A NOVEL MINIMALLY INVASIVE SURGICAL APPROACH TO PRIMARY OPTIC NERVE MENINGIOMA: CASE REPORT
2S.B. Dışkapı Y.B. Eğitim ve Araştırma Hastanesi, KBB Kliniği, Ankara, Türkiye
3S.B.Dışkapı Yıldırım Beyazıt Eğitim ve Araştırma Hastanesi, Patoloji Kliniği, Ankara, Türkiye
Summary
Primary optic nerve sheath meningiomas (ONSM) are rare tumors of optic nerve which account for approximately 5-10% of orbital neoplasms. The classic triad of optic atrophy, progressive visual loss and presence of opticociliary shunt vessels is pathognomonic for the clinical presentation of ONSM however only a few percent of cases has this classic presentation. The most common presenting symptom in these patients is painless, progressive loss of visual acuity and dyschromatopsia. On clinical examination pathologic appearance of optic disc with varying degrees of optic atrophy is commonly observed. The goal of treatment for cases of ONSM is tumor control and improvement of vision. In cases with small and non-progressive tumor and high functional vision, conservative follow-up of the lesion is appropriate since surgical excision of ONSM is generally associated with high visual morbidities. Here we present a 67-year-old female patient with primary ONSM located on retrobulbar space with a diameter of 2x2cm. On visual field test partial defect and blind spot enlargement were found. The patient underwent endoscopic resection of tumor and optic nerve decompression procedure. The operation was completed without early complication and postoperative follow-up was uneventful. Histopathological examination confirmed the diagnosis of optic nerve sheath meningioma.Introduction
Orbital meningiomas are relatively rare tumors and constitute %1-2 of all orbital tumors and all meningiomas[1,2]. Definitive treatment is challenging, however surgical excision has almost always resulted in postoperative blindness in the affected eye[3,4]. The optimal treatment of ONSMs has remained poorly defined. Here we report a 67-year-old female patient with a mass lesion on retrobulbar space. The incidence, clinical presentation, histopathological characteristics, and imaging findings associated with ONSM as well as current treatment modalities for these lesions, with an emphasis on endoscopic surgical resection was discussed in the light of the literature.Case Presentation
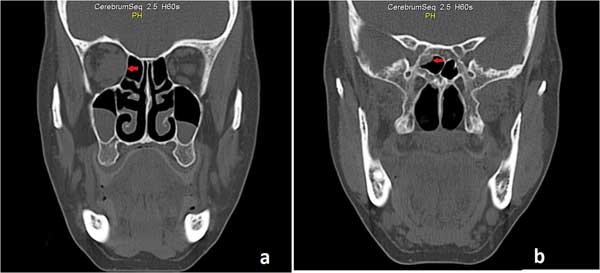
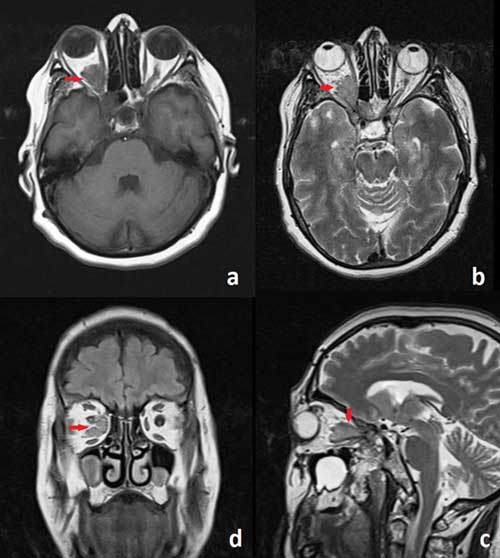
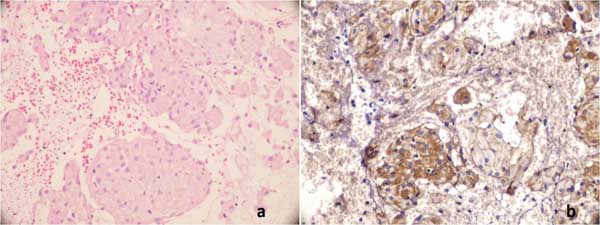
A 67-year-old female patient consulted to ENT clinic with right sided proptosis. Visual acuity was 1.1/1.5 OD and 1.2/1.2 OS and fundoscopic examination revealed no atrophy or edema of the optic disc and no lesion of the optic bulb. Partial defect and blind spot enlargement were found on right side of visual field test. Thyroid hormones were measured within normal limits. Computed tomography (CT) scan and magnetic resonance imaging (MRI) of eye indicated a retrobulbar mass lesion with a diameter of 2x2cm which was diagnosed as a meningioma (Figure 1, Figure 2). The patient was planned for endoscopic resection of tumor and optic nerve decompression procedure under general anesthesia. The patient was informed about her situation and a signed consent was obtained. Intraoperatively uncinectomy, anterior and posterior ethmoidectomy was performed there after lamina papyracea was identified and its bony covering was taken. Sphenoid sinus was widened by drilling bone inferior to it. Tumor that located in retrobulbar space and projected lateral to sphenoid sinus was recognized. Tumor was dissected between medial and inferior rectus muscles. Tumor was aspirated by using the CUSA (Cavitron Ultrasonic Surgical Aspirator) which is an ultrasonically powered aspirator that selectively fragments and aspirates parenchymal tissue while sparing vascular and ductal structures. During operation, annulus of Zinn and optic nerve were identified and protected. Operation was completed without early complication and postoperative follow-up was uneventful. Histopathological examination confirmed the diagnosis of optic nerve sheath meningioma. Immunohistochemical stainig of tumor revealed positivity with EMA (Epithelial membrane antigen), S-100, keratin (Figure 3). Ocular movement recovered completely and proptosis resolved within 1 year of surgery. There was no evidence of recurrence to the present.
 Büyütmek İçin Tıklayın |
Figure 1: Paranasal computed tomography (CT) images. (a) Coronal CT demonstrating intraorbital tumoral lesion (arrow). (b) Coronal CT demonstrating tumoral lesion projected into right sphenoid sinus (arrow). |
 Büyütmek İçin Tıklayın |
Figure 2: (a,b) Axial T2-weighted MR imaging of case revealed ONSM measuring 2x2cm in the retrobulbar compartment of the right orbit causing proptosis (arrows). (c) Sagittal and (d) coronal T2-weighted MR images showing ONSM (arrows). |
 Büyütmek İçin Tıklayın |
Figure 3: (a) Solid nests of meningoepithelial cells arranged in whorls, HEx100. (b) EMA (epithelial membrane antigen) positivity was shown, x100. |
Discussion
Primary optic nerve sheath meningiomas (ONSM) are rare tumors of optic nerve that only 53 (4%) were found in 1264 consecutive patients referred for an orbital mass, and Berman and Miller[3] reported that ONSMs comprise 1-2% of all meningiomas[4]. ONSMs occur more commonly middle aged women. In a review of the ONSM literature, Dutton[2] reported the mean age at presentation of ONSM patients to be 40.8 years (42.5 years in women and 36.1 years in men; range 3–80 years), with 61% of the patient population being female, a degree of female predominance similar to that associated with intracranial meningioma.ONSMs may be primary or secondary. Secondary ONSMs arise intracranially from dura on or near the planum sphenoidale and spread to surround the orbital portion of the nerve, whereas primary ONSMs arise from arachnoid cap cells within the dural sheath surrounding the orbital or, less commonly, the canalicular portion of the optic nerve[5]. The growth pattern is typical for meningiomas, and growth normally follows the path of least resistance. As with intracranial meningiomas, the WHO (World Health Organization) classification identifies 3 histological grades of ONSMs: I, benign; II, atypical; and III, malignant. Recurrence rates are associated with WHO malignancy grade and have been reported to be 6.9, 34.6, and 72.7%, respectively[6]. Tumor presented here was classified into grade1.
Clinical manifestations include ipsilateral visual loss, color vision disturbance, visual field defect, proptosis, optic disc edema and motility disturbance. Even patients who do not have significant reduction in visual acuity often have disturbances of color vision and visual field defects. Less common symptoms in patients with ONSMs include pain or discomfort, double vision, and transient visual obscurations[7]. The obscurations of vision are almost always associated with optic disc swelling and in some cases are exacerbated or induced by eye movement. In the presenting case proptosis was the only symptom and fundoscopic exam was normal.
The diagnosis of OSNM relies heavily on imaging findings. Because OSNMs tend to grow outward from the nerve sheath, they are less likely to efface the CSF layer between the nerve and sheath a property that sometimes helps to differentiate meningioma from glioma. Calcification is also a common characteristic of meningioma. MRI currently remains the modality of choice for diagnosis of OSNM, although less sensitive than CT in the recognition of calcification. ONSMs are typically isointense or slightly hypointense to brain and optic nerve tissue on T1 weighted images and hyperintense (may also be hypointense) on T2 weighted images[8].
Traditionally, orbital meningiomas have been observed without intervention, or treated by excision of the tumor along with the nerve because of difficulty of surgical approach. Attempts to excise these tumors while keeping the optic nerve intact had been unsuccessful and most patients are blind in the eye following such surgery[3,4]. Trials of medical therapy for ONSM have not been successful because of a variety of hormone expression. Recently stereotactic fractionated radiotherapy (SFR) was reported as successful treatment for ONSM, however late toxicity due to irradiation are sometimes seen including the optic nerve, retina, pituitary gland, and the white-matter tracts of the brain[3]. These undesirable complications bring continuous distress for the patients and decrease their quality of life. Consequently an aggressive procedure such as skull base approaches and basal frontal craniotomy was considered unnecessary when patient's age is relatively advanced and the risk of potential damage to the optic nerve is high.
The goal of the transnasal endoscopic approach is removal of as much of the lesion as possible, avoiding brain retraction, and minimizing neurovascular structure manipulation. Because of the strategic localization of the sphenoid sinus, retrobulbar space can be exposed, passing through this air-filled cavity, depending upon its grade of pneumatization. Such a route, reduces the risks of brain injury and allows one to perform an early decompression of the optic canals, thus resulting in a better visual outcome[9]. Because the major clinical presentation symptom is visual change, improvement and/or preservation of visual function takes priority in this surgery. Visual function, investigated before and after surgery, remained unchanged in our patient.
Reference
1) Carrasco JR, Penne RB: Optic nerve sheath meningiomas and advanced treatment options. Curr Opin Ophthalmol 2004;15:406–10. [ Özet ]
2) Dutton JJ: Optic nerve sheath meningiomas. Surv Ophthalmol 1992;37:167–83. [ Özet ]
3) Berman D, Miller NR: New concepts in the management of optic nerve sheath meningiomas. Ann Acad Med Singapore 2006;35:168–74. [ Özet ]
4) Kim JW, Rizzo JF, Lessell S: Controversies in the management of optic nerve sheath meningiomas. Int Ophthalmol Clin 2005;45:15–23. [ Özet ]
5) Wilson WB. Meningiomas of the anterior visual system. Surv Ophthalmol 1981;26:109-27. [ Özet ]
6) Turbin RE, Pokorny K: Diagnosis and treatment of orbital optic nerve sheath meningioma. Cancer Control 2004;11:334–41. [ Özet ]
7) Saeed P, Rootman J, Nugent RA, White VA, Mackenzie IR, Koornneef L. Optic nerve sheath meningiomas. Ophthalmology 2003;110:2019-30. [ Özet ]
8) Mafee MF, Goodwin J, Dorodi S: Optic nerve sheath meningiomas. Role of MR imaging. Radiol Clin North Am 1999, 37:37-58. [ Özet ]
9) Gardner PA, Kassam AB, Thomas A, Snyderman CH, Carrau RL, Mintz AH, Prevedello DM. Endoscopic endonasal resection of anterior cranial base meningiomas. Neurosurgery. 2008;63(1):36-52. [ Özet ]




