SUPRACLAVICULAR LYMPH NODE METASTASIS OF NONSEMINOMATOUS TESTICULAR CARCINOMA
2Ankara University Faculty of Medicine, Department of Pathology, Ankara, Türkiye
3Ankara University Faculty of Medicine, Department of Urology, Ankara, Türkiye
Summary
The patients with nonseminomatous testicular carcinoma generally undergo orchiectomy and cisplatin based chemotheraphy. If a residual or metastatic disease is noticed anywhere despite the therapy, it should be treated by definitive surgery in order to control the primary disease and to avoid fatal complications. When a metastasis to the cervical lymph nodes is encountered at the time of initial diagnosis or during the follow-up, head and neck surgeons rarely take part in the diagnosis and surgical treatment of testicular carcinoma,. In this study, we presented a case of nonseminomatous testicular carcinoma appearing as a left supraclavicular mass one year after chemotheraphy without evidence of residual disease in other sites. We also discussed the effectivity and safety of selective neck dissection for such a young patient with testicular carcinoma.Introduction
Supraclavicular lymph node metastasis from infradiaphragmatic malignancies generally indicates widespread disease that lost the chance of surgical treatment for cure, but testicular carcinoma represents an exception to this generalization.[1] Testicular carcinoma (seminomatous and nonseminomatous tumors) is the most common malignancy in men between 20-30 years of age.[2,3] Although the disease usually presents as a testicular mass or enlargement, abdominal, thoracal or cervical masses indicating metastatic disease may be noted during the follow-up.[1-3] Neck metastasis in the patients with testis cancer is an infrequent but, well established phenomenon and the incidence of neck metastasis in testicular carcinoma has been reported to be 4-5 %.[4-7]Testicular carcinoma often responds the combination of orchiectomy and chemotherapy. If residual or metastatic disease is noticed elsewhere after the therapy, it should be treated by definitive surgery in order to improve the survival and to reduce the risk of recurrence.[2,5] At this point, the head and neck surgeon plays role in the diagnosis and surgical treatment of residual neck disease. Since it is an oncologically safe procedure and effective for eliminating the possibility of residual neoplastic or teratomatous elements, neck dissection is accepted as a reliable treatment modality in such cases.[2,5]
The aim of this report is to present a case of nonseminomatous testicular carcinoma with supraclavicular metastasis, and to discuss the treatment of choice for residual neck disease in an adolesant.
Case Presentation
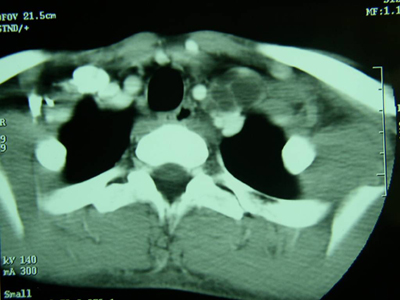
Sixteen year-old male presented with a 3-week history of a painless supraclavicular mass on the left side. According to his medical history, he had undergone orchiectomy one year ago. As the histologic examination of the testicle had demonstrated embryonal carcinoma, he had had four courses of chemotherapy consisting cisplatin, etoposite and bleomycine. Although all tumor markers had become negative after chemotheraphy, thoracoabdominal computerized tomography scanning has showed no regression of pre-existing retroperitoneal lymph nodes. Therefore, he had undergone retroperitoneal lymph node dissection in which histologic examination had demonstrated mature teratoma. Nine months after the lymph node dissection, he had noticed a mass on the left side of his neck while there was no evidence of infradiaphragmatic disease. Although fine needle aspiration did not demonstrate a positive result, uro-oncology tumor council accepted this supraclavicular mass as a metastasis of embryonal testicular carcinoma, and they recommended surgical treatment for this mass. Since the computerized tomography scanning depicted necrotic conglomerulate lymph nodes at inferior cervical region posterior to internal jugular vein and close to common carotid artery and apical pleura (Figure I), a selective neck dissection (level III-IV-V) was performed for the residual disease.
 Büyütmek İçin Tıklayın |
Figure 1: The necrotic and conglomerulate lymph nodes posterior to internal jugular vein and common carotid artery and superior to apical pleura on the CT scan of the neck. |
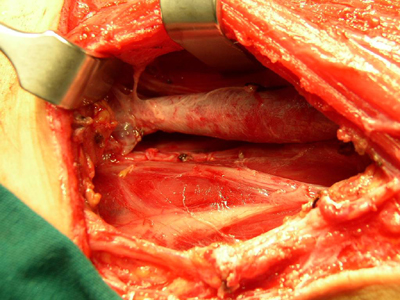
In this procedure, a low semi-apron incision extending from the ipsilateral Erb point to the suprasternal notch was used. The skin flap was elevated in the subplatysmal plane. The fascia of sternocleidomastoid muscle (SCM) was insized on the posterior border of the muscle and stripped over the muscle while SCM was retracted posterolaterally. The spinal accessory nerve was identified medial to the SCM and preserved. The mass with the dimensions of 5 x 9 cm was idendified posterior to the internal jugular vein. Dissection of the fascia was then continued over levator scapula and scalenus muscles and also over the internal jugular vein and carotid artery. During the procedure, the vagus, phrenic nerve and brachial plexus were carefully identified and preserved as well as the thoracic duct at the junction of internal jugular and subclavian veins (Figure II). As the tumor was extending inferiorly to innominate vessels and apical pleura, care has taken to avoid any damage to these nearby structures. Finally, all of the disease-involved adipo-lymphatic tissue of the supraclavicular fossa was removed by this selective neck dissection.
 Büyütmek İçin Tıklayın |
Figure 2: Intraoperative view of neurovascular structures, including internal jugular vein, thoracic duct, phrenic nerve and brachial plexus, around the tumor after selective neck dissection. |
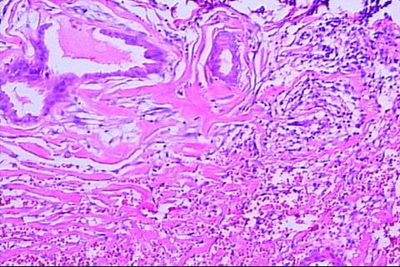
No complication was noticed during or after the surgical procedure. The histologic examination of the surgical specimen depicted mesenchymal differentiation in a fibrous stroma and it was reported as lymph nodes with metastasis of teratoma (Figure III). During 16-month follow-up, there was no evidence of recurrence anywhere and he was clinically free of disease.
 Büyütmek İçin Tıklayın |
Figure 3: Photomicrograph of the metastatic lymph node depicting mesenchymal differentiation in a fibrous stroma (Hematoxylin-eosin, x 200). |
Discussion
Supraclavicular masses are the most common presenting features of malignant diseases with no detectable primaries, and they generally indicate widespread diseases which is not amenable to surgical resection for cure. Testicular carcinoma represents an exception to this generalization when metastasizes to the neck, as it usually spreads through lymphatic pathways.[1-3] Initially, testicular carcinoma involves the retroperitoneal lymph nodes. The metastatic disease then spreads to the junction of internal jugular and subclavian veins via thoracic duct. From that location it may spread to cervical lymphatics. Testicular carcinoma which metastasizes to the neck most commonly presents as a Virchow's node.[3] Therefore, a young man presenting with a supraclavicular mass, especially on the left side, should be suspected for testis cancer.Testicular tumors are 96 % malignant and these are subdivided into seminomatous and nonseminomatous testicular carcinoma. Nonseminomatous testicular carcinomas are initially staged by physical examination, measurement of serologic tumor markers and computerized tomography scanning.[2,5] Majority of the cases of nonseminomatous testicular carcinoma are diagnosed at early stage. An evidence of metastasis above the diaphragm, usually in the thorax, indicates advanced disease which is relatively rare and has poor prognosis.[2,5] Nonseminomatous testicular carcinomas are treated by chemotherapy subsequent to orchiectomy. Aggressive chemotherapy can cause a histologic transformation leading the conversion of this lesion to a teratoma with scar and necrosis. Most likely, the chemotherapeutics selectively destroy the carcinomatous component leaving teratomatous remnants behind. In the majority of the cases, residual disease histologically consists of these teratomatous elements. Although teratoma is a nonmetastasizing form of testicular carcinoma, there is always some risk of eventual reversion of teratoma to its malignant counterpart. Therefore, surgical resection of the post-cheumotherapy residual disease is recommended to control the disease and to avoid fatal complications due to progressive local growth.[4-5]
After the diagnosis of nonseminomatous testicular carcinoma was established, our patient had been treated with chemotherapy following orchiectomy, and retroperitoneal lymph node dissection. He had noticed a left supraclavicular mass one year after chemotheraphy while there was no evidence of residual disease in other sites. The computerized tomography scanning of the cervical region depicted necrotic conglomerulate lymph nodes at supraclavicular fossa but fine needle aspiration did not demonstrate a positive result. Since the histologic examination of retroperitoneal disease has demonstrated mature teratoma, the urologist and the oncologist have accepted the supraclavicular mass as a cervical metastasis consisted of teratomatous elements.
We performed a selective neck dissection for this residual neck disease respecting the conclusion of uro-oncology council. In this procedure, the disesase-involved adipo-lymphatic tissue is removed by encompassing it in a packet formed by stripping the fascias over the muscles and neurovascular structures. This procedure provides excellent control of the neck disease by eliminating microscopic metastases.[8] Additionally, it is an effective procedure providing adequate exposure for the identification of neurovascular structures of the neck. Thus, the risk of damaging these structures is lower than simple resection of the mass and the morbidity is significantly less than those of radical neck dissection.[1,5]
It is unusual for the head and neck surgeon to perform neck dissection for the treatment of a metastatic neck disease with an infradiaphragmatic primary. It is also unusual to perform it for an adolescent. We consider that the selective neck dissection eliminates the micrometastasis and avoids neurovascular morbidity and deformity. Thus, we recommend selective neck dissection for cervical lymph node metastasis of testicular carcinoma to offer higher life standarts as well as oncologic safety for these young patients.
Reference
1) Zeph RD, Weisberg EC, Einhorn LH, Williams SD, Lingeman RE. Modified neck dissection for metastatic testicular carcinoma. Arch Otolaryngol 1985; 111: 667-672. [ Özet ]
2) Slevin NJ, James PD, Morgan DA. Germ cell tumors confined to the supraclavicular fossa: a report of two cases. Eur J Surg Oncol 1985; 11: 187-190. [ Özet ]
3) Wood A, Robson N, Tung K, Mead G. Patterns of supradiaphragmatic metastases in testicular germ cell tumors. Clin Radiol 1996; 52: 273-276. [ Özet ]
4) Weisberger EC, McBride LC. Modified neck dissection for metastatic nonseminomatous testicular carcinoma. Laryngoscope 1999; 109: 1241-1244. [ Özet ]
5) See WA, Laurenzo JF, Dreicer R, Hoffman HT. Incidence and management of testicular carcinoma metastatic to the neck. J Urol 1996; 155: 590-592. [ Özet ]
6) Akst LM, Discolo C, Dipasquale B, Greene D, Roberts J. Metastatic seminoma with cervical lymphadenopathy as the initial manifestation. Ear Nose Throat J 2004; 83: 356-359. [ Özet ]
7) Kilic G, Unal OF, Sungur A, Gursel B. Unusual presentation of choriocarcinoma metastasis to the neck. Otolaryngol Head Neck Surg 2003; 129: 297-299. [ Özet ]
8) Spiro RH, Strong EW, Shah JP. Classification of neck dissection: variations on a new theme. Am J Surg 1994; 168: 415-422. [ Özet ]




