JUVENILE NASOPHARYNGEAL ANGIOFIBROMA: RADIOLOGIC EVALUATION AND PRE-OPERATIVE EMBOLIZATION
2Cumhuriyet University Faculty of Medicine, Department of Otorhinolaryngology, Sivas, Turkey
Summary
Juvenile nasopharyngeal angiofibroma (JNA) constitutes less than 0.5% of all head and neck neoplasms. It is a histopathologically benign, yet locally agressive, vascular tumor that occurs most frequently in males from 5 to 25 years. Advances in imaging and treatment techniques are now facilitated more accurate staging of this disease. In this study, we present a case of JNA, to whom pre-operative embolization is administered.Introduction
JNA, as its suggests, is a combined vascular and fibrous neoplasm arising in the nasopharynx of prepubertal and adolescent males. The tumor exhibits a strong tendency to bleed and, despite being microscopically benign, frequently exhibits destructive and agressive behaviour.[1] In diagnostics, besides epypharyngoscopy, computed tomography (CT), magnetic resonance imaging (MRI) are the primary diagnostic tests.[2] Angiography is used for pre-operative embolization. In this case report, we aimed to demonstrate a case of JNA, to whom pre-operative embolization is administered, associated with CT, MRI and angiography.Case Presentation
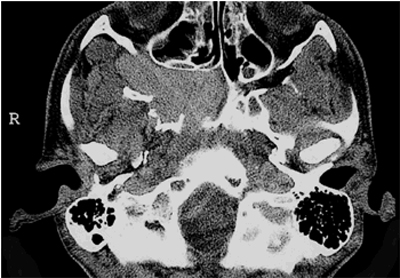
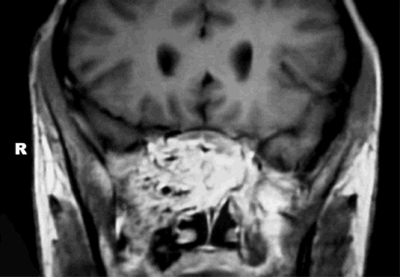
A 17-year-old boy, admitting to the hospital with intermittent right-sided epistaxis of spontaneous onset and vertigo, was examined with CT, MRI, and conventional catheter angiography. On examination the patient had a large fleshy mass completely filling the nasopharynx. There were no associated otologic complaints, generalized bleeding tendency, or loss of appetite or weight. Cranial nerves were all intact. Other physical and laboratory examination findings were normal. To elucidate the underlying pathologic abnormality, CT images at 2- and 4-mm increments obtained in the axial and coronal planes before and after contrast medium injection. CT scan confirmed a well-defined mass in the right post-nasal space, projecting into right sphenoid sinus and nasopharynx, with strong contrast enhancement (Fig. 1). Minimal bone erosion and remodeling were noted at the level of the skull base, suggesting that the lesion was a slow growing tumor. The MRI protocol included axial, sagittal and coronal planes in T1- (repetition time [TR] / echo time [TE] = 440msec/15msec) and T2- (TR/TE = 4000msec/100msec) weighted sequences. Gd-DTPA was used as a contrast agent at MRI. The lesion was characterized as a contrast enhancing mass within the nasopharynx on MRI (Fig. 2). Given these findings, the differential diagnoses included the tumors of the vascular origin.
 Büyütmek İçin Tıklayın |
Figure 1: Contrast-enhanced axial CT image: Tumor extends from the right pterygopalatine fossa into nasopharynx and continuing into sphenoid sinus on the right side. |
 Büyütmek İçin Tıklayın |
Figure 2: MRI scan: Gd-enhanced T1-weighted SE coronal image demonstrates a large, intensely enhancing nasal mass extending into the nasopharynx. |
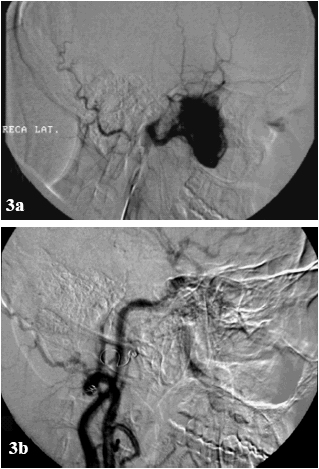
In our case, angiographic examination and embolization were performed during the same session. Superselective angiography demonstrated the feeding vessels from the right internal maxillary artery (IMA), and a smaller feeding vessel from the right internal carotid system. The embolization was performed under fluoroscopic control using digital substraction angiography (DSA), which gives an excellent image quality. Embolization of the feeding vessel from the external carotid system using polyvinyl alcohol (PVA) particles 500–710 µm (Contour embolization particles, Boston Scientific, USA) in size for good tumor penetration and three fibered platinum coils (4mm/20mm Target Therapeutics, Boston Scientific, USA) were performed, without complication, in order to reduce bleeding at the time of operation. Post-embolization angiogram revealed significant tumor blush reduction. There was residual blood flow from the branches of the right ophtalmic artery. Branches arising from the internal carotid or ophthalmic arteries were not embolized. Figure–3 shows the arteriogram before (Fig. 3(a)) and after (Fig. 3(b)) embolization of the feeding vessels. The patient underwent resection of tumor through a right lateral rhinotomy and partial medial maxillectomy on the next day. The histopathologic features were consistent with an angiofibroma. The patient was followed with 1-month interval for the first 6-month; and then with 3-month interval for two years; and 1-year interval thereafter. The patient was followed over 2 years without recurrence or residual tumor.
 Büyütmek İçin Tıklayın |
Figure 3: Pre-operative carotid angiogram. (a) Pre-embolization carotid angiogram revealing a vascular blush in the right nasal fossa. The vessel feeding the tumor is the internal maxillary artery, (b) Post-embolization angiogram shows significant blush reduction. |
Discussion
Hippocrates described the tumor in the 5th century BC, but Friedberg first used the term angiofibroma in 1940.[3] Angiofibromas are histopathologically benign but potentially locally destructive vascular tumors. They are unencapsulated neoplasms composed of a rich vascular network within a fibrous stroma.[4] Angiofibromas originate predominantly in the posterior-lateral wall of the nasopharynx. Angiofibromas arise typically in the nasopharynx, specifically at the trifurcation of the sphenoidal process of the palatine bone, the horizontal ala of the vomer, and the roof of the pterygoid process. These vascular tumors expand commonly beyond the nasopharynx into the cranium, nose, and paranasal sinuses.[4,5] JNAs are age- and sex-linked. Classically, they are confined to boys in adolescence and early adulthood.[6] JNA accounts for less than 0.5% of all benign lesions that originate in the nasopharynx. JNA is an uncommon tumor, with reported incidence between 1 in 5000 and 1 in 60,000 otolaryngology patients. Despite this low incidence, JNA is the most common benign tumor originating in the nasopharynx of young males. The etiology of JNA is unknown but it is postulated that there may be a relation to sex hormones. There is evidence of increased androgen receptors of tumors and successful tumor regression after anti-androgen therapy.[7]Diagnostic imaging should be performed prior to an invasive procedure since it may suggest the diagnosis, thereby reducing the risk of catastrophic hemorrhage associated with biopsy.
In a study of 72 patients, Lloyd et al.7 reported three findings on CT and MR imaging that should suggest a diagnosis of JNA:
1 - a soft tissue mass in the nasopharynx or nasal cavity,
2 - a mass in the pterygopalatine fossa,
3 - erosion of posterior osseous margin of the sphenopalatine foramen extending to the base of the medial pterygoid plate. In our case, the lesion was located in the nasopharynx, and projected into the right sphenoid sinus.
Angiofibroma can be diagnosed using CT, MR imaging and angiography. CT is a most important pre-operative test because it is useful for showing the destruction of bony structures and widening of foramen and fissures at the skull base due to spread of tumor. CT can also help recognize invasion of sphenoid and thus determine the aggressiveness of surgery. On CT, bone involvement and tumoral spread can be seen best on thin-section axial or coronal images.
MRI is useful to show presence of intracranial extension of the tumor. MRI also helps discern between sinus invasion, obstruction and retention of secretions. On MR imaging, JNA appears as a heterogenous mass with signal voids (representing hypertrophic tumor vessels) that are consistent with the highly vascular tumor; intense enhancement with gadopentetate contrast material is typical.[3,4] In this case, bone involvement is demonstrated best on CT. Selective angiography identifies the feeding vessels and allows the option of pre-operative embolization for vascular control.[8] This imaging method shows the size and site of the lesion as well as size and location of the feeding vessel. The arterial supply to JNAs is primarly from distal IMA branches, commonly the sphenopalatine, descending palatine, and posterior superior alveolar branches. The ascending pharyngeal artery not infrequently supplies JNAs.[9] As it grows, the tumor may parasitize bilateral arterial supply from any nearby vessel. Therefore, bilateral internal and external carotid arteriography is indicated in most patients. In our case, the lesion was mainly fed by a branch of the IMA. Surgical resection of JNAs is difficult because of abundant tumor vasculature; moreover, incomplete resection not infrequently results in tumor recurrence.[10] Preoperatively tumor embolization can greatly facilitate surgery. In JNA, superselective embolization of feeding vessels arising from the external carotid artery is highly effective and safe. Anastomosis between branches of the external and internal carotid artery and vascular spasm have to be considered when planning superselective embolization. Several materials have been tried over the years, including non-absorbable silastic spheres, Gelfoam, dura mater, and polyvinyl alcohol particles.[11] Recently, non-absorbable polyvinyl alcohol particles are preferred.[12] Migration of embolization particles to the ophthalmic artery, the cerebral or vertebral arteries via anastomosis or reflux of particles applied to the external carotid artery may cause severe ischemic deficits. In our case, the IMA was embolized with 500–710 µm PVA particles followed by three platinum coils proximally to prevent recanalization.
In JNA cases, spontaneous regression is rare. Recurrence rates ranged from 6% to 60% . Recurrence can occur as early as 3–4 months after surgery.[13]
The differential diagnosis of JNA includes antrochoanal polyp, inflammatory sinonasal polyp, neurofibroma, adenoidal hypertrophy, nasopharyngeal cyst, pyogenic granuloma, chordoma, and malignant neoplasms, such as nasopharyngeal carcinoma, lymphoma, or rhabdomyosarcoma.[3,13] CT and MR imaging of nasopharyngeal carcinoma show an inhomogeneous mass arising from the nasopharyngeal mucosa or submucosal space with skull-base erosion or intracranial extension. Lymphoma may arise from adenoidal tissues of the nasopharynx or Waldeyer’s ring and can be associated with lymphadenopathy. Imaging of rhabdomyosarcoma reveals a soft-tissue mass with frequent bone destruction and mild enhancement on CT, but marked enhancement on MR imaging.[14]
In conclusion, JNA should be suspected in a boy or adolescent male with a history of chronic nasal obstruction or recurrent epistaxis without history of trauma and a soft tissue mass in the nose or nasopharynx. Preoperative angiography is mandatory for identification of the feeding vessels in view of preoperative embolization before surgery in all cases.
Reference
1) Shaheen OH. Angiofibroma. In: Hibbert J, Kerr AG, eds. Scott-Brown’s Otolaryngology. Volume 5, 6th ed. Bath, Great Britain: Reed Educational and Professional Publishing Ltd. 1997.
2) Arslan H, Bozkurt M, Sakarya ME, et al. Power Doppler findings in nasopharyngeal angiofibroma. Clin Imag 1998; 22: 86–88. [ Özet ]
3) Tewfik T. Juvenile nasopharyngeal angiofibroma. http//:www.emedicine.com/2003
4) Huang RY, Damrose EJ, Blackwell KE, et al. Extranasopharyngeal angiofibroma. Int J Pediatr Otorhinolaryngol 2000; 54: 59–64. [ Özet ]
5) Specter JG. Management of juvenile angiofibroma. Laryngoscope 1988; 98: 1016–1026. [ Özet ]
6) Choremis J, Frenkiel S. Juvenile nasopharyngeal angiofibroma in a 16 year-old male: diagnosis and surgical treatment. McGill Journal of Medicine (MJM) 1998; 4: 22–27.
7) Lloyd G, Howard D, Phelps P, et al. Juvenile angiofibroma: The lessons of 20 years of modern imaging. J Laryngol Otol 1999; 113: 127–134. [ Özet ]
8) Lim IR, Pang YT, Soh K. Juvenile angiofibroma: case report and the role of endoscopic resection. Singapore Med J 2002; 43(4): 208–210. [ Özet ]
9) Pile-Spellman J. Endovascular therapeutic neuroradiology. In: Taveras JM. Neuroradiology. 3rd ed. Williams&Wilkins. Baltimore 1996.
10) Davis KR. Embolization of epistaxis and juvenile nasopharyngeal angiofibromas. AJR 1987; 148: 209–218. [ Özet ]
11) Koç C, Özdem C, Arıkan OK, Beriat K. Clinical value of pre-operative polyvinyl alcohol embolization in juvenile nasopharyngeal angiofibroma. Turk Arch Otolaryngol 2001; 39: 267–272 (in Turkish).
12) Antonelli AR, Cappiello J, DiLorenzo D, Donajo CA, Nicolai P, Orlandini A. Diagnosis, staging, and treatment of juvenile nasopharyngeal angiofibroma. Laryngoscope 1987; 97: 1319–1325. [ Özet ]
13) Durden DD. Skull Base tumor Surgery. Radiology of skull base neoplasms. Otolaryngol Clin North Am 2001; 34: 1043–1064. [ Özet ]
14) Som PM, Curtin HD. Head and Neck Imaging. St. Louis, Mosby, 2003.




