DESMOID TUMOR INVADING RESIDUAL THYROID TISSUE
2İzmir Atatürk Training and Research Hospital, Department of Pathology, İzmir, Turkey
Summary
Desmoid tumors (Fibromatosis) are rare soft tissue tumors whose etiology is not completely understood. Extraabdominal desmoid tumors involve mainly the extremities or the chest wall, hovewer, desmoid tumors invading residual thyroid tissue are very rare.These tumors are firm, rubbery, and have a remarkable tendency to infiltrate into surrounding structures. Although distant spread has not been documented in long-term follow-up studies, these tumors have a strong propensity to recur locally after resection. Wide radical resection with negative margins whenever possible has been considered essential to successful management. However, curative resection may be a challenge, particularly for recurrent tumors or those invading vital structures of the neck. Radiotherapy may be beneficial for tumor control in patients with unresectable tumors; those with positive margins after resection.
Our objective was to report a very rare form of this head and neck area located tumor invading residual thyroid tissue.
Introduction
Aggressive fibromatosis, also known as desmoid tumor, was first described by MacFarlane in 1832.[1] Desmoid tumors are not better understood because of their aggressive character and high recurrence rates despite benign histologic appearance.[2,3] Histologically, these tumors consist of spindle-shaped cells in a collagenous matrix and lack the pleomorphic, atypical, or hyperchromatic nuclei of malignancy. They exibit a character between fibroma and fibrosarcoma.[2] Desmoid tumors can be originated from any tissue in the body. Its incidence is 2.4-4.3 case/1 million patient/year and location is extraabdominal in 1/3 of the tumors.[4] Only 12-15% of all are located in head and neck region. In 40-85% of these cases, cervical region is affected.[5]Case Presentation
A 50 year old woman who underwent bilateral subtotal thyroidectomy due to nodular goitre in 2000 was interned with complaints of swelling in anterior cervical region and dyspnea in 2004. Physical examination showed a palpable rigid and fixed 5x5 cm mass deviating trachea to the left. All laboratory tests were normal. Ultrasound revealed a mass measuring 5x6 cm extending from right thyroid lobe to retrosternal region; and a mass measuring 1,5x2,5x2 cm related to residual thyroid mass in the left thyroid lobe. Thyroid scintigraphy showed nonhomogenous activity distribution and hypoactive multipl nodules, and the retrosternal extension of right residual thyroid lobe. Result of fine needle aspiration biopsy was considered doubtful. According to frozen section results, a fusiform cell tumor was thought during operation. The residual tissue on the left side was excised. The rigid residual tissue on the right side was seen to be fixed to trachea and invade carotid sheath. Recurrent and superior laryngeal nerves have not been identified clearly. So an incomplete resection was performed.Surgical specimen was stiff, solid, coloring gray to white, measuring 5x4.5x2 cm, and had fibrotic appereance as helical figures. Microscopic examination revealed that the tumor comprised cellular and fascicular structures consisted of uniform oval and fusiform cells on a collagenous ground (Figure 1). Nuclei had fine chromatin pattern and unsignificant nucleoli. No atypical mitosis was observed. Structures consisted of epithelial cells having focal uniform nuclei in a follicular arrangement were observed in samples taken from periphery of the material. Immunohistochemistry revealed diffuse cytoplasmic thyroglobulin, CEA, and cytokeratin 9/19 positivity. There were no ostrogen and progestrone receptor reactivity in tumoral fusiform cells. Consequently, the case was reported as fibromatosis invading residual thyroid tissue.
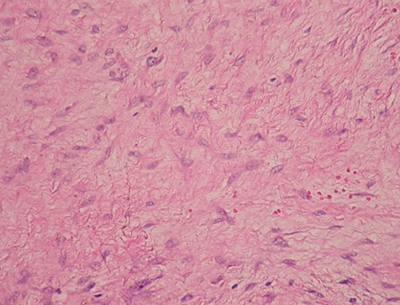 Büyütmek İçin Tıklayın |
Figure 1: Thyroglobulin positivity in epithelial cells in follicular arrangement at tumor periphery, H&E, X200. |
In early postoperative period, no complication developed. In 3rd postoperative month, CT showed a hypodense lesion having solid density, pushing trachea to the left, and measuring 5x4x4 cm in right thyroid lobe. In 5th postoperative month, CT revealed a mass extending from right paratracheal region to mediastinum, and measuring 7x5x5 cm in right throid lobe (Figure 2). The patient rejected another surgical procedure and were given radiotheraphy in a dose of 5000 cGy. After radiotherapy, no increase was detected in tumor size. The patient has been under control for 20 months.
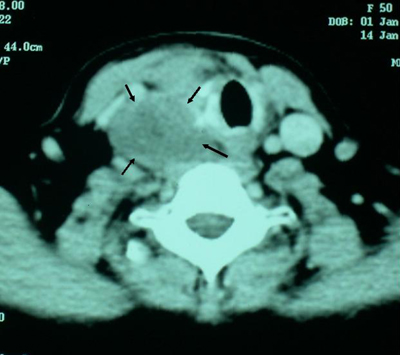 Büyütmek İçin Tıklayın |
Figure 2: CT imaging in 5th postoperative month |
Discussion
Desmoid tumors are primary located abdominally or intraabdominally.[6] Its incidence is 2.4-4.3 case/1 million patient/year and location is extraabdominal in 1/3 of the tumors[3]. Extraabdominal fibromatosis may occur in a variety of anatomic locations; retroperitoneally, chest wall and back, thign and head and neck.[7,8] Seven percent to 12% will occur in the head and neck region, of these, 85% will affect the neck. [9] Origin of extraabdominal fibromatosis from any thyroid tissue is now reported.Desmoid tumors are seperated from fibrosarcomas with their low mitosis and metastasis rates and cell counts.[3,4] The etiology of desmoid tumors could not be elucidated completely. While a history of previous insicion or blunt trauma were often recorded in these patients, it was thougt that this tumor arised from uncontrolled immature fibroblasts in the healing period. But the presence of the patients with no local trauma history made the validity of this hypothesis doubtful. [10] The high levels of oestrogen in these patients and regression of the tumor in postmenauposal period proposed a possible role for hormones in etiology.[2,10] Concurrence with Gardner syndrome and adenomatosis polyposis coli points the presence of chromosomal defects and inappropriate expression of certain genes. [4]
They grow very slowly and cause pain or motor deficits sometimes by pressure on adjacent tissues. [3] Pressure on vital structures big vessels or trachea can trigger life-threatining conditions. As in our case, fine needle aspiration is often non-diagnostic and preoperative diagnosis is made with core needle or open biopsy.
Desmoid tumors of the head and neck have a recurrence rate of 25% to 86%, with the highest percentage of recurrence in the supraclavicular and cervical region because of their neigbourhood with vital structures.[4,10] Since fibromatosis of the head and neck area is such a rarely reported event in the literature, no guidelines for theraphy have been defined clearly. Complete surgical excision is one that achieves negative, even if close, microscopic surgical margin remains the treatment of choice for most patients with desmoid tumors. Typically, these tumors lack pseudoencapsulation. Despite this, attempts have been made in a number of reports to define the optimal operative procedure by evaluating outcome according to the type of resection such as simple excision, local excision, wide excision, adequate resection, inadequate resection, radical local excision. Hovewer, several retrospective series in the literature suggest that the margin status following resection does not necessarily correlate with local disease recurrence.[3,5]
Treatments like radiotherapy, chemotherapy, steroids, antioestrogens, theophylline, nonsteroid anti-inflammatory drugs, vitamin C and castration were performed sporadically but could not be evaluated exactly.[3,4,10] Although radiotheraphy is often used today, there is no consensus in effectivity of radiotheraphy in cases with residual tissue or no negative surgical border. Radiation therapy may significantly decrease the volume of tumor but fails to eradicate this disease totally. Our patient were subjected to 5000 cGy radiotherapy and there was no major regression in residual tumor.
Our objective was to report on a case of a very rare form of this head and neck area located tumor invading residual thyroid tissue. Radiologic studies, including CT imaging, can fail to suggest local invasion. Surgery remains the treatment of choice. Radiation therapy could be of benefit.
Reference
1) Dalen BP, Bergh PM, Gunterberg BU. Desmoid tumors: a clinical review of 30 patients with more than 20 years' follow-up. Acta Orthop Scand 2003; 74: 455- 459. [ Özet ]
2) Lessow AS, Song P, Komısar A. Unusual fibromatosis of the head and neck. Otolaryngol Head Neck Surg. 2004 Mar;130(3):366-9. [ Özet ]
3) Collins BJ, Fischer AC, Tufaro AP. Desmoid tumors of the head and neck: a review. Ann Plast Surg 2005;54:103–108. [ Özet ]
4) Siegel NS, Bradford CR. Fibromatosis of the head and neck: a challenging lesion. Otolaryngol Head Neck Surg 2000;123:269-75. [ Özet ]
5) Hoos A, Lewis JJ, Urist MJ, Shaha AR, Hawkins WG, Shah JP, Brennan MF. Desmoid tumors of the head and neck: a clinical study of a rare entity. Head Neck. 2000;22:814. [ Özet ]
6) Fletcher CD: Myofibroblastic tumours: an update. Verh Dtsch Ges Pathol 1998; 82: 75- 82. [ Özet ]
7) Weiss SW, Goldblum JR. Fibromatosis. In: Weiss SW, Goldblum JR, eds. Enzinger and Weiss's soft tissue tumors. St Louis, Mo: Mosby Inc, 2001; 309-346.
8) Budzynski A, Wysocki A. Retroperitoneal desmoid tumor. Przegl Lek 1996; 53: 506- 507. [ Özet ]
9) Wilkins SA Jr, Waldron CA, Mathews WH, Droulias CA. Aggressive fibromatosis of the head and neck. Am J Surg 1975; 130: 412- 415. [ Özet ]
10) Abdelkader M, Riad M, Williams A. Aggressive fibromatosis of the head and neck (desmoid tumours). J Laryngol Otol 2001;115:772-6. [ Özet ]




