THE INVESTIGATION OF THE ROLE OF C3-C4 COMPONENTS OF THE COMPLEMENT SYSTEM IN OME
2KSU, Mikrobiyoloji, Kahramanmaraş, Türkiye
Summary
Objective: Otitis media with effusion (OME), a common disease in childhood, is characterized by chronic inflammation in which the proinflammatory activity of the complement (C) system is postulated to be one of the causative factors. The aim of this study was to investigate whether complement system has a role in the pathogenesis of OME or not.Methods: The study included 16 patients with OME, 8 patients with acute otitis media (AOM) and 16 healthy controls. Blood samples were collected from all subjects, while middle ear fluid samples were obtained only from AOM and OME group. C3 and C4 levels in serum and middle ear effusions were determined.
Results: The C3 and C4 levels in the serum of the patients with AOM were significantly higher than those of the patients with OME and normal controls. The presence of C3 and C4 in the middle ear effusions of the patients with OME and AOM was shown, but C3 and C4 levels were significantly lower in middle ear effusions than in serum of the same patients.
Conclusion: The present study showed that C3 and C4 components of the complement system are present in the middle ear effusions of the patients with OME. These components may have a role in the development, maintenance or the chronicity of the disease but further studies are needed to elucidate the role of complement system in OME.
Introduction
Otitis media with effusion (OME), a common disease in childhood, is characterized by fluid accumulation in the middle ear behind an intact tympanic membrane without signs and symptoms of acute infection [1]. OME has been considered as a multifactorial disease since various factors like eustachian tube dysfunction, impairment of middle ear clearence system and ventilation, upper respiratory tract infections, anatomic abnormalities, bacteria, viruses, and various inflamatory mediators have been implicated in the etiopathogenesis of this disease. The contribution of immune mechanisms in the etiology of the diseases with multifactorial origin like OME is very likely. Local and/or systemic immunological disturbances as well as the aforementioned factors may contribute to the etiopathogenesis of chronic OME.The complement system comprises a group of more than 30 serum and cell surface proteins that interact with other immune system molecules and with each other in a highly regulated manner to provide many of the effector functions of humoral immunity and inflammation [2]. This system is activated via either the classical pathway, which is one of the major effector mechanisms of humoral immunity, or the alternative pathway which is a mechanism of innate immunity [2]. The classical pathway consist of C1, C4 and C2 proteins and is activated by antigen-antibody complex (IgM and IgG1,2,3), polynucleotides, C-reactive protein, viruses, plasmine, etc. [2]. The alternative pathway consists of properdin, C3, Factor B and D proteins, and is activated by microbial polysaccharides and lipopolysaccharides, insulin, IgG4, IgE, IgA, etc.[2]. The complement system has a number of important properties that enable it to operate efficiently in host defense against microorganisms without injuring normal tissues. Deficiencies in certain complement components are associated with some infections and autoimmune diseases [2]. Nevertheless, the complement system sometimes may lead to significant tissue damage even when it is appropriately activated and properly regulated.
The presence in middle ear fluid of B- and T- lymphocyte, macrophage, polimorphonuclear leukocyte, IgA, IgE, IgG, IgM, lysozyme, immune complex, rheumatoid factor, antinuclear antigen and bacteria was shown [3-10]. It can be expected that complement activation via either the classical pathway or the alternative pathway may occur, or at least it plays a role in some stages of this chronic process.
In the present study, we aimed at investigating the role of complement system on OME.
Methods
This study was prospectively undertaken on 16 patients with OME, 8 patients with AOM and 16 healthy children. The study was approved by the local ethics committee, and informed consent was obtained from the parents or guardians.OME group included 10 male and 6 female patients. AOM group consisted of 5 male and 3 female. All of the patients with OME suffered from hearing loss and all of those with AOM presented with earache. During the 2 months follow-up of the 16 patients with OME that did not respond to antibiotic therapy, 14 had bilateral and 2 had unilateral OME on otoscopic examination. Audiologic evaluation (Interacoustics AC 40, Denmark) revealed conductive hearing loss in all patients with a pure tone average of 27.5 dB. Tympanometric measurements (interacoustics AZ 26, Denmark) showed type B tympanogram in 26 ears, type C in 4 ears and type A in two ears. Of the 8 patients with AOM, 3 presented with right earache and 5 left earache. In otoscopic examination of these patients, hyperemia and bulging were seen in tympanic membrane but there was no spontaneous perforation or supuration. Other ears were normal. The control group included 10 male and 6 female children, who were questioned about any sign of upper respiratory tract infection or middle ear infection. Otoscopic and other otorhinolaryngologic examinations were normal. The normality of the ears of the control group was tested by using tympanometry and audiometry. Type A tympanograms were obtained in all. The mean ages of the subjects were 8,0±5,4 years for EOM, 9,4±1,3 years for AOM and 8,2±2,6 years for healthy controls.
Venous blood samples of the patients with OME were taken 5-6 days before operation for routine preoperative investigations and those of the patients with AOM were obtained before paracentesis. Venous blood samples of the control group were obtained from the healthy subjects who admitted to the hospital for circumcision or screening for vaccination. These healthy subjects did not have any signs or symptoms of acute infection and were also evaluated by otoscopic and tympanometric methods.
Before paracentesis, external auditory canal (EAC) was cleansed with alcohol in all patients with OME and AOM. In patients with OME, 2% lidocaine solution with 1:100,000 epinephrine was filled into the EAC, and paracentesis was performed after 5-7 minutes time had elapsed. In patients with AOM, 2% lidocaine with 1:100,000 epinephrine solution was injected into the external auditory canal skin, and then EAC was filled with 2% lidocaine with 1:100,000 epinephrine and paracentesis was performed after 5-7 minutes time elapse. After that, EAC was rinsed with physiological saline and cleaned thoroughly by suction. Ventilation tubes were placed after paracentesis in all patients with OME, under general anaesthesia within operating room conditions. Paracentesis which was performed on the most prominent point of the bulging tympanic membrane was conducted on patients with AOM under local anaesthesia on an outpatient basis. Middle ear fuid was aspirated by using a setting we designed (Figure 1). This setting included a 1,3 mm suction cannula, a 2,5 mL injector whose piston was ejected and an adaptor for suction cannulas. In this setting, the 1,3 mm suction cannula was connected to the tip of the 2,5 mL injector, and the adaptor connected to the suction device via a rubber tube was attached to the bottom of the 2,5 injector. According to paracentesis findings, middle ear fluids were classified into three groups as serous, gluey and purulent. Of the 30 ears of the 16 patients with OME, gluey material was aspirated from 20 ears, serous fluid was aspirated from 8 ears, and purulent material was aspirated from 2 ears. Of the 20 ears with gluey fluid, four ears excluded from the study because of the contamination of the middle ear fluid with blood during aspiration. Purulent material was aspirated from all patients with AOM. Aspirated middle ear fluid was diluted with physiological saline to the total amount of 0,5 mL. Blood and middle ear fluid samples were taken to the microbiology laboratory.
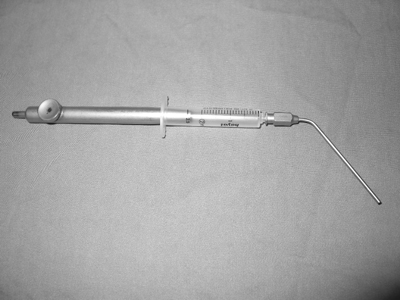 Büyütmek İçin Tıklayın |
Figure 1: The setting designed for aspiration of the middle ear fuid |
The levels of C3 and C4 in blood and middle ear fluid were measured by nephelometric method using DADE BEHRING kits (Dade Behring Marburg GmBH, Marburg, Germany) in a nephelometer at 37 oC. The units are expressed as g/L.
Statistical analysis was carried out with the SPSS-X (Release 4.1) programme. Goodness of fit to normal distributions were investigated by plots and the Shapiro-wilks test. Differences between the groups for C3 and C4 values were analyzed by using non-parametric tests (Kruskal-Wallis test), and Mann-Whitney U test was used for pairwise multiple comparisons (for post hoc test). The results are expressed as mean values ± standard deviation of the mean (SD). P values less than 0.05 were considered significant.
Results
The C3 and C4 levels in the serum of the patients with AOM were significantly higher than those of the patients with OME and normal controls (Table 1).Table 1: Mean serum C3 and C4 levels in patient and control group (mean ± SD)
The presence of C3 and C4 in the middle ear effusions of the patients with OME and AOM was shown, but C3 and C4 levels in middle ear effusions were significantly lower than those in serum of the same patients. According to the paracentesis findings, OME group was reclassified into three groups on the basis of the material character as gluey, serous and purulent. According to this new classification, C3 and C4 levels in purulent effusions (including AOM group) were significantly higher than those in gluey and serous effusions. In other words, decrease in C3 and C4 levels in middle ear effusions when compared to the serum levels was most evident in gluey type effusions, followed by serous and purulent types (Table 2).
C3 and C4 levels were too low to be calculated, being under the lower measurement threshold of the nephelometer in 4 ears with gluey effusion and in one ear with serous effusion.
Discussion
The complement system is comprised of more than 30 molecules that play key roles both in innate and adaptive immunity. A number of the complement products generated during activation play a major role in host defense. The larger fragments derived from C3 and C4 (i.e. C3b and C4b) are involved in biologic effector functions, such as in opsonization, phagocytosis and immune-modulation. The smaller fragments, C3a, C4a and C5a, called anaphylatoxins, are involved in mediation of inflammatory reactions. Anaphylatoxins play a major role in inflammation, including the recruitment and activation of various leukocytes. Chemotaxis of granulocytes and macrophages to sites of infection plays a crucial role in inflammatory responses. On the other hand, activation of the complement system is not entirely beneficial. Even when it is properly regulated and appropriately activated, the complement system sometimes can cause significant tissue damage. Some of the pathology associated with bacterial infections is attributable to the biologic effects of complement activation [2]. These pathologic effects include the bystander destruction of normal host cells when acute inflammatory responses to infectious organisms take place.In the present study, we found that the mean C3 and C4 levels in serum of the patients with OME were similar to those in serum of the controls and there was no statistically significant difference between the two groups. However, the mean C3 and C4 levels in serum of the patients with AOM were significantly higher than those in serum of both the patients with OME and healthy controls. This may be related with the fact that AOM is a systemic but OME is a local process. In the present study, the presence of C3 and C4 in the middle ear effusions of the patients with OME and AOM was shown. However, C3 and C4 levels in middle ear effusions were significantly lower than those in serum of the same patients. According to paracentesis findings, study group was reclassified into three groups on the basis of the material character as gluey, serous and purulent. According to this new classification, C3 and C4 levels in purulent effusions were significantly higher than those in gluey and serous effusions. In other words, decrease in C3 and C4 levels in middle ear effusions when compared to the serum levels was most evident in gluey effusions, followed by serous and purulent types. Also, other studies on OME showed that, while serum C3 and C4 values were normal, C3 and C4 levels in middle ear fluid were lower than those of the serum [11-15]. Even if the levels in effusions are less than those in serum, presence of both C3 and C4 in middle ear effusions suggests that the complement system activated by both the classical and alternative pathway may play a role in fluid accumulation. Both the higher serum C3 and C4 levels in patients with AOM (when compared to the controls) and also higher C3 and C4 levels in serous and purulent effusions (when compared to gluey effusions) indicate that, initially, complement system involves in the inflammatory process as a part of an immunologic defence system against microorganisms. The mean values for C3 and C4 serum levels were not different in patients with OME from the control group. Also, although less than in purulent material, both C3 and C4 in serous and gluey effusions were found to be present. These two findings suggest that complement activation still continues as time goes by, but as a local event. B- and T- lymphocyte, macrophage, polimorphonuclear leukocyte, IgA, IgE, IgG, IgM, lysozyme, immune complex, rheumatoid factor, antinuclear antigen and bacteria found in middle ear may lead to complement activation via both the classical pathway and the alternative pathway. On the other hand, complement activation is not always entirely useful and sometimes can cause tissue damage. Ongoing complement activation may also cause capillary dilatation, thereby leading to the occurence of effusion in the middle ear. Consequently, the complement system which is initially activated against microorganisms may lately itself play a role as a part of the pathological process.
In an experimental study on guinea pigs, Ryan et al. [11] have reported that complement system may play a role in the pathogenesis of OME. In an another study, it has been reported that complement C3 activation products are intensely deposited in the middle ear mucosa of the patient with OME, indicating a local complement activation [15]. Therefore, it has been suggested that there is a strong ongoing complement activation and consequent inflammation in the middle ear cavity, which could contribute to the chronic inflammation in OME. It has been reported that complement components in middle ear effusions probably diffuse from the blood plasma and/or are synthesized locally, e.g. by macrophages in the tissue [15].
In conclusion, the present study showed that C3 and C4 components of complement system are present in the middle ear effusions of the patients with OME. These components may have a role in the development, maintenance or the chronicity of the disease but additional research is needed to elucidate the role of complement system in OME. Should it be proven by further studies that there is a strong association between chronic OME and complement system, then complement inhibitors may have merit in the prevention and /or treatment of chronic OME.
Reference
1) Özşahinoğlu C, Soylu L, Seçinti E. Akut orta kulak iltihapları. Pratik Pediatrik Otolaringoloji. Adana: Çukurova Üniversitesi Basımevi, 1993:13-20.
2) Abbas AK, Lichtman AH, Pober JS. Cellular and Molecular İmmunology. 3.rd ed., Philadelphia: W.B. Saunders Company, 1997:313-338.
3) Bernstein JM, Tsutsumi H, Ogra Pl. The middle ear mucosal immune system in otitis media with effusion with effusion. Am J Otolaryngol 1985; 6:162-168. [ Özet ]
4) Özkarakaş H, Erol Hİ, Özcan A, Güngör A, Candan H, Poyrazoğlu E. Efüzyonlu Otitis Mediada Efüzyonun İmmunokimyasal Değerlendirmesi ve Etyolojik Nedenlere Yaklaşım. Türk Otolarengoloji Arşivi, 1993;31 (3):139-141.
5) Bernstein JM. The role of IgE-mediated hypersensitivity in the development of otitis media with effusion. Otolaryngol Clin North Am 1992; 25(1):197-211. [ Özet ]
6) Harada T, Juhn SK, Adams GL. Lysozyme levels in middle ear effusion and serum in otitis media. Arch Otolaryngol Head Neck Surg, 1990;116(1):54-6. [ Özet ]
7) Veltri RW, Sprinkle PM. Serous otitis media- immunoglobulin and lysozyme levels in middle ear effusion and serum. Ann Otol 1973; 82:297-301. [ Özet ]
8) DeMaria TF; McGhee RB Jr; Lim DJ: Rheumatoid factor in otitis media with effusion. Arch Otolaryngol 1984; 110(5):279-80. [ Özet ]
9) Palva T, Lehtinen T, Rinne J. Immune complexes in the middle ear fluid in chronic secretory otitis media. Ann Otol Rhinol Laryngol 1983; 92:42-44. [ Özet ]
10) Liu YS, Lim DJ, Lang RW, Birch HG. Chronic middle ear effusions: Immunochemical and bacterial investigation. Arch Otolaryngol 1975; 101:278-286. [ Özet ]
11) Ryan AF, Catanzaro A, Wasserman SI, Harris JP, VogelCW. The effect of complement depletion on immunologically mediated middle ear effusion and inflammation. Clin Immunol Immunopathol 1986; 40(3):410-21. [ Özet ]
12) Meri S, Lehtinen T, Palva T. Complement in chronic secretory otitis media. C3 breakdown and C3 splitting activity. Arch Otolaryngol 1984; 110:12, 774-8. [ Özet ]
13) Harada T, Ogino S, Suzawa Y, Matsunaga T, Hong KS, Inoue K. Complement anaphylatoxins activity in middle ear effusion. Auris Nasus Larynx 1985;12 Suppl 1:188-90. ( PubMed-abstrakt). [ Özet ]
14) Sun W, Liu Z, Sun Y. Determination of complements in serum and middle ear effusion of the patients with secretory otitis media. Lin Chuang Er Bi Yan Hou Ke Za Zhi 1997;11(2):59-60. ( PubMed-abstrakt). [ Özet ]
15) Närkiö Mäkelä M, Jero J, Meri S. Complement activation and expression of membrane regulators in the middle ear mucosa in otitis media with effusion. Clin Exp Immunol 1999;116:3, 401-9. [ Özet ]




