed in the literature[4].
In confirming the otitis media with effusion, tympanometry has long played an important role, by conveying presence/absence of middle ear fluid. Most tympanometry in primary care clinics use low frequency probe tones (220–226 Hz) to classify tympanometrys as Jerger A, B, or C[5].
The purpose of this study was to investigate the preoperative sensivity and specificity of binocular microscopy in the diagnosis of OME of patients that had myringotomy (and adenoidectomy, adenotonsillectomy, tympanostomy tube insertion) by reviewing retrospective findings of preoperative tympanometry, intraoperative binocular microscopic findings and the middle ear fluid features which was aspirated after myringotomy in a 2-years period in Antalya Training and Research Hospital, Ear Nose Throat (ENT) Clinic.
Methods
The patients files that had myringotomy (andadenoidectomy, adenotonsillectomy, tympanostomy tube insertion) in Antalya Training and Research Hospital, ENT Clinic, reviewed retrospectively. All patients age, gender, allergy, smoke exposure (parents smoking), and gastroesophageal reflux symptoms and socio-demographic characteristics were recorded.Patients over the age of 17, and the patients that have insufficient file information, previous myringotomy / tympanostomy tube had applied and perforated tympanic membrane, and patients with skull-facial malformation, were exculuded from the study. The patients who have ongoing otitis media with effusion for at least 3 months constituted an indication for myringotomy (tympanostomy tube insertion)[4].
The study protocol was approved by the Ethics Committee of the Antalya Training and Research Hospital.
Audiologic evaluation
Tympanometric and pure tone audiometric (cooperative children underwent audiometric testing) were done by the same audiologist using the same audiometer and tympanometer for all children. Tympanometry was performed using the same device (Madsen Capella, GN Otometrics, USA) and the same examiner, as was pure-tone audiometry (AC-40 Clinical Audiometer, Interacoustics, Denmark). All children underwent tympanometric measurement and classified according to the classification of Jerger[6,7]. Type-A represents normal compliance of the tympanic membrane, type-B represents decreased compliance, and type-C represents negative pressure in the middle ear. The audiologist had no information about the otoscopic examination results.
Binocular microscopy
Binocular otomicroscopy (Möller Hi-R, Germany) was performed on the anaesthetised child by a specialist otolaryngologists (UO, HE), with magnification. During the operation the tympanic membrane, categorized as normal, hypervascular, dull and retracted and it was recorded to file. All patients had myringotomy to anterior-inferior portion of the tympanic membrane and recorded as middle ear fluid aspiration present / not present.
Each sample was classified as a mucoid or serous middle ear effusions (MEE) based on the gross appearance upon inspection with the naked eye. A mucoid MEE was a thick, viscoid, and mucus- like effusion that did not flow on inversion, while a serous MEE was a thin and watery effusion that flowed on inversion[8].
Statistical analysis
The Statistical Package of Social Science (SPSS Inc., Chicago, IL) for Windows version 11.5 was used to analyse the data. Chi square and specificity, positive predictive value (PPV), and negative predictive value (NPV) test were used for statistical evaluation of parameters. The statistical significance level was established at p < 0,05.
Results
In this study a total of 400 patient's 800 ears were evaulated. 175 (43.8%) patients were girls and 225 (56.2%) were boys. The ages were between 1-17 (mean age was 6.28 (± 2.99)). The primary complaints of the patients diagnosed with OME were as follows; open mouth breathing during sleep and snoring in 192 (48%) , hearing loss in 114 (28.5%), nasal obstruction in 45 (11.3%), recurrent tonsillitis in 25 (6.3%) , and 6 % presented with other symptoms. Morover 6% of the patient's had a history of previous operation (60% adenoidectomy; 40% adenotonsillectomy). In 2-years period of our follow-up, the operations were most frequently done in May by 16.8%. (Figure 1).
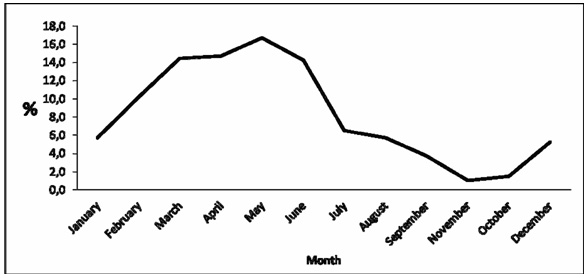 Büyütmek İçin Tıklayın |
Figure 1: Distribution of operations according to months of a year |
21.3% of patients had a history of smoke exposure ( same household mother and / or father smoking), 15.3% had a history of clinically diagnosed and treated allergies, 4.8% had a history of diagnosed and treated reflux by a pediatrician. Demographic characteristics of the patients are shown.(Table 1).
Table 1: Patients demographics.
Tympanometric evaluations were as follows; type-A 10. 9%, type-C1 25.0%, type-C2 50.5%, type-B 13.6%. Compliance and volume were calculated and they were 0.19 ± 0.18ml (0.01 to 1.16), 0.53 ± 0.23 ml (0.48 to 1.01) respectively. 79 cooperative children underwent audiometric testing. The right ear pure tone average was 29dB (± 10.6), the left ear pure tone average was 26 dB (± 10.9).
Binocular microscopic examination was normal in 10.5% of patients, dull in 43.2% , hypervascular in 27.8% and retracted in 18.5% .
Fluid was aspirated from middle ear during myringotomy in the 70.1% of the patients, and the charecteristic of the aspirate was serous in 256 patient (44.9%), mucoid in 314 (55.1%). (Table 2,3, Figure 2).
Table 2: Tympanometry results compared with effusion feature which was aspirated from middle ear.
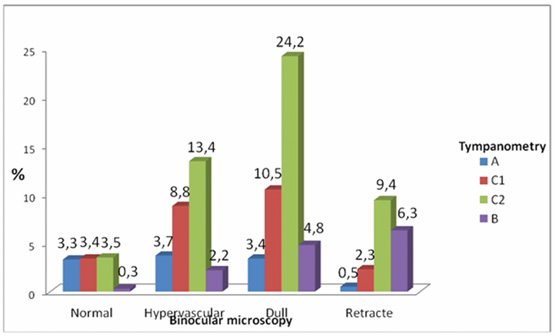 Büyütmek İçin Tıklayın |
Figure 2: Tympanic membrane findings according to binocular microscopy findings and comparison with tympanometry results |
Fluid aspiration during myringotomy was accepted as the gold standard for evaluation of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for tympanometric and binocular microscopic diagnosis. Calculated sensitivity for tympanometry was 93.6 %, specificity was 21.3%, positive predictive value (PPV) was 73.9%, negative predictive value (NPV) was 58.1%. For binocular microscopic examination sensitivity was as 94.5%, specificity 22.6%, PPV 74.4%, NPV 63.1% (Table 4).
Table 4: Comparison of diagnostic tools.
When the presence of fluid in middle ear is accepted as the only criteria for OME, the difference between gender was not statistically significant in patients with OME (χ2=0,642,p=0,349).
Patient age groups were classified as, group 1 (1-2 years of age ), group 2 (3-4 years of age), group 3 (5-6 years of age) and group 4 (7 years and older). Tympanometry and myringotomy results were compared within each group. While there was no statistically significant correlation (p = 0.097, χ2 = 2.70, p = 0.090, χ2 = 0.014) in group 1 and 2, we found statistically significant correlation in group 3 and 4 (p = 0.004, χ2 = 8.094, p = 0.000, χ2 = 38.457). In other words the accuracy of diagnosis of OME by tympanometry increased by age. When binocular microscopy findings and myringotomy results were compared within each group; we found statistically significant correlation in all age groups (p = 0.000, χ2 = 15.593, p = 0.000 χ2 = 0.004 χ2 = 12.583, p = 0.004 χ2 = 8.357, p = 0.000, χ2 = 20.340). Tympanometric results and binocular microscopic examination findings were classified according to the mentioned age groups and, sensivitity, specificity, PPV, and NPV values were determined (Table 5,6).
Table 5: Tympanometry for selected age groups.
Table 6: Binocular microscopy for selected age groups.
The relationship between predisposing risk factors and middle ear effusion (determined during myringotomy) was investigated. Accordingly, between OME and allergy no statistically significant relationship (p = 0.226, χ2 = 1.854), but there was significant relationship between OME and passive smoking (p = 0.02, χ2 = 5.450) and OME and gastroesophageal reflux (p = 0.05, χ2 = 3.701).
Discussion
There are certain individual and environmental risk factors for OME, including gender, socio-economic status, family history, birth and neonatal history including breastfeeding, passive smoking, recent history of hearing loss, allergies, nasal symptoms, acute tonsillitis, recurrent and recent upper respiratory tract infections, previous history of AOM, effect of seasons and attending to a daycare[2].The anatomy of an infant's ear canal differs between an older child or adult. Younger patients have smaller ear canals and less support, leading to collapse of the cartilaginous ear canal with minor pressure changes. Paradise et al. determined that tympanometric findings of patients younger than 8 months had no diagnostic value because the sensivity and specificity of tympanometry in this age group were 34.8% and 85.7% respectively[9,10]. Rogers et al. reported that tympanometric sensivity among the children aged 13-24 month was 92.1%, and specificity was 38.3% and the most valuable results optained in the 25-69 month age group, as spesivity increases.In our study, as the increase in the age; the increase in tympanometric positivity was significant (p = 0.004, χ2 = 8.094, p = 0.000, χ2 = 38.457). However, no significant difference was observed in terms of age groups in our study. Similarly Rogers[4]. et al. showed that as the increase in age; the increase in timpanometry specificity was observed (for 7 years and older patients; sensitivity was 93.1%, specificity was 32.7%, with PPD 77.8%, and NPV 58.1%).
A recent study showed binocular microscopy to be quite accurate in identifying middle ear effusions, but it did not assess the experience of the examiner[11]. However, patient cooperation during binocular microscopy is extremely impotant to make an accurate diagnosis, and this is often dependent on the patient's age.
Inhalational anaesthesia and positive pressure ventilation may affect findings at myringotomy. Middle ear changes under anaesthesia include both positive and negative middle ear pressure fluctuation, which may cause dispersion of the middle ear contents to the eustachian tube. This in turn may affect findings at myringotomy when comparing pre-operative tympanometry with intraoperative otomicroscopy[12,13].
Rogers et al. reported that the binocular microscopy applied by a pediatric otolaryngologist had the sensitivity of 88%, and specifity of 89%[4]. Takata et al. were unable to evaluate binocular microscopy and the impact of patient age in the diagnosis of otitis media with effusion[3].
In our study, we take the middle ear fluid as the gold standard value; and we found the most sensitive and specific diagnostic tool to assess was binocular microscopic examination, (sensitivity 94.5%, specificity 22.6%, PPV 74.4%, NPV 63.1%).
However, as a result of we found type-A timpanometry in 87 ears preoperativly where only 26 ears binocular intraoperative microscopic examination were evaluated as normal. However, 7.5% of these patients' had fluid aspirated in myringotomy and 41.8% of these fluid were mucoid. We could not found a study in literature that compared binocular microscopy and typanometry by using the aspirated middle ear fluid after myringotomy.
Important factor in restricting our work is that we don't have a group of patients under the age one (existing patients were excluded due to insufficient file information). There were some other limitations in our study; retrospective design of the study and routine otologic clinic examination without pneumotic otoscopy.
In our study we found that binocular microscopy is the most specific and sensitive diagnostic tool in the diagnosis of OME (sensitivity 94,5%, specifity 22,6%), although, it should be considered that anesthesia is likely to change the intraoperative findings. So in our opinion cooperative children binocular microscopy done outpatiently. We conclude that there is need for comparative, prospective studies investigating the diagnostic value of binocular microscopy.
Reference
1) Apostolopoulos K, Xenelis J, Tzagaroulakis A, et al. The point prevalence of otitis media with effusion among school children in Greece. Int J Pediatr Otorhinolaryngol 1998; 44:207-214. [ Özet ]
2) Gultekin E, Develioglu ON, Yener M, et al. Prevalence and risk factors for persistent otitis media with effusion in primary school children in Istanbul, Turkey. Auris Nasus Larynx 2010; 37:145–149. [ Özet ]
3) Takata GS, Chan LS, Morphew T, et al. Evidence assessment of the accuracy of methods of diagnosing middle ear effusion in children with otitis media with effusion. Pediatrics 2003; 112:1379-1387. [ Özet ]
4) Rogers DJ, Boseley ME, Adams MT, et al. Prospective comparison of handheld pneumatic otoscopy, binocular microscopy, and tympanometry in identifying middle ear effusions in children. Int J of Pediatr Otorhinolaryngol 2010; 74:1140-1143. [ Özet ]
5) Johnson KC. Audiologic assessment of children with suspected hearing loss. Otolaryngol Clin North Am 2002; 35:711–732. [ Özet ]
6) Jerger J. Clinical experience with impedance audiometry. Arch Otolaryngol Head Neck Surg 1970; 92:311-324. [ Özet ]
7) Zielhuis GA, Rach GH, Van den Broek P. The occurrence of otitis media with effusion in Dutch preschool children. Clin Otol 1990; 15:147-153. [ Özet ]
8) Carrie S, Hutton DA, Birchall JP, et al. Otitis media with effusion: components which contribute to the viscous properties. Acta Otolaryngol 1992; 112:504-511. [ Özet ]
9) Sassen ML, van Avaerm A, Grote JJ. Validity of tympanometry in the diagnosis of middle ear effusion. Clin Otolaryngol 1994; 19:185-189. [ Özet ]
10) Paradise JL, Smith CG, Bluestone CD. Tympanometric detection of middle ear effusion in infants and young children. Pediatrics 1976; 58:198–210. [ Özet ]
11) Young DE, Cate WJF, Ahmad Z, Morton RP. A accuracy of otomicroscopy fort he diagnosis of pediatric middle ear effusion. Int J. Pediatr Otorhinolaryngol 2009; 73:825-828. [ Özet ]
12) Chinn K, Brown OE, Manning SC. Effects of inhalant anaesthesia: tympanometry validation. Int. J. Pediatr. Otorhinolaryngol 2005; 69:187-192. [ Özet ]
13) Fish BM, Banerjee AR, Jennings CR, et al. Effect of anaesthetic agents on tympanometry and middle ear effusions. J Laryngol Otol 2000; 114:336-338. [ Özet ]




