EFFECTS OF NASAL PACKING ON THE QUALITATIVE AND QUANTITATIVE PROPERTIES OF TEAR FLUID AFTER SEPTOPLASTY
2Bozyaka EAH, Göz Kliniği, İzmir, Türkiye
3Sivas Devlet Hastanesi, KBB Kliniği, Sivas, Türkiye
Summary
Introduction: Septoplasty is one of the most common surgical procedures performed in otorhinolaryngology practice and is usually ended with nasal packing. Although nasal packing after septoplasty has a wide acceptance among rhinologists, various complications may occur due to packing itself.Materials and Methods: This prospective study included 13 patients who underwent septoplasty due to nasal septal deviation. Following surgery, patients were randomly divided into two groups, one with nasal packing (group 1, n=6) and other with trans septal suturing (group 2, n=7). The same ophthalmologist evaluated all patients during the preoperative first visit and at postoperative 48th hour by performing Schirmer test and tear break up time (BUT) measurement in order to record the quantitative and qualitative properties of tear fluid respectively.
Findings: The difference between pre and postoperative mean Shirmer's values was comparable between the groups for both sides. (p>0.05) The difference between pre and postoperative mean BUT was comparable between the groups for both sides. (p>0.05).
Conclusion: Nasal packing after septoplasty is a controversial procedure in otorhinolaryngology practice. Trans septal suturing is introduced as a more safe and comfortable alternative to nasal packing by most of the surgeons. This study showed that nasal packing after septoplasty does not have any negative effect on nasolacrimal drainage system and tear fluid dynamics of the patients.
Introduction
Surgical correction of a deviated nasal septum is one of the most common otorhinolaryngological procedures worldwide and it may be performed alone or as part of a surgical plan.[1] In the history of septoplasty, numerous modifications about the surgical procedure have been introduced in order to achieve less complicated and improved results. Unfortunately, septoplasty is still not a complication free surgery and numerous unwanted conditions as bleeding, synechiae formation or septal hematoma may be associated with it during or after the procedure.[2] Various intraoperative and postoperative measures have been developed to prevent these complications, including proper subpericondrial elevation, trans septal suturing or postoperative nasal packing. Of these measures, nasal packing is the most controversial one because of its potential and dangerous complications such as dysphagia, aspiration, airway obstruction, hypoventilation, hypoxemia, local and/or general infections and feeling of discomfort and reduced quality of life.[3]Orbital structures and lacrimal apparatus have close relationship with nasal cavity both anatomically and physiologically. Tear fluid drainage pathway ends in nasal cavity through the nasolacrimal duct, which places beneath the lateral wall of the nasal cavity and opens to the inferior nasal meatus. Both lacrimal drainage system and nasal cavity have capability to affect each other by this close anatomical and physiological relation. In this study we aimed to investigate the effects of nasal packing on the qualitative and quantitative properties of tear fluid after septoplasty.
Methods
The ethical committee of the institution had approved the study protocol with a file number 142/2013. All participants had given informed consent prior to surgery. Procedures had performed between November 2013-April 2014. Patients were recruited among adult men and women who have a complaint of nasal obstruction due to a deviated nasal septum and scheduled to undergo nasal septal surgery under local anesthesia. Patients those have additional systemic diseases, history of prior nasal septal or nasolacrimal system surgery or ongoing infectious condition were excluded from the study. Eighteen (n=18) patients who fulfilled the criteria have been evaluated by the ophthalmologist preoperatively in order to confirm the nasolacrimal system patency. Five of them had a concurrent nasolacrimal duct obstruction at the same side with the nasal deviation and excluded from the study. Other 13 patients had patent nasolacrimal systems bilaterally and scheduled to undergo septal surgery.
Surgical procedure
Surgical procedures have been performed under local anesthesia and all participants were received 10 mg intramuscular diltiazem hydrochloride for premedication and 1gram intravenous co-amoxiclav for antimicrobial prophylaxis. Xylomatazoline 0,1% soaked cottons were used for nasal mucousal decongestion. Vascular hemostasis was achieved by injection of 2 ml lidocaine HCI 1% with adrenaline 1: 100000. Our approach briefly consisted of Killian incision, creation of subpericondrial tunnels, posterior chondrotomy, osteotomy if needed and septal reconstruction. Trans septal suturing was applied to all patients by 4-0 absorbable materials. Suturing was performed in a “continue fashion” starting from the most posterior and ends at anterior part of the septum (Figure 1). The patients were randomly allocated into two groups as group 1 (packing group) and group 2 (trans septal suturing only). Each nasal cavity was packed with a Merocel® (Medtronic Xomed, Jacksonville, Florida) in 6 patients at group 1 (Figure 2). Packs were free of any kind of lubricant agent or antimicrobial topical pomade and kept in nasal cavity for 48 hours. All patients received per-oral 500 mg second-generation cephalosporin for prophylaxis.
 Büyütmek İçin Tıklayın |
Figure 1: Endoscopic view of trans-septal sutures |
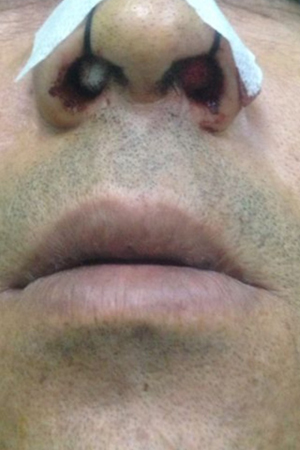 Büyütmek İçin Tıklayın |
Figure 2: Nasal cavities packed with Merocel® |
Ophthalmologic examination
The same ophthalmologist evaluated all patients during the preoperative first visit and at postoperative 48th hour by performing tear film break up time (BUT) measurement and Schirmer test in order to record the qualitative and quantitative properties of tear fluid respectively. The BUT was measured first using a cobalt blue filter on slit-lamp examination. A sterile fluorescein strip containing 1 mg fluorescein sodium was applied on the inferior bulbar conjunctiva (Madhu Instruments, Delhi, India). The strip was moistened with normal saline solution prior to application. The interval between a complete blink and the appearance of the first dry spot was noted (Figure 3). Two measurements were taken in succession and averaged.[4] The participant then waited for 30 minutes, and Schirmer's test with anesthesia (alcaine) was performed with the eyes closed by placing the test strip over the inferior lid margin towards the lateral canthus. After waiting for another 30 minutes, the Rose Bengal test was performed by applying a moistened sterile strip containing 1.5 mg Rose Bengal over the inferior bulbar conjunctiva (Figure 4). A van Bjisterveld score of 4 or more was considered positive for dry eye syndrome.[5] Mean values for Schirmer's test and BUT of groups were compared statistically using Mann–Whitney U test.
 Büyütmek İçin Tıklayın |
Figure 3: Application of Schirmer test |
 Büyütmek İçin Tıklayın |
Figure 4: Tear break up time measurement (biomicroscopic view) |
Results
Of the 6 patients packed with Merocel, 4 were male and 2 were female with an age ranging from 20 to 60 (mean 37,44±2,18). Of the 7 patients in suture group, 4 were male and 3 were female with an age ranging from 19 to 52 (mean 33,1±2,48). No postoperative complication occured in groups. The difference between pre and postoperative mean Shirmer's values was comparable between the groups for both sides. (p>0.05) The difference between pre and postoperative mean BUT was comparable between the groups for both sides. (p>0.05) Mean values for each test results are summarized in Table 1.Discussion
Septoplasty has a pivotal role in the surgical management of deviated nasal septum and is usually ended with nasal packing. The main goals of packing are to maintain hemostasis, prevent septal hematoma and create structural support.[6] However, nasal packing may be related to numerous unwanted conditions postoperatively. Albeit most of these problems are less problematic and managed easily (mucosal adhesions, minor bleedings), rarely they are much more serious and deadly (toxic shock syndrome, spinal osteomyelitis, meningitis).[7,8] In addition to these minor or major medical difficulties, nasal packing is also associated with various degrees of patient discomfort. Cukurova et al. showed that patients with Merocel packing had significantly more pain and nasal discomfort compared to the patients who received only trans-septal suturing.[9] In contrast to these findings, considerable amount of nasal surgeons are still believed to advocate the benefits of nasal packing and chose to use the different types of packing materials in their routines. Another important aspect of this controversy is the point of view of the patients. As we observed in our practice, patients are more curious to receive un-packed septoplasty these days. In literature there are different thoughts and results about the complication rates of septoplasty with and without packing. For example Naghibzadeh showed that the rate of complication and morbidities between packing and suture groups were same and the differences were not significant, except the pain and discomfort post operatively and during pack removal.[10] However Von Schoenberg and colleagues found that a higher rate of complications (including hemorrhage, vestibulitis and septal perforation) were observed in the packed group compared to un-packed group.[11] Besides these negative literature findings, Laing, MR & Clark and El-Silimy shows that nasal packing after septoplasty has a direct pressure effect to the septal flaps and to the blood vessels located in the nasal septum and thus, prevents postoperative bleeding and hematoma formation.[11] Unfortunately this data has not been supported by other studies with large number of cases.Complications of septoplasty have a wide spectrum and incidence can range anywhere from 5% to 60%.[12] Possible perioperative or postoperative complications may arisen from any organ or system that adjacent to nasal cavity. From dental pulp necrosis to unilateral hemiplegia, many different and unique cases were introduced in the literature.[13] Among these complications, specific ophthalmological problems such as temporary mydriasis, periorbital emphysema, central retinal artery occlusion, extra ocular muscle trauma had been reported.[14] Although there is no reported specific complication about nasolacrimal apparatus in literature, close proximity of surgical field with the nasolacrimal system and indirectly with tear fluid cause attention about the possible interaction between them during or short after the procedure. According to our findings, we may conclude that septoplasty procedure seems altering tear fluid dynamics insignificantly. Similarly, in their study Durmaz et al. showed that ocular flora might alter following septoplasty.[15] Their study had pointed out the possible interaction and relation between septal surgery and lacrimal system. More specifically our findings revealed that nasal packing has no additional effect on nasolacrimal drainage compared to trans septal suture method. While there are plenty of questions and ongoing debates about the necessity of using nasal packs after septoplasty, our results may justify and acquit nasal packing at least about the possible negative impacts of it on to the nasolacrimal system and tear fluid.
Conclusion
Although there are very limited data and clinical experiences about the effects of septoplasty and especially nasal packing on lacrimal system dynamics and tear properties postoperatively, our results revealed that nasal packing do not alter tear fluid quality and quantity significantly. However future studies that have more comprehensive design may expand our knowledge about this issue.Declaration of conflicting interests: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article
Funding: The authors received no financial support for the research and/or authorship of this article.
Reference
1) Özkiris M, Kapusuz Z, Öztürk S, Bolat E, Saydam L. The effects of sevoflurane and isoflurane in nasal septal surgery. J Craniofac Surg. 2013; 24(2):592-5. [ Özet ]
2) San T, Ertugay OC, Catli T, Acar M, Ertugay CK, Dag I et al. Effects of surfactant on biofilm formation on silicone nasal splints. Eur Arch Otorhinolaryngol. 2014 May 30. [Epub ahead of print] [ Özet ]
3) Hajiioannou JK, Bizaki A, Fragiadakis G, Bourolias C, Spanakis I, Chlouverakis G et al (2007) Optimal time for nasal packing removal after septoplasty. A comparative study. Rhinology.Mar; 45(1):68-71. [ Özet ]
4) Lemp MA. Report of the National Eye Institute/Industry workshop on Clinical Trials in Dry Eyes. CLAO J 1995; 21:221-32. [ Özet ]
5) Van Bijsterveld OP. Diagnostic tests in the Sicca syndrome. Arch Ophthalmol 1969;82:10-4. [ Özet ]
6) Al-Raggad DK, El-Jundi AM, Al-Momani OS. Suturing of the nasal septum after septoplasty, is it an effective alternative to nasal packing? Saudi Med J.2007; 28:1534–1536. [ Özet ]
7) Mäkitie A, Aaltonen LM, Hytönen M, Malmberg H. Postoperative infection following nasal septoplasty. Acta Otolaryngol Suppl.2000; 543:165-6. [ Özet ]
8) Mane RS, Patil B, Mohite A. Comparison of septoplasty with and without nasal packing and review of literature. Indian J Otolaryngol Head Neck Surg. 2013;65:406-8. [ Özet ]
9) Cukurova I, Cetinkaya EA, Mercan GC, Demirhan E, Gumussoy M. Retrospective analysis of 697 septoplasty surgery cases: packing versus trans-septal suturing method. Acta Otorhinolaryngol Ital. 2012 Apr;32(2):111-4. [ Özet ]
10) Naghibzadeh Bijan, Peyvandi Ali Asghar, Naghibzadeh Ghazal. Does post septoplasty nasal packing reduce complications? Acta Medica Iranica.2011; 49:10–12. [ Özet ]
11) Von Schoenberg M, Robinson P, Ryan R. Nasal packing after routine nasal surgery: is it justified? J Laryngol Otol.1993; 107:902–905. [ Özet ]
12) Bloom JD, Kaplan SE, Bleier BS, Goldstein SA. Septoplasty complications: avoidance and management. Otolaryngol Clin North Am. 2009 Jun;42(3):463-81. [ Özet ]
13) D'Ascanio L, Cappiello L, Piazza F. Unilateral hemiplegia: a unique complication of septoplasty. J Laryngol Otol. 2013 Aug;127(8):809-10. [ Özet ]
14) Güvenç G, Eren E, Arslanoğlu S, Yüceer N. A rare complication of septoplasty: tension pneumocephalus without rhinorrhea. J Craniofac Surg. 2014;25:360-1. [ Özet ]
15) Durmaz E, Dursun E, Iriz A, Mumcuoglu I, Eryilmaz A. Changes in the ocular and nasal cultures in patients who had undergone septoplasty. J Otolaryngol Head Neck Surg. 2011 Dec;40(6):493-8. [ Özet ]




