TUBERCULOUS PAROTITIS: CAN BE LEFT SILENT FOR A LONG TIME?
2Ankara Numune Training and Research Hospital, Clinic of Patology, Ankara, Turkey
Summary
Tuberculous infection of the parotid gland is rare. A fifty-one-year-old woman presented with a history of 30 year swelling in preauricular region and a gradual increase in dimension at last year. Patient was suggested as parotid malignancy and underwent parotidectomy and mass excision. Pathological examination revealed a granulomatous infection. She was diagnosed as tuberculous parotitis by chest specialists and treated by anti-tuberculous-chemotherapy. Tuberculosis should be considered as part of the differential diagnosis of parotid masses.Introduction
Infections of parotid gland is common, tuberculosis of the parotid gland however is rare even in countries where the disease is endemic such as Africa and India. Tuberculous parotitis was first described in 1981 by Kuruvilla [1]. Tuberculous parotitis with pulmonary infections is seen more commonly, but primary type of isolated tuberculous parotitis is seen rarely [2].The disease involves the parenchyma of the gland, either through hematogenous spread or from infection of the lymph nodes secondary to a tonsillary or a dental infection within or around the parotid gland [3,4]. According to its ethiopathologic involvement route, the disease may present either as a result from infection of intracapsular or periglandular lymph nodes or as a diffuse gland growth because of parenchymatous tuberculosis [3]. Clinically it is presented as usually unilateral, slow growing parotid mass indistinguishable from a tumour.
In this case report, an interesting case of parotid tuberculosis simulating parotid neoplasm is presented.
Case Presentation
A 51 year-old woman admitted to our department with swelling in her right preauricular region which was present for 30 year. She had also 1-year history of same-sided infraauricular swelling. The mass wasn't painful. Neither had she complaints of night sweats, nor weight loss. There was history of hypertension and diabetes mellitus for 15 years. She gave no personal or family history of tuberculosis.In clinical examination, there was a soft, semi mobile, non-tender, circumscribed mass of 3x3x4 cm in size in the right preauricular area, which was non-fluctuant and non-erythematous. In addition to this mass, a 3x3x2 cm non-fluctuant swelling and a mass of 1 cm in diameter in the infraauricular region were detected. Both were smooth, firm and mobile. Intraoral examination was normal. No lymph nodes were palpable in the neck. Facial nerve functions were normal.
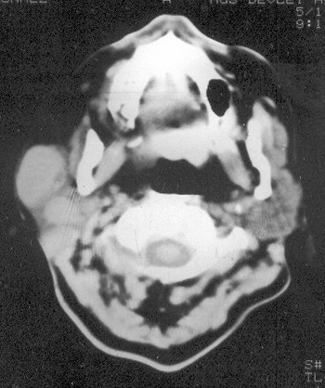
In laboratory investigation, white cell count was 10.9 x 109 /L. Erythrocyte sedimentation rate was 35mm/h. Biochemical investigations and two sided chest x-ray were normal. Thorax computed tomography (CT) was normal except pre-tracheal and precarinal lympadenopathies. Body temperature ranged between 36.2 and 37.5 C. Skin tuberculin test (Mantoux test) was positive with a weal of 17 mm, but since BCG was positive, skin tuberculin test was not found valuable. Triple repeated sputum specimen and gastric washing material showed no acid and alcohol resistant bacteria (AARB) staining. CT of the parotid and neck region showed a parotid mass of varying density and such nonhomogenous lesion with cystic areas of lower attenuation and two benign appearing masses that are not cavitated inferior to this lesion (Figure-1). Fine needle aspiration biopsy (FNAB) of the mass was negative for malignancy and granulomatous infection findings. No bacterial culture was carried out; since there was no abscess formation.
 Büyütmek İçin Tıklayın |
Figure 1: Computerized tomography of the parotid and neck region showing a parotid mass of varying density and such nonhomogenous lesion with cystic areas of lower attenuation and two benign appearing masses that are not cavitated inferior to this lesion |
 Büyütmek İçin Tıklayın |
Figure 2: Granulomas composed of epitheloid histocytes with central necrosis (X40, HE) |
 Büyütmek İçin Tıklayın |
Figure 3: Granulomatous infection of the lymph node, neighbouring parotid gland (X40, HE) |
Discussion
Although recent studies have shown that extra pulmonary tuberculosis is not uncommon, tuberculosis parotitis is still rare [1,4]. Patients usually present with diffuse, unilateral swelling of parotid gland of a long duration. Most of the related cases presented with slow growing masses increasing in size gradually during 2 to 6 months, and 1 case during a 10 years period [5,6]. Most cases were misdiagnosed as parotid tumours, with the diagnosis of mycobacterial infection only after parotidectomy and histopathologic examination [7].In this case, there is a history of 30 year swelling and gradually increase in dimension at last year. This increase in dimension had been considered as a carcinoma that had been developed secondary to a parotid adenoma. Together with different natures of the masses in palpation, although fine needle aspiration biopsy result was thought as granulomatous infection, these findings suggested us to surgical intervention.
FNAB; when used for the diagnosis of tuberculosis lesions has a sensitivity of 80% and has a specificity of 93% [8]. Since it is not pathognomonic in differentiating diagnosis of other granulomatous diseases and can be leading false positive results, no anti-tuberculosis chemotherapy is suggested in all time and surgical intervention is suggested especially malignancy is expected. FNAB causes false positive results especially in large and necrotic parotid neoplasms [9].
Tuberculouss parotitis can be classified into a ‘focal form' that spreads from a tuberculosis infection of the intraglandular or periglandular lymph nodes, and a ‘diffuse form' in which the parenchyma is involved diffusely [4]. The salivary gland register (1965-1981) contains only 2 cases of paranchymatous tuberculosis of the parotid gland. But contains 46 cases of intraglandular or periglandular lymph node involvement [10]. In this case parotid tuberculosis is of a focal form.
In this case, due to history of the patient, we considered, the mass was a carcinoma that was developed secondary to a parotid adenoma. 30-year history of swelling is considered as a very long duration for granulomatous infections of the gland. Clinical evaluation, negative thorax CT findings and negative AARB staining of sputum and gastric washing materials also supported our surgical decision in spite of FNAB result.
As a conclusion; tuberculous parotitis should be considered as part of the differential diagnosis of salivary gland masses. FNAB and Thorax CT are contributory to diagnosis. However, surgery is indicated for cases of malignancy suspicion.
Reference
1) Kuruvilla A, Saha NK, Barton RPE, Zardawi IM. Tuberculosis of the intraparotid lymph nodes. J Laryngol Otol. 1981; 95(11): 1165-7. [ Özet ]
2) Ustuner TE, Sensoz O, Kocer U. Primary tuberculosis of the parotid gland. Plastic and Recons Surg. 1991 Nov; 88(5): 884-5. [ Özet ]
3) Fabian RL. Salivary glands. In: Moris PF, Malt RA, ed. Oxford Textbook of Surgery. Vol 2. Oxford: Oxford Medical Publications. 1994; 2220-6.
4) Rowe-Jones JM, Vowles R, Leighton SE, Freedman AR. Diffuse tuberculosis parotitis. The J Laryngol Otol. December 1992; Vol.106: 1094-5. [ Özet ]
5) O'Connell J, George MK, Speculand B, Pahor AL. Mycobacterial infection of the parotid gland: An unusual cause of parotid swelling. J Laryngol Otol. 1993; 107: 561-4. [ Özet ]
6) Bhat NA, Stansbie JM. Tuberculous parotitis: A case report. J Laryngol Otol. 1996; 110: 976-7. [ Özet ]
7) Suoglu V, Erdamar B, Colhan I, Katircioglu OS, Cevikbas U. Tuberculosis of the parotid gland. J Laryngol Otol. 1998; 112: 588-91. [ Özet ]
8) Weiner GM, Pahor AL. Tuberculous parotitis: Limiting the role of surgery. J Laryngol Otol. Jan 1996; Vol 110: 96-97. [ Özet ]
9) Bhargava AK, Shenoy AM, Kumar RV, Nanjundappa, Rao CR. Parotid tuberculosis simulating malignancy. J Laryngol Otol. Oct 1999; Vol 113: 951-2. [ Özet ]
10) Holmes S, Gleeson MJ, Cawson RA. Mycobacterial disease of the parotid gland. Oral Surg Oral Med Oral Pathol Radiol Endod. Sep 2000; 90(3): 292-8. [ Özet ]




