EFFECT OF TRANSTYMPANICALLY APPLIED GASTRIC CONTENT ON DISTORTION PRODUCT OTOACOUSTIC EMISSIONS IN RABBITS
2Bayındır Devlet Hastanesi, KBB, İzmir, Türkiye
3Celal Bayar Üniversitesi Tıp Fakültesi, Histoloji ve Embriyoloji, Manisa, Türkiye
4Dokuz Eylül Üniversitesi, Deney Hayvanları Bilim Dalı, İzmir, Türkiye
Summary
Purpose: Gastro-oesophageal reflux is a common problem in children and even in adults. Many otolaryngological problems were linked to reflux induced inflammation. Reflux has been implicated as a culprit in otitis media with effusion mostly in children.Materials and Methods: Sixteen rabbits were used. Animals were divided into two groups. One group received its own gastric content and the other group received saline transtympanically for twenty days. Hearing levels were evaluated with distortion product otoacoustic emissions (DPOAE) on day 0 and day 27. Animals were sacrificed on day 27 and histological analyses of middle ear were performed.
Results: Epithelial thickness of the middle ear mucosa, capillary vasodilatation and inflammatory cell count were all significantly increased in the gastric-content group compared with the control group ([(p = 0.002, χ2 = 12.667) (p = 0.004, χ2 = 11.200), p < 0.001 respectively). The comparison of pre and post procedure difference of ( signal to noise ratio) SNR levels between gastric content and control groups revealed statistically significant difference in 0.5 and 1 kHz frequencies (p = 0.017, p = 0.017 respectively).
Conclusion: Transtympanicaly applied gastric content is found to induce middle ear inflammation and decrease in cochlear reserve in 0.5 and 1 kHz frequencies.
Introduction
Gastro-oesophageal reflux (GER) is common in children and is associated with morbidity and mortality[1]. In the first few months of life (0-3 months), postprandial reflux is a physiological event which gradually decreases, disappearing by one year of age[2]. The passage of gastric contents from the oesophagus into the respiratory and otolaryngeal tracts is extra-oesophageal reflux.Extra-oesophageal reflux is implicated in various otolaryngologic diseases such as laryngitis, subglottic stenosis[3], chronic sinusitis[4], and otitis media[3]. Given anatomic and physiologic immatury of Eustachian tube in children, they are prone to otitis media with effusion (OME) compared to adult population. Extra-oesophageal reflux can cause inflammation of Eustachian tube, impaired mucociliary clearance, obstruction of the tube and stasis of secretions and eventually effusion. Pepsin was demonstrated in middle ear of patients with otitis media with effusion[5]. A recent study O'Reilly et al demonstrated pepsin in the middle ear cleft of 20% of paediatric patients with otitis media undergoing tympanostomy tube placement, compared with 1.4% of controls[6].
Hearing loss caused by OME can be evaluated using otoacoustic emissions (OAE). Studies indicate that cochlear reserve can be monitored especially with distortion product otoacoustic emissions (DPOAE) in patients with OME[7,8].
Here we use an experimental reflux induced middle ear inflammation model to evaluate the effect of gastric content induced inflammation on hearing levels and cochlear reserve.
Methods
All animals were treated in accordance with protocols approved by the Animal Care and Use Committee of Dokuz Eylul University. The study was conducted at the animal care facility of Dokuz Eylul University Faculty of Medicine. Sixteen healthy adult New Zealand rabbits (2271 to 3182 g each) with no external or middle ear pathology were used.The animals were anesthetized by intramuscular administration of Xylazine (Basilazin, 5 mg/kg; Animedica GmbH, Senden-Bosensell, Germany) and ketamin (Ketalar, 50 mg/kg; Eczacıbaşı Warner Lambert, Istanbul, Turkey). DPOAE (Vivosonic Integry V500 Toronto, Ontario, Canada) measurements were made using tympanometry probes adjusted to fit in the rabbit ear canal. Baseline DPOAE measurements were taken from the ears before the procedure. The cochlear activity of ear of all rabbits was examined in day 0 and day 21, using DPOAEs in sedated animals. Once the probe was placed with a good seal in the ear canal, the DPOAEs were measured. Equilevel primary tones f1 (65 dB) and f2 (55 dB) were fixed at f1/f2 = 1.22, and DPOAEs were measured at seven different frequencies ranging from 0,5 to 8 kHz (0,5, 1, 2,3, 4, 5, and 8 kHz). By calculating the difference between the distortion products and noise standard deviations, the signal–noise ratios (SNR) for each frequency were found. Two DPOAE measurements were obtained on days 0, and 21 in order to detect any possible deterioration in cochlear activity. All measurements were recorded in a quiet room.
Under microscopic observation, a tympanic perforation was created using a pick. Gelfoam was inserted through the perforation to prevent tympanic membrane closure. After the surgical procedure, the animals were divided into two groups of eight each. The rabbits received either their own gastric contents (gastric-content group, n = 8) or saline (control group, n = 8) transtympanically injected with a 23-gauge dental syringe, once daily (0.1 mL/day) for 20 days. On day 27, the rabbits were euthanized by injection of a lethal dose of pentobarbital sodium and isopropyl alcohol. After decapitation, the temporal bones were harvested.
Formalin-fixed, paraffin-embedded samples of tissues from control and experimental rabbits were prepared by routine paraffin embedding procedures. In brief, tissue samples were fixed in 10% formalin for 24 to 48 h, dehydrated in a graded series of ethanol, cleared in xylene, and embedded in paraffin. Paraffin blocks were serially sectioned at a thickness of 5 μm and prepared for histochemical staining. Serial sections were obtained from middle ear tympanic membrane to middle ear promontorium mucosa. For histological assessment, sections were stained with hematoxylin and eosin (H&E). The sections observed under a bright-field microscope (BX 40; Olympus, Tokyo, Japan). Control samples were processed in an identical manner. Two blinded observers independently and scored the H&E stained sections for epithelial thickness, capillary vasodilatation and number of inflammatory cells.
Statistical analysis
SPSS 16 for Windows was used for the statistical analysis. Histochemical staining differences were evaluated using the contingency-table analysis using the χ2 test. Fisher's exact test was used when numbers in one of the cells were < 5. SNR level intragroup differences were evaluated with Wilcoxon signed rank test, and inter group differences with Mann-Whitney U test. The statistical significance level was established at P < 0.05, and confidence intervals were 95%.
Results
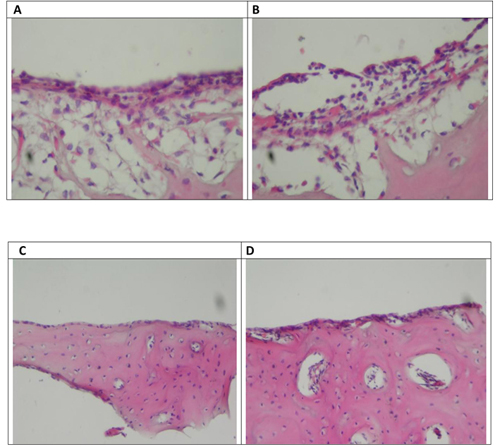
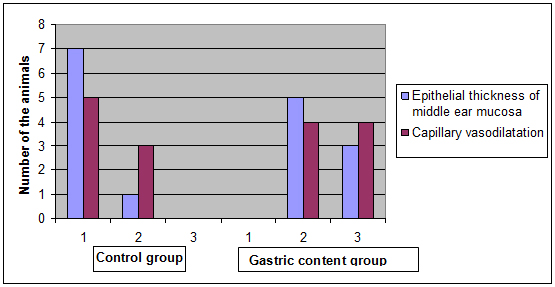
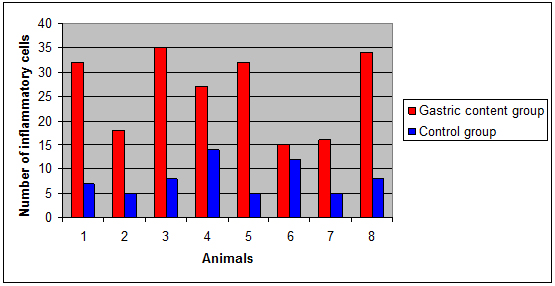
Histological findingsIn the control group, microscopic observations of the H&E-stained sections confirmed that the middle ear space contained simple squamous epithelium, consistent with bone. In the gastric-content group, microscopic observations of the H&E-stained sections revealed thickened lamina propria and epithelium lining; increased numbers of active fibroblasts, collagen fibres, and inflammatory cells; and vascular dilatation (Figure 1). Scores for epithelial thickness (normal, 1; mildly thickened, 2; and thickened two-fold, 3; and capillary vasodilatation (none, 1; mildly increased, 2; and increased, 3) were assigned for each group (Figure 2). Epithelial thickness of the middle ear mucosa, and capillary vasodilatation were all significantly increased in the gastric-content group compared with the control group (3 X 2 contingency-table analysis using the χ2 test, confidence interval % 95 ) [ (p = 0.002, χ2 = 12.667) ( p = 0.004, χ2 = 11.200), and ( p = 0.01, χ2 = 9,143) respectively). Inflammatory cells were significantly increased in gastric content group compared with the control group ( Mann- Whitney U test , p < 0.001) (Figure 3)
 Büyütmek İçin Tıklayın |
Figure 1: H&E-stained sections of the middle ear from rabbits in the gastric-content and control groups. (A-B) Control group. (C-D) Gastric-content group. Thickening of the epithelium, increased numbers of active fibroblasts and collagen fibers in the lamina propria, increased capillary dilatation, and increased number of inflammatory cells is seen. Ep: epithelium. Lp: lamina propria. Cp: capillary. B: bone. |
 Büyütmek İçin Tıklayın |
Figure 2: A graphic showing comparison of the histopathological scores of the control and gastric-content groups. The scoring of each parameter was as follows: Epithelial thickness of the middle ear mucosa: normal, 1; mildly thickened, 2; or thickened two-fold, 3. Number 2. Capillary vasodilatation: none, 1; mildly increased, 2; or increased, 3. |
 Büyütmek İçin Tıklayın |
Figure 3: Comparison of the number of inflammatory cells in both groups (x400 magnification) |
Audilogic Assessment
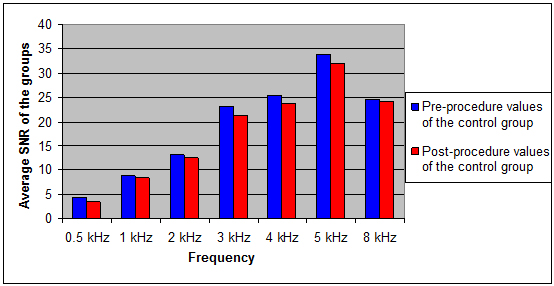
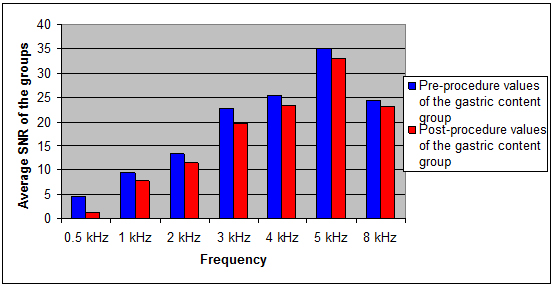
The comparisons of pre-procedure and post-procedure SNR levels are listed in Figures 4 and 5. In control group the differences of pre and post-procedure SNR levels in 0.5, 1, 3, 4, 5 kHz frequencies were found to be statistically significant ( p < 0.05). In gastric content group the differences of pre and post-procedure SNR levels in 0.5, 1,2 ,3, 4, 5 kHz frequencies were found to be statistically significant (p < 0.05). The comparison of pre and post procedure difference of SNR levels between gastric content and control groups revealed statistically significant difference in 0.5 and 1 kHz frequencies (p < 0.05).
 Büyütmek İçin Tıklayın |
Figure 4: The comparison of pre-procedure and post-procedure signal noise to ratio (SNR) levels of the control group |
 Büyütmek İçin Tıklayın |
Figure 5: The comparison of pre-procedure and post-procedure SNR levels of the gastric content group |
Discussion
Otitis media with effusion is one of important cause of hearing loss in children. Extra-oesophageal reflux is one of the underlying culprits of OME[9]. In our study we create an experimental reflux model for evaluating pattern of gastric content induced hearing loss and assess the destructive effect of gastric content on cochlear reserve audilogically.Heavner et al reported repeated exposure of pepsin in hydrochloric acid transtympanically leads to Eustachian tube dysfunction.[10] Although they do not assess hearing status, Eustachian tube dysfunction is the most important factor in middle ear disease[11], and it can be speculated reflux can induce a chain of inflammatory events that lead to OME and hearing loss.
In our study both in control and gastric content group show evidence of hearing deterioration. Except ın frequencies 2 kHz and 6 kHz in control group and 6 kHz in study group, the intervention, regardless of inciting agent, seem to cause hearing loss in most of the frequencies. The difference of SNR levels between study and control group on the contrary, reveal statistically significant hearing loss in frequencies 0.5 and 1 kHz.
In a recent study, Tas et al reported 19 children (38 ears) with OME who are scheduled for myringotomy and/or ventilation tube insertion were evaluated with DPOAE[8]. They found that especially glue ear effusion can cause a reduction in emissions in 2, 4 and 8 kHz. A similar study performed on 43 children (85 ears) Yeo et al has concluded that middle ear effusion could affect the expression of DPOAE in frequencies 3 and 4 kHz[12]. Both of these papers do not investigate the underlying factors that cause effusion.
In our study hearing loss observed nearly all frequencies measured in both groups might reflect the fact that perforated tympanic membrane and the fluids that fill the middle ear might result in deterioration of hearing status. Histological investigation revealed increased epithelial thickness of the middle ear mucosa, capillary vasodilatation and increased number of inflammatory cells compared to control group. As shown by histological evidence pronounced inflammation in study group might be responsible of low frequency hearing loss as compared to control group. This could be consequence of gastric content induced middle ear effusion.
It is known that ototoxic effects are initially seen in the high frequency region of the cochlea and lower frequencies are affected in the late stage of the ototoxic drug administration. Locally administrated povidine-iodine solution could cause transient otoacoustic emission disappear[13]. In rabbit ototoxicity model, Oghan et al assessed transtympanically administrated gentamicin and tobramycin with DPOAE and concluded that low frequencies (2 and 3 kHz) are more sensitive to the administration of topical gentamicin than to topical tobramycin[14]. The ototoxicity of topically applied agents is different between laboratory animals and humans. This may explained by the fact that in humans the round window is deeper and thicker than in small laboratory animals[15]. Statically significant decreased in cochlear reserve of the study group in frequencies 0.5 and 1 kHz were found. It can be speculated that gastric content might induce cochleotoxic effect on low frequencies. A recent study investigated ototoxicity of gastric reflux on rats. They prepared acidified gastric pepsin by the addition of HCl and deionized water to pepsinogen from porcine stomach and demonstrated that the acidified gastric pepsin caused statistically significant hearing loss in the experimental ears.[16] The discripancy between results might result from the methodogy of the studies. In our study we used animal's own gastic content that resembles natural content of the laryngopharyngeal reflux.
A recent interesting study by Deppe et al.[17] demonstrated that conductive hearing loss (CHL) alters the L2/L1 ratio that reaches the inner ear. As consequence of a CHL, the absolute DPOAE level alterations strongly depend on the L2,L1 combinations. They stated that as consequence of a CHL, DPOAE level can increase and concluded that Continuously increasing CHL values do not necessar¬ily result in monotonically decreasing DPOAE level alterations.
There is some certain limitation of our study. Although we have histological examination of middle ear, there is no scanning microscopic examination of cochlea. A scanning electron microscopic examination of cochlea might support our speculation if gastric content is cochleotoxic. In our study hearing loss observed nearly all frequencies measured in both groups might reflect the fact that perforated tympanic membrane and the fluids that fill the middle ear might result in deterioration of hearing status. Histological investigation revealed increased epithelial thickness of the middle ear mucosa, capillary vasodilatation and increased number of inflammatory cells compared to control group. Apart from the previous clinical studies mentioned our result show low frequency hearing loss. We have demonstrated that gastric acid induced middle ear effusion in an animal model result in a decreased SNR level in 0.5 and 1 Hz. Most of the clinical studies that evaluate the value of DPOAE in OME, did not investigate the inciting event that causes the effusion. We think that our results reflect a cochlear toxicity induced by gastric content.
Conclusion
Transtympanicaly applied gastric content can induce in middle ear inflammation and decrease in cochlear reserve in 0.5 and 1 kHz frequencies. This paper is the first study to evaluate gastric content induced ototoxicity. Further studies needed to investigate if gastric content is ototoxic or not.Reference
1) Contencin P, Maurage C, Ployet MJ, Seid AB, Sinaasappel M. Gastroesophageal reflux and ENT disorders in childhood. Int J Pediatr Otolaryngol 1995;32(Suppl):135-44. [ Özet ]
2) Orenstein SR. Infantile reflux: different from adult reflux. Am J Med 1997;103:114-9 [ Özet ]
3) Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg 2002;127:32–35. [ Özet ]
4) Halstead LA. Role of gastroesophageal reflux in pediatric upper airway disorders. Otolaryngol Head Neck Surg 1999;120:208–214 [ Özet ]
5) Tasker A, Dettmar PW, Panetti M, Koufman JA, Birchall JP, Pearson JP. Reflux of gastric juice and glue ear in children. Lancet 2002;359:493 [ Özet ]
6) O'Reilly RC, He Z, Bloedon E, Papsin B, Lundy L, Bolling L, Soundar S, Cook S, Reilly JS, Schmidt R, Deutsch ES, Barth P, Mehta DI. The role of extraesophageal reflux in otitis media in infants and children. Laryngoscope 2008 ;118 : 1-9 [ Özet ]
7) Akdogan O, Ozkan S. Otoacoustic emissions in children with otitis media with effusion. Int J Pediatr Otorhinolaryngo. 2006 ;70:1941-4 [ Özet ]
8) Tas A, Yagiz R, Uzun C, Adali MK, Koten M, Tas M, Karasalihoglu AR. Effect of middle ear effusion on distortion product otoacoustic emission. Int J Pediatr Otorhinolaryngol 2004 ;68:437-40. [ Özet ]
9) Al-Saab F, Manoukian JJ, Al-Sabah B, Almot S, Nguyen LH, Tewfik TL, Daniel SJ, Schloss MD, Hamid QA. Linking laryngopharyngeal reflux to otitis media with effusion: pepsinogen study of adenoid tissue and middle ear fluid. J Otolaryngol Head Neck Surg. 2008 ;37:565-71. [ Özet ]
10) Heavner SB, Hardy SM, White DR, Prazma J, Pillsbury HC 3rd.Transient inflammation and dysfunction of the eustachian tube secondary to multiple exposures of simulated gastroesophageal refluxant. Ann Otol Rhinol Laryngol 2001 ;110:928-34. [ Özet ]
11) Bluestone CD. Pathogenesis of Otitis Media: Role of Eustachian Tube. Pediatr Infect Dis J 1996 ; 15: 281-91 [ Özet ]
12) Yeo SW, Park SN, Park YS, Suh BD. Effect of middle-ear effusion on otoacoustic emissions. J Laryngol Otol 2002 ;116:794-9. [ Özet ]
13) Yagiz R, Tas A, Uzun C, Adali MK, Koten M, Karasalihoglu AR. Effect of topically applied povidone-iodine on transient evoked otoacoustic emissions in guinea pigs. J Laryngol Otol 2003 ;117:700-3 [ Özet ]
14) Oghan F, Apuhan T, Yılmaz F. Ototoxicity caused by topical administration of gentamicin versus tobramycin in rabbits. Int J Pediatr Otorhinolaryngol 2011 ;75:915-8 [ Özet ]
15) Perez R, Freeman S, Sohmer H, Sichel JY. Vestibular and cochlear ototoxicity of topical antiseptics assessed by evoked potentials. Laryngoscope 2000 ;110:1522-7 [ Özet ]
16) Develioglu ON, Yilmaz M, Caglar E, Topak M, Kulekci M. Oto-toxic effect of gastric reflux. J Craniofac Surg. 2013, 24(2):640-4 [ Özet ]
17) Deppe C, Kummer P, Gürkov R, Olzowy B. Influence of the individual DPOAE growth behavior on DPOAE level variations caused by conductive hearing loss and elevated intracranial pressure. Ear Hear. 2013;34(1):122-31 [ Özet ]




