CASTLEMAN'S DISEASE AS A CAUSE OF CHRONIC DYSPNEA: CASE REPORT
2Atatürk Eğitim ve Araştırma Hastanesi, Patoloji Bölümü, Ankara, Türkiye
Summary
Castleman hastalığı, boyun bölgesinde kitle ile karşımıza çıkabilen bir hastalıktır. Castleman's diesase may cause neck mass. A patient complaining of chronic dyspnea had been treated with the presumptive diagnosis of bronchial asthma. However, her complaints did not subside after treatment. She applied to our clinic due to a mass in lower jugular region that was compressing the trachea. Fine needle aspiration biopsy was reported to be consisting of benign cytology. Complete excision of the mass was done under general anesthesia and the histopathologic assessment was consistent with Castleman's disease. Dyspnea was found to be almost totally relieved in the postoperative period. Castleman's disease may cause neck mass and result in various symptomatology due to compression of the surrounding structures.Introduction
Castleman's disease (CD) is a rare, benign lymphoproliferative disorder of unknown etiology[1]. It is also known as angiofollicular lymph node hyperplasia, angiomatous lymph node hamartoma, follicular lymphoreticuloma, and giant lymph node hyperplasia[1-4]. The lesions were classified into two types with respect to clinical and histopathological criteria: Hyaline vascular type constitutes 90% of cases and is usually asymptomatic, but occasionally it can result in symptoms due to mass effect on surrounding structures[5]. Plasma cell type comprises 10% of cases and exists as a fulminant multicentric disease with systemic symptoms[1]. Noninvasive methods usually do not suffice for diagnosis, therefore histopathological evaluation after complete excision is essential.In this case report, we present a case with a neck mass due to Castleman's disease, whose complaint of chronic dyspnea disappeared after compression over trachea by the mass was relieved.
Case Presentation
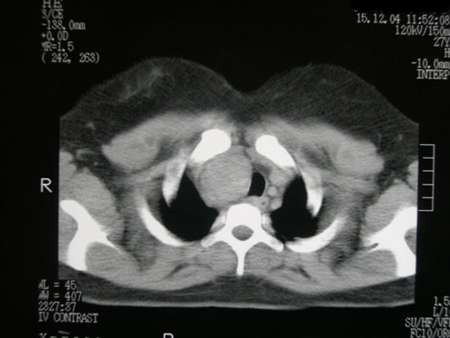
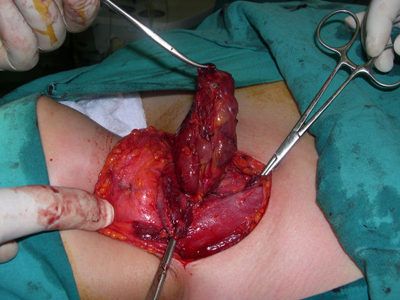
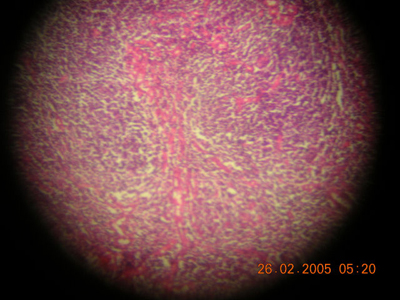
A 24-year-old female patient presented with a mass on right side of the neck for 3 months. She had recurrent expiratory dyspnea attacks and she was diagnosed to have bronchial asthma. There were no additional symptoms, nor there was a noteworthy data in her family history. The physical examination revealed a firm, mobile, and non-tender mass of 4X4 cm, in right lower jugular area just behind sternocleidomastoid muscle. The results of complete blood count and biochemistry panel were within normal limits. Computed tomography scans with contrast showed a well circumscribed lesion extending towards the mediastinum. The mass was compressing the trachea resulting in considerable decrease of lumen size (Figure 1). Fine needle aspiration biopsy revealed lymphoepithelial cells of benign character. The mass was totally excised under general anesthesia and the compression on trachea was relieved (Figure 2). Histopathological examination demonstrated a well-encapsulated lesion, with hyalinized follicular centers and prominent interfollicular vascular proliferation. The diagnosis was consistent with “hyaline vascular type Castleman's disease” (Figure 3). At one and a half years' follow-up, the patient remains free of disease and complaint of chronic dyspnea has totally disappeared.
 Büyütmek İçin Tıklayın |
Figure 1: The compression of the mass on the trachea results in the narrowing of lumen size. |
 Büyütmek İçin Tıklayın |
Figure 2: Complete excision of the mass resulting in relief of compression on trachea. |
 Büyütmek İçin Tıklayın |
Figure 3: Histopathological view of the lesion revealing hyalinized follicular centers and prominent interfollicular vascular proliferation, confirming the diagnosis of hyaline vascular type Castleman's disease (Hematoxyline-eosine X 100). |
Discussion
Castleman's disease (CD) is a benign tumor of lymphoid tissue of unknown etiology. It was considered to be a consequence of hamartomatous or inflammatory processes[6]. It may occur at any site wherever lymph nodes are located. The peak incidence is between 15-30 years of age, and the most common form of clinical presentation is an asymptomatic solitary mass[4]. There is no predilection for gender and race[2]. Our patient's age was consistent with peak incidence interval as well. Constitutional symptoms (fever, weight loss, arthralgia, etc.) and biochemical alterations (anemia, elevated erythrocyte sedimentation rate, and hypoalbuminemia) are reported to be associated with almost all cases of multicentric form and 50% of cases with plasma cell variant[6]. Our patient had previously been diagnosed to have bronchial asthma. Any possibility of a bronchial hyperreactivity cannot be denied, but the compressive effect over trachea and its contribution to resultant asthma-like symptomatology is noteworthy. After surgical excision, dyspnea symptom was almost totally relieved.The algorithm proposed by Casper in evaluation of patients suspected to have a neck mass due to CD is based on preoperative CT evaluation and complete excision[7,8]. CT scan is useful in distinguishing CD from thymoma and lymphoma[8].
Castleman's disease most commonly occurs in thorax (60%), head and neck region being the second most frequent site (14%)[2,8]. When confined to head and neck, it exists as an asymptomatic solitary mass as it was in our case[4]. A detailed investigation of neck, thorax and abdomen yielded no other disease foci in this patient. Our patient had hyaline vascular type of CD, in which the pathology is mostly diagnosed coincidentally.
Castleman's disease is thought to be a reactive lymphoid hyperplasia or a benign tumor. It is postulated that CD is induced by Human Herpes Virus-8 (Kaposi sarcoma-associated human herpes virus) infection or cytokines such as interleukin-6 and vascular endothelial growth factor[2]. However, further studies are necessary to unveil the underlying pathophysiological process.
Since appearance of CD in neither computerized tomography (CT) nor magnetic resonance imaging (MRI) is typical, histopathological examination stands to be the only definitive diagnostic tool[6].
Differential diagnosis of cervical lymph nodal enlargements include lymphoma, neurogenic tumor, hemangioma, thymoma, sarcoma and metastatic disease. Preperative radiographic studies and fine needle aspiration biopsy can aid in elimination of other entities[9]. On gross examination, CD is a well-circumscribed lesion without any sign for invasion of adjacent structures[2]. Hyaline vascular type of CD, as in our case, has an irregular shaped arrangement with atrophic nodal architecture surrounded by radially arranged capillaries penetrating the germinal centre of these follicles[2]. For unifocal lesions, complete excision is usually curative. However, any possible residual tissue must be carefully followed-up[6]. Even though, the only head and neck recurrence had been reported with plasma cell variant of CD in the literature[10], our patient is still under follow-up and there is no sign of recurrence up to now.
In conclusion, CD must be kept in mind in the differential diagnosis of solitary masses in head and neck region. Co-existing constitutional symptoms may ensource from compression of the surrounding structures and symptomatology can be vague. As a general rule, final diagnosis must be based on detailed and thorough examination rather than the symptom itself.
Reference
1) Frank DK, Charney D, Kashani A. Plasma cell variant of Castleman's disease occurring concurrently with Hodgkin's disease in the neck. Head Neck 2001; 23: 166-169. [ Özet ]
2) Samadi D, Hockstein NG, Tom LWC. Pediatric intraparotid Castleman's disease. Ann Otol Rhinol Laryngol 2003; 112: 813-816. [ Özet ]
3) Zim S, Doherty J, Ma Y, Lee E. Pathology quiz case. Castleman's disease (CD), unicentric, hyaline vascular type. Arch Otolaryngol Head Neck Surg 2001; 127: 1133-1135. [ Özet ]
4) Keller AR, Hochholzer L, Castleman B. Hyaline vascular and plasma cell types of giant lymph node hyperplasia of mediastinum and other locations. Cancer 1972; 29: 670-683. [ Özet ]
5) Arslan D, Ozturk F, Patiroglu T, Kucukaydin M, Gunduz Z. Castleman's disease. A case report. Turkish J Pediatr 1996; 38: 361-366. [ Özet ]
6) Rodrigo JP, Fernandez JA, Alvarez JC, Gomez J, Suarez C. Castleman's disease restricted to infratemporal fossa. J Laryngol Otol 1996; 110: 896-898. [ Özet ]
7) Casper C. The aetiology and management of castleman's disease at 50 years: translating pathophysiology to patient care. Br J Haematol 2005;129:3-17. [ Özet ]
8) Chen CC, Jiang RS, Chou G, Wang CP. Castleman's disease of the neck. J Chin Med Assoc 2007;70:556-558. [ Özet ]
9) Yuca K, Kosem M, Cankaya H, Kutluhan A, Kiris M. Castleman's disease arising in the cervical region: a case report. Hiroshima J Med Sci 2003; 52: 31-32. [ Özet ]
10) Sanz C, Sierra J, Cobarro J, Avellanda R, Monserrat E, Rozman C. An unusual case of Castleman's disease restricted to the neck. ORL J Otorhinolaryngol Rel Species 1992; 54: 331-333. [ Özet ]




