GRADING FOR INTERORBITAL DISTANCE: DOES IT VARIATE IN SINONASAL PATHOLOGIES?
2Süleyman Demirel University Faculty of Medicine, Department of Radiology, Isparta, Turkey
Summary
Objective: Anatomic variations and configurations of ethmoid sinuses (along with dimensions) are very important for endoscopic sinus surgeon. The most dangerous complications of endoscopic sinus surgery are orbital and intracranial ones. The purpose of this study was to make a classification of interorbital distance and to determine whether it was altered by some sinonasal pathology.Materials and Methods: Five hundred fifty-four adult patients (321 Male, 233 female) underwent paranasal sinus computed tomography imaging for evaluation of either rhinological or orbital complaints were included in this study. The patients were classified as follows: patients with nasal polyposis (n= 75), patients with chronic rhinosinusitis (n= 192), patients without sinonasal disease (n= 287). Interorbital distance and Keros typing of all patients were measured from the same standard location of coronal computed tomography of paranasal sinuses.
Results: There was no statistically significant difference among three groups regarding to two types of classifications.
Conclusions: Computed tomography of paranasal sinus before endoscopic sinus surgery may give some clue about surgical difficulties in the region of the narrowest part of ethmoids (interorbital distance). This parameter has not been influenced from sinonasal pathologies such as nasal polyposis and chronic rhinosinusitis.
Introduction
Endoscopic intranasal interventions are popular approaches for the diagnosis and treatment of paranasal sinus disease. A major limitation of these techniques, however, is the potential for the surgeon to become spatially disoriented and thereby increase the risk of serious complications [1]. The literature regarding to the correlation between sinonasal complaints and CT scan evidence of paranasal sinus disease is controversial. However, CT scanning of the paranasal sinuses is the preferred mode of imaging for the purpose of diagnosis, disease monitoring, and surgical planning [2]. This modality guides us for the method of surgical intervention and makes us to avoid complications of endoscopic sinus surgery. Careful preoperative evaluation of computerized tomography (CT) scans is the gold standard for endoscopic sinus surgery. Nasal polyps may lead to expansion of nasal fossae and pressure atrophy of the adjacent bony wall of the sinonasal cavities [3]. This study was planned to investigate; i) by means of CT, to measure both the depth of ethmoidal roof and the IOD, ethmoido-nasal and ethmoido-orbital distances ii) to determine the effect of chronic rhinosinusitis and/or nasal polyposis on these measurements.Methods
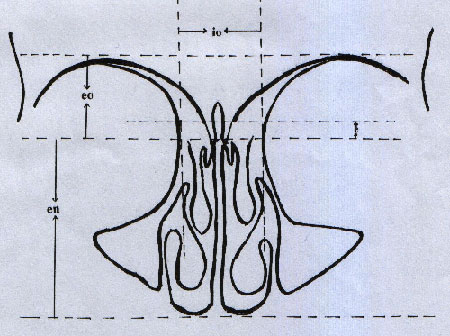
A retrospective analysis of paranasal sinus CT scans of 554 adult patients (321 Male, 233 female) between 18 and 76 years of age (mean age, 34.41 ± 13.24 years) was performed. The patients were evaluated in 3 groups; patients with nasal polyposis (NP), patients with chronic rhinosinusitis (CRS) and those without sinonasal disease. Patients with nasal polyps were defined from endoscopic nasal examination findings of records. All patients with radiologic sinonasal pathologies have been examined by nasal endoscopy. The patients with previous nasal or sinus surgery, sinonasal tumors and mucocele were excluded from the study. Patients with no complaint, or with complains of less than 3 months of duration, but demonstrating opacity on their CT images were also excluded from the study. CT evaluation of the paranasal sinuses was performed in the coronal projection without the administration of i.v. contrast material. Thin-section CT scanning (Philips, Tomoscan AVPS, Neitherland) was obtained with the following parameters; field of view, 160 mm; section thickness, 5 mm; index, 5 mm; 120 mA; 175 kV; small focal spot; mean total acquisition time, 5 minutes. One radiologist and one ENT specialist evaluated the entire paranasal sinus CTs.The measurement of the depth of ethmoid roof was carried out at the deepest part of it. The measurement of IOD was carried out at the slice on which the orbits were in largest diameter. The values of ethmoid roof measurement were scaled as Keros classification. IOD measurements were graded as follows: grade I-IOD ≤23 mm, grade II-IOD; 24-29 mm, grade III-IOD; ≥30 mm. The ethmoido-orbital distance (EOD) measurement was carried out from cribriform plate to the line connecting the most superior point of orbital roof. The ethmoido-nasal distance (END) measurement was carried from cribriform plate to the nasal floor (Fig.1).
 Büyütmek İçin Tıklayın |
Fig 1: The measurement of depth of ethmoid roof (e), interorbital distance (io), ethmoido-nasal distance (en) and ethmoido-orbital distance (eo). |
The nasal septal deviation angle, if present, was measured for each CT scan by the following method; the mean value of three consecutive coronal CT images at the level of the OMC was used for the calculation of the direction and degree of NSD. The superior insertion of the nasal septum at the level of the crista galli, its inferior insertion at the anterior nasal floor, and the apex of the NSD were all identified and clearly marked on the respective CT scan. The resultant angle was calculated using a standard protractor with the direction of the NSD noted. Three groups were compared regarding to the Keros (3 types) classification, IOD (3 grades), nasal septal deviation angle, ethmoido-orbital distance and ethmoido-nasal distance.
The SPSS statistical package was utilized for computation and performing the analysis, One-way ANOVA test was performed.
Results
The patients were classified as follows: patients with NP (n= 75), patients with CRS (n= 192), those without sinonasal disease (n= 287). NP group included 75 patients (47 male, 28 female) with mean age of 34.52 ± 12.20 years (range 19-73). CRS group included 192 patients (123 male, 69 female) with mean age of 33.80 ± 12.60 years (range 18-76). Control group (without sinonasal disease) included 287 patients (151 male, 136 female) with mean age of 34.49 ± 13.93 years (range 18-76) (Table 1). The mean depth of ethmoidal roof was 4.49 ± 1.18 mm (ranging from 2 mm to 10 mm) in NP group. The IOD was 26.29 ± 2.62 mm (ranging from 22 mm to 33 mm) in NP group. According to our classification the distributions of patients were as follows; grade I: 8 patients, grade II: 56 patients, grade III: 11 patients (Table 3). The mean depth of ethmoidal roof was 4.60 ± 1.18 mm (ranging from 2 mm to 10 mm) in chronic rhinosinusitis group. According to the Keros grading system the distributions of patients were as follows; Keros type I: 32 patients, Keros type II: 157 patients, Keros type III: 3 patients. The mean IOD was 25.81 ± 3.15 mm (ranging from 18 mm to 35 mm) in CRS group. According to our classification the distributions of patients were as follows; grade I: 38 patients, grade II: 131 patients, grade III: 23 patients (Table 3). The mean depth of ethmoidal roof was 4.66 ± 1.38 mm (ranging from 2 mm to 10 mm) in control group. According to the Keros grading system the distributions of patients were as follows; Keros type I: 55 patients, Keros type II: 222 patients, Keros type III: 10 patients. The IOD was 25.71 ± 2.62 mm (ranging from 18 mm to 32 mm) in control group. According to our classification for IOD the distributions of patients were as follows; grade I: 59 patients, grade II: 207 patients, grade III: 21 patients.Table 1: The general characteristics and the results of measurements of groups.
Table 2: Depth of ethmoid roof (Keros type classification) among three groups.
Table 3: The grading of groups regarding to the interorbital distance (IOD)
The mean EOD measurements were 12.28 ± 2.94 (ranging from 7 to 19 mm), 11.84 ± 3.16 (ranging from 5 to 20 mm), 11.93 ± 2.91 (ranging from 6 to 20 mm) in control, NP and CRS groups, respectively. The mean END measurements were 47.23 ± 4.51 (ranging from 32 to 60 mm), 48.29 ± 4.84 (ranging from 39 to 60 mm), 47.96 ± 4.78 (ranging from 30 to 60 mm) in control, NP and CRS groups, respectively.
There was no statistically significant difference among the three groups regarding to the Keros typing, IOD, END and EOD.
Discussion
Endoscopic sinus surgery necessitates an accurate evaluation of diseases and paranasal anatomic variations [4]. A major limitation of the endoscopic intranasal interventions is the potential for the surgeon to become spatially disoriented and thereby increase the risk of serious complications. Although the majority of reported complications are less serious, those that involve violation of the orbit or central nervous system may be devastating [5]. The anatomy of this area gained more and more significance as the endoscopic sinus surgery develops further. In contrast to the medial wall of the nasal cavity, the anatomy of the lateral nasal wall is complicated [5]. The area between nasal septum and lateral nasal wall is the area in which the sinus surgeon deals with. The more the volume of this area is, the easier the manipulation will be. We have investigated the height and width of this anatomic region by measuring the depth of ethmoidal roof and IOD.There are some morphometric studies of paranasal structures. The most important morphometric study is Keros classification. This indicates 3 types of relation between cribriform plate and ethmoid roof [6-8]. The most dangerous of them is the type III for the suregeon because of the likelihood of a perforation through the lateral lamella of the lamina cribrosa. Fernandez et al [9]. found that the greater volume of maxillary sinus in chronic rhinosinusitis patients when compared to others, and they correlate this finding to the osteolytic effect of the inflammatory process in the sinus bone. In our study we found no significant alteration in the dimensions of IOD, EOD, END and Keros type classification by any effect of nasal polyp and/or chronic rhinosinusitis.
The literature regarding correlation between sinonasal complaints and CT scan evidence of paranasal sinus disease is controversial. However, CT scanning of the paranasal sinuses is the preferred mode of imaging for the purpose of diagnosis, disease monitoring, and surgical planning [2]. Grading of IOD with Keros type classification makes the surgeon evaluates the access of surgical intervention. Grade III is the easiest candidates for endoscopic sinus surgery. It is difficult to operate patients with grade I (IOD) and with Keros type III. Although IOD are slightly wider in NP groups than the control and chronic rhinosinusitis groups, there was no statistically significant difference among three groups regarding to both types of classification.
Conclusion
In adult patients, IOD together with ethmoid roof have not been influenced from sinonasal pathologies such as NP and CRS. However, they should be evaluated before any endoscopic sinus intervention due to feasibility of surgical access. The high-risk group of patient for endoscopic sinus surgery (especially for orbital complications) may be determined preoperatively by index of IOD. Grade I IOD is the most dangerous for surgeon because of close relationship with orbital wall and orbits. To evaluate the effect of these pathologies on sinonasal development, a prospective study can be made involving pediatric patients.Reference
1) Ferrie JC, Azais O, Vandermareq P, Klossek JM, Drouineau J, Gasquet C. X-Ray computed tomographic study of the ethmoid and middle meatus. II. Radioanatomy (axial incidence) and morphological variations. J Radiol 1991;72:477-87. [ Özet ]
2) Kenny TJ, Duncavage J, Bracikowski J, Yildirim A, Murray JJ, Tanner SB. Prospective analysis of sinus symptoms and correlation with paranasal computed tomography scan. Otolaryngol Head Neck Surg 2001;125:40-4. [ Özet ]
3) Mafee MF, Carter BL. Nasal cavity and paranasal sinuses. In: Valvassori GE, Mafee MF, Carter BL. Imaging of the Head and Neck. New York, Thieme Medical Publishers Inc; 1995:289.
4) Sanchez Fernandez JM, Anta Escuredo JA, Sanchez Del Rey A, Santaolalla Montoya F. Morphometric study of the paranasal sinuses in normal and pathological conditions. Acta Otolaryngol. 2000;120(2):273-8. [ Özet ].
5) Streitmann M.J, Otto R.A, Sakai C.S. Anatomic considerations in complications of endoscopic and intranasal sinus surgery. Ann Otol Rhinol Laryngol 1994;103:105-9. 6) Bingham B, Wang RG, Hawke M, Kwok P. The embryonic development of the lateral nasal wall from 8 to 24 weeks. Laryngoscope 1991;101:992-7. [ Özet ]
7) Arslan H, Aydinlioglu A, Bozkurt M, Egeli E. Anatomic variations of the paranasal sinuses: CT examinations for endoscopic sinus surgery. Auris Nasus Larynx. 1999;26:39-48. [ Özet ]
8) Meloni F, Mini R, Rovasio S, Stomeo F, Teatini GP. Anatomic variations of surgical importance in ethmoid labyrinth and sphenoid sinus. A study of radiological anatomy. Surg Radiol Anat 1992;14:65-70. [ Özet ]
9) Anderhuber W, Walch C, Fock C. Configuration of ethmoid roof in children 0-14 years of age. Laryngorhinootologie. 2001;80(9):509-11. [ Özet ].




