OCCULT LYMPH NODE METASTASIS FROM A THYROGLOSSAL DUCT CYST CARCINOMA: A CASE REPORT
2Devrek Devlet Hastanesi, Kulak Burun Boğaz Baş-Boyun Cerrahisi, Zonguldak, Türkiye
3Avicenna Hospital, Kulak Burun Boğaz Baş-Boyun Cerrahisi, İstanbul, Türkiye
4Erciş Devlet Hastanesi, Kulak Burun Boğaz Baş-Boyun Cerrahisi, Van, Türkiye
5Şişli Etfal Eğitim ve Araştırma Hastanesi, Patoloji Kliniği, İstanbul, Türkiye
Summary
Thyroglossal duct cysts (TGDC) are the most common congenital cystic masses of the neck. Malignancies arising from TGDC are quite uncommon, the prevalence of which has been reported to be 1%. TGDC carcinomas, which are usually diagnosed post-operatively, generally arise from the thyroid cells. The majority of TGDC carcinomas are papillary carcinomas. There are two opinions on the origin of TGDC carcinomas; one favors the thyroid itself while the other considers the TGDC as the origin of TGDC carcinomas. The treatment of TGDC carcinomas is controversial and the extent of the planned surgery depends on the risk group of the patient. A 44-year-old female presented to our clinic for evaluation of a painless, moderately solid mobile mass 5x6 cm in size located in the submental region in the mid-line of the neck. The mass was excised, and upon the diagnosis of papillary carcinoma in the thyroid tissue adjacent to a TGDC, she underwent a total thyroidectomy and selective neck dissection. This rare case is discussed in the light of the literature.Introduction
Thyroglossal duct cysts (TGDC), one of the most common lesions of the anterior neck[1], are the most common developmental disorders of the neck. TGDC are frequently observed at the subhyoid level and usually present with a painless swelling. TGDC carcinomas are quite rare and approximately 200 cases have been reported till today[2]. The risk of developing cancer in a TGDC is approximately 1% ;they are generally detected in adults in the perioperative period. Papillary carcinoma is the most common histological type of TGDC carcinomas (80%). As development of carcinoma in the cyst wall does not change the presentation, the diagnosis is based on the histological examination of the surgical specimen. It is controversial whether or not TGDC carcinomas arise from the thyroid tissue in TGDC or is a metastasis from an occult primary thyroid carcinoma. The optimal treatment of TGDC carcinomas is yet another controversial issue. Tumor excision, Sistrunk procedure, isthmusectomy, and/or total thyroidectomy may be preferred; elective lymph node dissection is not routinely performed. There is still no definite consensus on the treatment of lymph node metastasis, thyroid suppression therapy or radioactive iodine therapy[1-4]. We report herein a rare case of a TGDC carcinoma with lymph node metastasis in the light of the literature.Case Presentation
A 44-year-old female was admitted to the Otolaryngology Outpatient Clinic for evaluation of a swelling in the submandibular region. The patient reported that the swelling had increased in size over the last 2 years. Her physical examination revealed a painless mass 5x6 cm in size in the submental region in the mid-line of the neck. The tumor was mobile during swallowing and was moderately hard, with no pallor or rubor (Figure 1). On magnetic resonance imaging (MRI) of the neck, a mid-line cystic mass with the widest diameter approximately 5 cm was located at the infrahyoid level, and the mass contained an irregular solid component at the right postero-lateral aspect. (Figure 2). As the fine needle aspiration biopsy (FNAB) revealed cystic contents, the mass was excised. A mass, containing a cystic component, 5x4 cm in size, and a solid component at the right lateral aspect, 2x1.5 cm in size, was observed in the submental region. The solid component of the mass was attached to the hyoid bone. The duct arising from the cystic component of the mass was traced to its inferior. The solid component of the mass was removed by en bloc resection, over the hyoid bone (Figure 3). On macroscopic examination, the diameter of the solid component was 1 cm and the thickness of the wall of the cystic component was 0.3 cm. The pathological examination revealed a TGDC and a papillary carcinoma in the adjacent solid part (Figure 4,5). A post-operative ultrasound (US) examination showed an irregular, hypoechoic nodule 7.6x5.6 mm in size with indistinct micro-calcifications located at the junction of the left thyroid lobe and isthmus, and a spherical lymph node 5.5 mm in diameter in the cervical chain at the left lateral aspect of the neck, suspicious for malignancy. FNAB was performed on both lesions. Histopathological examination of the specimen from the thyroid nodule revealed atypical cells, suspicious for malignancy. No lymphocytes were observed in the cytological examination of the specimen obtained from the lymph node, thus the result was interpreted in favor of papillary carcinoma or papillary carcinoma metastasis. The patient underwent total thyroidectomy and left anterolateral neck dissection. The level 3 lymph node suspicious for malignancy was sent for frozen section evaluation, the result of which was reported as malignancy. On the histopathological examination, 3 foci of papillary carcinoma (0.6 cm, 0.4 cm, and 0.2 cm in diameter) were detected in the left thyroid lobe and a single foci (0.3 cm in diameter) was detected on the right lobe (multicentric; Figure 6). The neck dissection specimen was reported as reactive lymph nodes.
 Büyütmek İçin Tıklayın |
Figure 1: A mass approximately 5x6 cm in size in the midline submental region of the neck. |
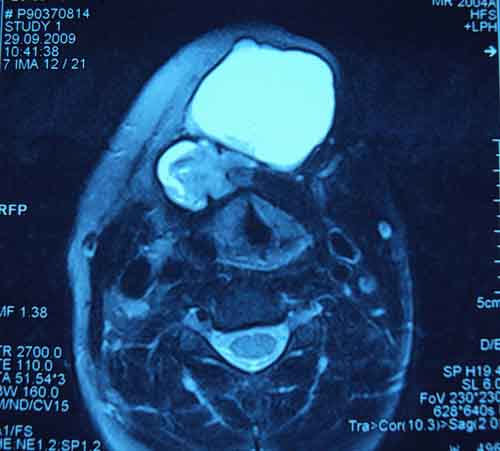 Büyütmek İçin Tıklayın |
Figure 2: Axial T2 MRI image; a cystic mass approximately 5 cm in the widest diameter located in the midline at the infrahyoid level, involving an irregular solid component in the postero-lateral aspect. |
 Büyütmek İçin Tıklayın |
Figure 3: The excision specimen of the thyroglossal duct cyst and the carcinoma. |
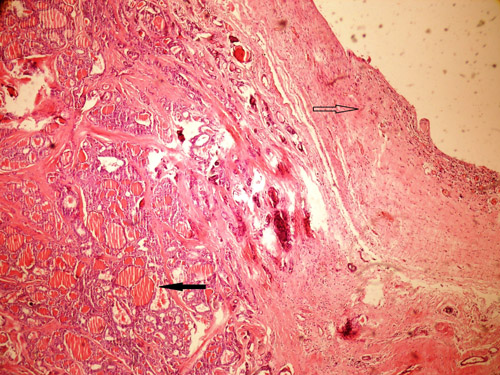 Büyütmek İçin Tıklayın |
Figure 4: Above presented is the epithelium of the cyst (empty arrow), and below is the thyroid tissue (black arrow; H&E x 40). |
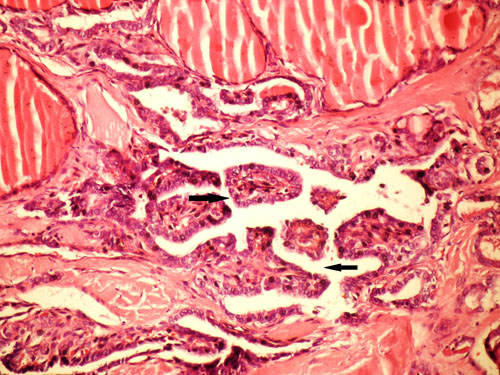 Büyütmek İçin Tıklayın |
Figure 5: The focus of papillary carcinoma in the thyroid tissue below the cyst (H&E x 400). |
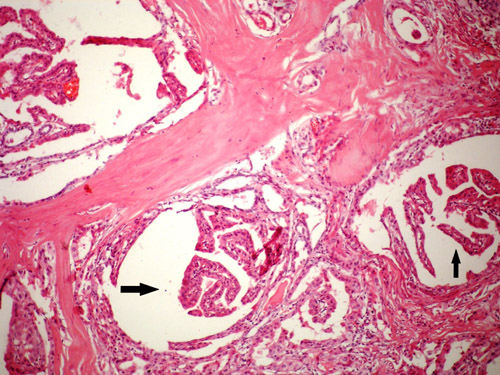 Büyütmek İçin Tıklayın |
Figure 6: The focus of papillary carcinoma in the thyroid tissue (H&E x 100). |
Discussion
Malignancies arising from TGDC are uncommon, with a prevalence of 1.3% of all TGDC[4,5]. The prevalence of TGDC carcinomas was reported to be 0.7% in 741 TGDC in a Mayo Clinic series[3], whereas LiVolsi et al.[2] reported 6 patients (1.5%) with TGDC carcinomas in a similar series of 377 cases. The first case of a TGDC carcinoma was reported in 1911 by Brentano[2]. Approximately 200 cases have been reported since that time[3]. Owing to the fact that the clinical presentation of TGDC carcinomas is generally not distinct from cases with benign TGDC, the diagnosis usually cannot be made until the post-operative histopathological examination; however, carcinoma must be considered in cases associated with solid, fixed, irregular lymphadenopathies. TGDC carcinomas are quite uncommon among children, they most commonly occur in females 40 years of age[1,2].Computed tomography (CT) or MRI should be considered for evaluating patients with suspected TGDC carcinomas[6]. CT scans may show findings that indicate TGDC carcinomas. These findings mainly include the presence of solid nodules within the cyst, calcifications, irregular borders, and the wall of the cyst being thicker than expected[1,2,7]. Calcifications in the cyst wall are in particular typical for papillary carcinomas[7]. As cancer incidence is low and as the rate of false positivity and false negativity is high, the value of performing FNAB in all cases with TGDC is low[1,2]; FNAB can only routinely be performed in adults considered to have TGDC[1,8].
As TGDC carcinomas are uncommon, they are usually diagnosed by the post-operative histopathological examination of the surgical specimen. Papillary carcinomas are the most common type (80%), followed by follicular, mixed, hurtle-cell, and squamous-cell carcinomas; medullary carcinomas has never been reported[1,2].
It is still unclear whether or not TGDC carcinomas arise from the aberrant thyroid tissue in the cyst wall or is a metastasis from an occult carcinoma of the thyroid gland[1,2]. The defenders of the first opinion suggest the risk for concomitant foci of carcinoma in the thyroid gland unlikely to be higher than the rate of presence of ectopic thyroid tissue in the cyst wall which is 60%[1,9]. Additionally, the fact that thyroid medullary carcinoma arising from the parafollicular C cells that originate from the ultimobranchial body has never been reported in TGDC, supports this opinion[1,2].
The Sistrunk procedure, in which the cyst and the hyoid bone are removed and the duct is traced from the base of the tongue to foramen cecum, is the minimal surgical procedure that can be performed for papillary thyroid carcinomas arising from TGDC[10].
Total thyroidectomy is not routinely recommended for TGDC carcinomas as it has no significant impact on the survival and lifelong thyroxine use is required after the operation[2,4]. The criteria for patients who are at high-risk for TGDC carcinoma and should be applied total thyroidectomy or more aggressive treatments are: > 45 years of age; history of radiotherapy; presence of a thyroid tumor on radiological examination; positive lymph nodes in clinical or radiological examination; a tumor diameter > 1.5 cm; cyst wall invasion on histopathological evaluation; and presence of positive surgical margins[1].
The prevalence of lymph node metastasis from papillary TGDC carcinomas has been reported to be between 7% and 15%; thus, routine selective lymph node dissection is not recommended[6,11]. Central neck dissection is routinely performed to assess the extension of the disease and to lower the likelihood of re-operation at the same site[4]. There is a consensus on performing selective neck dissection together with frozen section in the presence of suspicious lymph nodes[12].
No mass was palpated in the thyroid gland or in the neck of the patient presented herein. An ultrasound examination revealed a nodule < 1 cm in size with microcalcifications, which favored malignancy in the left lobe of the thyroid gland and a radiologically-suspicious lymph node < 1 cm in size in the mid-jugular chain on the left. The patient underwent total thyroidectomy and left anterolateral neck dissection. The frozen section of the suspicious lymph node revealed malignancy. The changes in the anterior compartment and the lateral cervical lymph nodes were reported as reactive hyperplasia in the postoperative pathological examination. The result was interpreted as metastasis in a single lymph node. Lateral lymph node metastasis without central lymph node involvement can occur, as in the present case. Hartl et al.[8] reported the prevalence of this type of metastasis as 40% in a series involving 18 patients. Such a high prevalence can be associated with the lymphatic drainage of the TGDC being primarily towards the lateral aspect of the thyroid gland along with the superior thyroid vessels.
Postoperative radioactive iodine and hormone suppression therapies can be applied in high risk patients in the presence of positive lymph nodes. As the patient presented herein was at high risk, suppressive therapy with levothyroxine was initiated following radioactive iodine therapy, at a dose of 150 mCi. There are no large-scale studies reporting the outcomes of these treatment modalities. Our patient is disease-free with no recurrence at 10 months follow-up.
Conclusion
TGDC carcinomas are quite uncommon tumors that account for 1% of TGDC, and should be considered in the preoperative differential diagnosis in adult patients pre-diagnosed with TGDC and have mid-line neck masses. The risk factors should be taken into consideration when planning the treatment.Reference
1) Kermani W, Belcadhi M, Abdelkefi M, Bouzouita K. Papillary carcinoma arising in a thyroglossal duct cyst: case report and discussion of management modalities. Eur Arch Otorhinolaryngol 2008; 265: 233-36 [ Özet ]
2) Motamed M, McGlashan JA. Thyroglossal duct carcinoma. Curr Opin Otolaryngol Head Neck Surg 2004; 12: 106-09 [ Özet ]
3) Heshmati HM, Fatourechi V, Van Heerden JA, et al. Thyroglossal duct carcinoma: report of 12 cases. Mayo Clin Proc 1997; 72: 315-1 [ Özet ]
4) Hartl DM, Ghuzlan AA, Chami L, Leboulleux S, Schlumberger M, Travagli JP. High Rate of Multifocality and Occult Lymph Node Metastases in Papillary Thyroid Carcinoma Arising in Thyroglossal duct cyst. Ann Surg Oncol 2009; 16: 2596-2601 [ Özet ]
5) Doshi SV, Cruz RM, Hilsinger RL. Thyroglossal duct carcinoma: a large case series. Ann Otol Rhinol Laryngol 2001; 110: 734-38 [ Özet ]
6) Kennedy TL, Whitaker M, Wadih G. Thyroglossal duct carcinoma: a rational approach to management. Laryngoscope 1998: 10; 1154-58 [ Özet ]
7) Branstetter BF, Weisman JL, Kennedy TL, Whitaker M. The CT appearance of thyroglossal dukt carcinoma. Am J Neuroradiol 2000: 2; 1547-50 [ Özet ]
8) Yang YJ, Haghir S, Wanamaker JR, et al. Diagnosis of papillary carcinoma in a thyroglossal duct cyst by fine-needle aspiration biopsy. Arch Pathol Lab Med 2000: 124; 139-42 [ Özet ]
9) Mazzaferri EL. Thyroid cancer in thyroglossal duct remnant: a diagnostic and therapeutic dilemma. Thyroid 2004: 14; 335-36 [ Özet ]
10) Shah JP, Loree TR, Dharker D, Strong EW, Begg C, Vlamis V. Prognostic factors in differantiated carcinoma of the thyroid gland. Am J Surg 1992;164: 658-61 [ Özet ]
11) Weiss SD, Orlich CC. Primarypapillary carcinoma of a thyroglossal duct cyst: report of a case and literature review. Br J Surg 1991; 78: 87-89 [ Özet ]
12) Luna-ortiz K, Hurtado-lopez LM, Valderrama-landaeta JL, Ruizvega A. Thyroglossal duct cyst with papillary carcinoma: what must be done? Thyroid 2004; 14: 363-66 [ Özet ]




