EFFECT OF POSTAURICULAR INCISION ON AURICLE PROTRUSION: ONE-YEAR EXPERIENCE
2Şanlıurfa Eğitim ve Araştırma Hastanesi, Kulak Burun Boğaz, Şanlıurfa, Turkey
3Mersin Şehir Hastanesi, Kulak Burun Boğaz, Mersin, Turkey
Summary
Objective: In this study, we aimed to determine whether auricle protrusion at three different levels (superior, middle and inferior) of patients who underwent ear surgery with the postauricular incision resulted in any significant changes compared to the healthy ear of the same patients.Methods: All cases in which the retroauricular/postauricular incision was performed during any type of ear surgery at the Otorhinolaryngology Clinic of Şanlıurfa Mehmet Akif İnan Training and Research Hospital between June 2019 and June 2020 were included in the study. The longest distance between the auricle and the mastoid skin was recorded in millimeters from the superior, middle and inferior points. All three measurements were performed in both operated and non-operated ears at the postoperative third month.
Results: Of the 61 patients evaluated in the study, 52.5% were male (n = 32) and 47.5% were female (n = 29). The mean age of the patients was 43.15 ± 9.98 years. The mean protrusion distances of the operated and non-operated ears of the patients were 11.10 ± 3.17 and 11.79 ± 1.99, respectively for the superior point, 15.02 ± 4.19 and 15.82 ± 2.62, respectively for the middle point, and 14.34 ± 4.71 and 15.38 ± 3.31 mm, respectively for the inferior point. The superior, middle and inferior protrusions of the operated and non-operated ears were similar (p > 0.05).
Conclusion: Our findings demonstrated no difference between the patients" operated and non-operated ears in terms of auricle protrusion. In future studies, further useful findings can be obtained by performing preoperative measurements and comparing them with postoperative values.
Introduction
Many patients undergo ear surgery for various reasons and with different surgical approaches. Although various types of surgery may necessitate the use of specific techniques, it is well accepted that the postauricular approach is generally a good option in the majority of surgical treatments performed on the ear [1,2]. The main reason for adopting this approach is that it provides sufficient width to perform different operations and allows the surgeon to move more comfortably [1,3].Ear surgery using the postauricular sulcus incision is widely preferred, but some researchers consider that it will be replaced by endoscopic surgery in the near future [4,5]. One of the most important reasons for this is the possibility of various undesirable outcomes and complications due to the postauricular incision. Since various important structures, including the posterior auricular muscle are cut when making the postauricular incision, this approach is reported to cause mild to severe problems, including esthetic concerns, possibility of numbness and tingling sensation in the retroauricular region, and alterations in auricle positioning [6,7]. An important reason for the preference of endoscopic surgery over the postauricular incision is that sensory and esthetic concerns are minimized, and there is little to no possibility of ear deformities since there is no incision during endoscopy.
Different deformities may occur in the auricle of patients who undergo ear surgery with the postauricular incision (scoop ear, conjoined ear, etc.). This study aimed to determine the measurements of the three different regions (superior, middle and inferior) of the operated ear in patients who underwent ear surgery for any reason using the postauricular incision. In addition, we aimed to investigate the relationship between the postauricular sulcus incision and deformities of the auricle by performing comparisons with the non-operative ear of the same patients.
Methods
All cases in which the retroauricular/postauricular incision was performed during any ear surgery at the Otorhinolaryngology Clinic of Şanlıurfa Mehmet Akif İnan Training and Research Hospital between June 15, 2019 and June 15, 2020 were included in the study. Patients who refused to participate in the study, those with any type of ear deformity due to other causes, those who had previously undergone ear surgery, and those with incomplete otorhinolaryngology-related data were excluded from the study. Ethical approval was obtained from the Ethics Committee of Toros University at the beginning of the study (approval number: 8-50, date: 16/10/2019).
Surgical procedure
In brief, the postauricular approach applied in the study regardless of the reason for the operation was as follows: The operation was started with a 3-4 cm incision on the postauricular sulcus with the patients under general anesthesia. The skin layer, muscle layer and periosteal layer on the mastoid bone were cut. After the necessary procedure was completed, these structures were repaired and closed in order.
Measurements
The longest distance between the auricle and the mastoid skin was recorded in millimeters from the superior, middle and inferior points of auricle protrusion (Figure 1). All three measurements were performed in both operated and non-operated ears at the postoperative third month.
 Büyütmek İçin Tıklayın |
Figure 1: Measurement of the superior (s), middle-point (m) and inferior (i) distances of auricle protrusion in operated and non-operated ears |
Statistical Analysis
All analyses were performed using SPSS v. 21 (SPSS Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to determine whether quantitative variables were normally distributed. Comparison of the measurements between the operated and non-operated ears was undertaken with the Mann-Whitney U test. p < 0.05 values were accepted as statistically significant.
Results
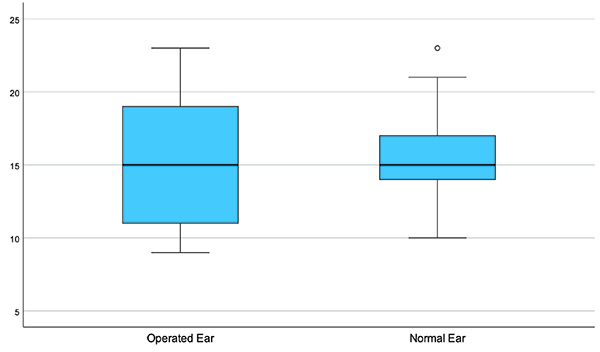
Of the 61 patients evaluated in the study, 52.5% were male (n = 32) and 47.5% were female (n = 29). The mean age of the patients was 43.15 ± 9.98 years. The mean distance of the operated and non-operated ears of the patients was as follows: 11.10 ± 3.17 and 11.79 ± 1.99, respectively for the superior point, 15.02 ± 4.19 and 15.82 ± 2.62, respectively for the middle point, and 14.34 ± 4.71 and 15.38 ± 3.31 mm, respectively for the inferior point (Figures 2-4). The superior, middle and inferior point distances of the operated and non-operated ears were found to be similar (p > 0.05, Table 1).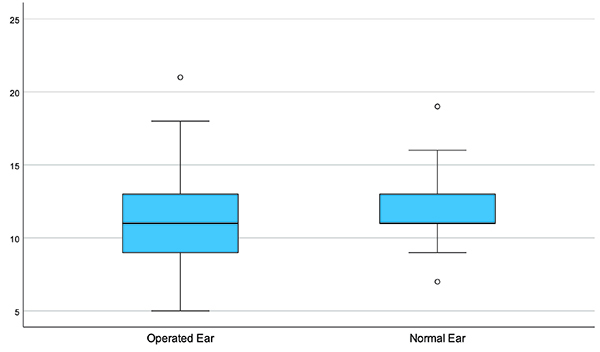 Büyütmek İçin Tıklayın |
Figure 2: Superior point measurements for the operated and non-operated ears |
 Büyütmek İçin Tıklayın |
Figure 3: Middle point measurements for the operated and non-operated ears |
 Büyütmek İçin Tıklayın |
Figure 4: Inferior point measurements for the operated and non-operated ears |
Discussion
Although the postauricular approach is generally preferred for surgical interventions to the ear in various diseases, endoscopic approaches are becoming increasingly popular due to current concerns about esthetic outcomes and possible complications related to the postauricular approach. However, in this study, this effect was found to be limited. The distances measured from the superior, middle and inferior points of the operated ears of the patients were found to be shorter, but the differences between the groups were not statistically significant.The effect of the postauricular approach on auricle protrusion anatomy has been previously discussed in different studies. El-Anwar and El-Aassar examined ear position in patients who underwent the short postauricular sulcus incision for myringoplasty. Similar to our study, they reported that there was no significant difference between the preoperative and postoperative measurements when auricle protrusion was measured from the upper, middle and lower points of the ear. The authors also reported no cosmetic and functional problems after the operations were performed with the postauricular approach [8]. Akgül et al. evaluated the postoperative outcomes of the postauricular incision only by evaluating superior and middle point measurements, and they also found that the preoperative and postoperative values were similar [1]. Furthermore, Coşkun et al. reported that the mastoid-helix distances were similar between the operated and non-operated ears after the postauricular incision [9]. In a study in which the results of the postauricular sulcus incision in a pediatric age group were evaluated with measurements performed from the same areas as in our study, Hong et al. reported no significant differences for up to one year [10]. It is clear that the results of many studies in the literature are consistent with our findings. Therefore, we can conclude that auricle deformities after the postauricular sulcus incision is not significantly effective in auricle protrusion.
In different studies comparing the cosmetic results of the postauricular incision with other approaches, different results have been reported. Contrary to studies examining only the relationship between the postauricular approach and auricle deformities, there are also those exploring whether the postauricular approach offers better or worse cosmetic outcomes compared to the other available methods. In a study by Al Amry et al., who performed similar to our study, the postauricular incision was reported to cause significantly more cosmetic deformities relative to the sulcus incision [11]. Supporting this, Inwood et al. reported that the postauricular incision more frequently caused ear shape deformations (15%) compared to ear surgery performed with the end auricular incision [12]. Despite these interesting findings, the literature is far from being conclusive on this subject since there are various studies reporting almost completely opposite results. For instance, the postauricular sulcus incision was shown to have better cosmetic results than the sulcus incision in two different studies [3,13]. These conflicting results may be associated with different methods employed to evaluate ear-related outcomes and the fact that the esthetic evaluation of the ear is rather difficult. Thus, direct a comparison between studies cannot be made without closely evaluating the methods of each particular research. This is also true for our study, in which we were not able to compare the outcomes of the postauricular incision with the other types of incisions because we did not include other methods of ear surgery in our study.
The primary aim of our study was to ascertain whether the postauricular incision could cause deformities in the ear, possibly due to the destruction of some structures that hold the ear in its regular anatomical position. One of the important structures cut during the postauricular approach is the posterior auricular muscle. It is known that ear deformities are seen more frequently when this muscle is not functional [14]. Lee et al. investigated the cosmetic results of suturing the posterior auricular muscle after postauricular ear surgery. They evaluated the outcomes of the operation based on the helical-mastoid distance and conchomastoid angle measurements. As a result of the study, it was reported that the conchomastoid angle value decreased more in the group where the posterior auricular muscle was sutured, and thus the authors suggested that the posterior auricular muscle should not be sutured if this angle was to be preserved [15]. Although many studies have reported a lack of significant differences between cosmetic measurements, Coşkun et al. determined that approximately half of the patients had postoperative cosmetic complaints even when postoperative corrections were performed [16]. Despite complaints and reported effects of the loss of this muscle, Mokhtarinejad et al. showed that the distances recorded from the healthy and operated ears were similar after operations in which the posterior auricular muscle was cut [17]. In accordance with the literature, we found that the measurements of patients who had undergone ear surgery with this incision (involving the cutting of the posterior auricular muscle) did not show a significant difference when compared to the results of the non-operated ear.
Although literature studies are mostly consistent in terms of objectively measurable results, it is noteworthy that the measured values are often reported in different ranges. El-Anwar and El-Aassar reported that the preoperative and postoperative third-month data as follows: 18.2 and 18.6 mm, respectively for the superior point, 19.8 and 19.7 mm, respectively for the mid-point, and 15.5 and 15.8 mm, respectively for the inferior point [8]. Al Amry et al. found the preoperative and postoperative third-month values to be in an even greater distribution range: 15.1 and 17.8 mm, respectively for the superior point,17.3 and 17.4 mm, respectively for the mid-point, and 18.7 and 19.2 mm, respectively for the inferior point [11]. Akgül et al. reported that the preoperative and postoperative first-year values were 15.03 and 14.67 mm, respectively for the superior point, and 17.92 and 17.25 mm, respectively for the mid-point [1]. In our study, we observed that the postoperative third-month values of the operated and non-operated ears were 11.1 and 11.8 mm, respectively for the superior point, 15.0 and 15.8 mm, respectively for the mid-point, and 14.3 and 15.4 mm, respectively for the inferior point, but no significant difference was observed. It is considered that this wide range of distribution differences between almost all studies may be due to the characteristics of different study populations, races and measurement areas. Earlier studies have shown that these features affect the shape of the ear [18,19]. Moreover, it is not possible to make a consistent comparison because characteristics, such as gender, age and body mass index, which are shown to be associated with ear measurements, are heterogeneous between study groups. [18-20].
The number of patients evaluated in our study was sufficient compared to similar studies. However, in future studies, the number of patients can be increased to perform more detailed analyses, especially to reduce the influence of race and ethnicity-based facial characteristics. An important limitation of this study is that the preoperative measurements of patients were not recorded, but this was by design since our aim was to compare the results between the two ears of the same patients. Thus, the healthy ears of each patient were evaluated as control measures. Indications for surgery, severity of the surgery, and postoperative complications may have affected the measurement results of ear deformity. Furthermore, whether the incision and suture are performed properly can affect esthetic appearance [13]. However, we did not evaluate this or compare the results of different angles or measurements that could indicate ear deformity.
Conclusion
The postauricular incision was not associated with alterations in auricle protrusion as determined by the measurement and comparison of the superior, middle and inferior auricle protrusions in the operated ear and the healthy auricle. Although we did not detect significant differences, we can state that the distance of the inferior point of the operated ear is somewhat shorter. Our results were similar to the majority of the literature on this topic; however, it is possible that future studies can provide more beneficial findings by optimizing various factors in patient inclusion, study design, and surgical comparisons. When our results are assessed, it is possible to speculate that if more operations are to be evaluated, significant differences may be obtained, especially in terms of superior and inferior protrusion measurements. Although this may be tempting, it is absolutely crucial to determine the characteristics of the tested population in terms of auricle protrusion.
Conflicts of Interest: No conflict of interest was declared by the authors
Financial Disclosure: The authors declared that this study has received no financial support
Reference
1) Akgül G, Özgür A, Yemiş T et al. Does Postauricular Incision Cause Auricula Protrusion After Tympanoplasty? The Journal of craniofacial surgery. 2019. [ Özet ]
2) Yorgancılar E, Yıldırım M, Ramazan G et al. Analysis of 36 patients underwent cochlear implantation surgery. Dicle Tıp Dergisi. 2012;39:262-8.
3) Barrett G, Koecher S, Ronan N et al. Patient satisfaction with postaural incision site. Int J Otolaryngol. 2014;2014:851980. [ Özet ]
4) Shakya D, Kc A, Nepal A. A Comparative Study of Endoscopic versus Microscopic Cartilage Type I Tympanoplasty. Int Arch Otorhinolaryngol. 2020;24:e80-e5. [ Özet ]
5) Tarabichi M, Kapadia M. Principles of endoscopic ear surgery. Current opinion in otolaryngology & head and neck surgery. 2016;24:382-7. [ Özet ]
6) Frampton SJ, Pringle M. Cutaneous sensory deficit following post-auricular incision. The Journal of Laryngology & Otology. 2011;125:1014-9. [ Özet ]
7) Yu H, Wang D, Li Q. Periotic sensory dysfunction via postauricular approach after otitis media surgery. The Laryngoscope. 2019;129:454-8. [ Özet ]
8) El-Anwar M, ElAassar A. Effect of postauricular sulcus incision for myringoplasty on auricle protrusion: 5 years' experience. Indian Journal of Otology. 2017;23:71-3.
9) Okur E, Kahveci OK, Miman MC et al. Ear protrusion after tympanoplasty and the use of mastoid dressing. Kulak Burun Bogaz Ihtis Derg. 2014;24:74-7. [ Özet ]
10) Hong P, Arseneault T, Makki F. A long-term analysis of auricular position in pediatric patients who underwent post-auricular approaches. Int J Pediatr Otorhinolaryngol. 2014;78:471-3. [ Özet ]
11) Al Amry S, Alshehri H, Al Sanosi A. Ear protrusion post tympanoplasty: Sulcus incision immediately through post auricular groove versus 5 mm post auricular. SMU Med J. 2015;2:202-10.
12) Inwood JL, Wallace HC, Clarke SE. Endaural or postaural incision for myringoplasty: does it make a difference to the patient? Clinical Otolaryngology & Allied Sciences. 2003;28:396-8. [ Özet ]
13) Shekhar C, Bhavana K. Aesthetics in ear surgery: A comparative study of different post auricular incisions and their cosmetic relevance. Indian J Otolaryngol Head Neck Surg. 2007;59:187-90. [ Özet ]
14) Guyuron B, DeLuca L. Ear projection and the posterior auricular muscle insertion. Plast Reconstr Surg. 1997;100:457-60. [ Özet ]
15) Lee JC, Cheon TU, Lee JO et al. Role of posterior auricular muscle to prevent protruding ear after retroauricular ear surgery. Auris Nasus Larynx. 2019. [ Özet ]
16) Coskun BU, Cinar U, Seven H et al. The effects of the incision types in myringoplasty operations on cosmesis. Eur Arch Otorhinolaryngol. 2006;263:820-2. [ Özet ]
17) Mokhtarinejad F, Talai HE, Seiedmohammaddoulabi S et al. Evaluation of Auriculocephalic Angle following Canal Wall Up and Canal Wall Down Mastoidectomy Procedures. The Journal of Otorhinolaryngology and Facial Plastic Surgery. 2015;2:16-8.
18) Shireen S, Karadkhelkar V. ANTHROPOMETRIC MEASUREMENTS OF HUMAN EXTERNAL EAR. Journal of Evolution of Medical and Dental Sciences. 2015;4:10333-8.
19) Taura M, Adamu L, Modibbo M. External ear anthropometry among Hausas of Nigeria: the search of sexual dimorphism and correlations. World Journal of Medicine and Medical Science Research. 2013;1:91-5.
20) Brucker MJ, Patel J, Sullivan PK. A morphometric study of the external ear: age-and sex-related differences. Plast Reconstr Surg. 2003;112:647-52; discussion 53-4. [ Özet ]




