PREDICTORS OF POSTOPERATIVE HEARING OUTCOMES AFTER ENDOSCOPIC STAPEDOTOMY SURGERY FOR OTOSCLEROSIS
2Balıkesir Atatürk Şehir Hastanesi, Kulak Burun Boğaz ve Baş Boyun Cerrahisi Kliniği, Balıkesir, Turkey
3Bozok Üniversitesi Tıp Fakültesi, Kulak Burun Boğaz ve Baş boyun Cerrahisi Anabilim Dalı, Yozgat, Turkey
Summary
Aim: To investigate predictors of postoperative hearing outcomes in endoscopic stapedotomy.Methods: Patients who underwent endoscopic stapedotomy for otosclerosis and met the inclusion criteria were included in this retrospective study.
Patients were divided into two groups according to postoperative functional success. Group 1 included patients whose postoperative air bone gap (ABG) was ≤10 dB, and Group 2 included patients whose postoperative ABG was >10 dB.
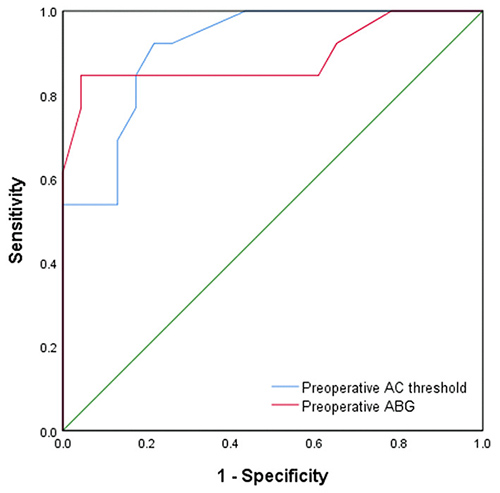
Logistic regression analysis were used to evaluate possible factors affecting postoperative hearing outcomes and receiver operating characteristics (ROC) analysis were used to identify the best cut-off threshold for predicting functional success.
Results: In both groups, statistically significant improvement was observed in mean air conduction (AC) threshold and mean ABG values after operation ( AC Group1: p<0.001, Group 2: p=0.023, ABG group1: p<0.001, group 2: p=0.002).
Group 1's mean preoperative ABG and preoperative AC thresholds were significantly lower than those of Group 2 (p<0.001 and p<0.001, respectively).
Preoperative AC thresholds and preoperative ABGs were found to be significant predictors of functional success. For AC: The area under the curve (AUC) = 0.913, 95% confidence interval (CI): 0.823-1.000, p < 0.001, and for ABG: AUC = 0.890, 95% CI: 0.753-1.000, p < 0.001.
The best cut-off thresholds in predicting the functional success of the operation were found to be 47.5 dB and 32.0 dB respectively for preoperative AC and preoperative ABG.
Conclusion: Lower preoperative ABGs and lower AC thresholds were found to be independent predictors of successful hearing outcomes for endoscopic stapedotomy.
Introduction
Otosclerosis is a unique disease affecting the otic capsule and middle ear bones, characterized by abnormal bone resorption and deposits in foci. Its histological incidence is approximately 10%, while its clinical incidence is about 1% [1,2].The most common site of involvement is the fissula ante fenestram, which is a small cleft just adjacent to the oval window, and the most common clinical finding is conductive hearing loss (CHL) [3,4]. In cases where the endosteum of the cochlea is involved, with advanced pathology and increased otoslerotic plaques, mixed type or sensorineural hearing loss (SNHL) may occur as well.
Historically, the most widely accepted surgical treatment for otosclerosis was microscopic stapes surgery [5-7].
However, with the advent of new techniques involving endoscopes in otological surgery, the endoscopic method is now often preferred in stapes surgery due to its advantage in visualizing the oval window niche, stapes, facial nerve and other anatomic structures in the middle ear. Endoscopic stapes surgery is reported to be a safe procedure with low risk of peri or postoperative complications.
Irrespective of the surgical method used, understanding the predictors of postoperative hearing outcomes is beneficial for identifying the best candidates for stapes surgery, determining the best treatment option and predicting the surgical success rate [8,9].
We reviewed studies on otosclerosis surgery and found that most of them focused on the efficacy of surgical treatment and comparison between surgical treatment methods (stapedectomy or stapedotomy, endoscopic or microscopic) [10-12].
To our knowledge, there is no previous study on predictors of postoperative hearing outcomes from surgery done with the endoscopic stapedotomy technique.
The aim of this study is to investigate whether the demographic characteristics and preoperative audiological values of the patients are predictors of postoperative hearing outcomes of endoscopic stapedotomy surgery.
Methods
The present study was carried out retrospectively at a territory reference center upon the approval of local ethics committee (approval number: 2020/74) in accordance with the principles of the Helsinki Declaration.We included information from patients meeting these inclusion criteria: between the ages of 18-65 with a presumable diagnosis of clinical otosclerosis from audiologic and radiological findings (i.e., normal external ear canal and normal otoscopic examination results, otherwise unexplained CHL, no stapes reflex and no history of ear infection) who underwent explorative tympanatomy and subsequently endoscopic stapedotomy surgery.
We excluded patients who had undergone stapes surgery previously, had ossicular chain anomalies, who had incus and malleus fixation and tympanosclerosis, those who underwent operation with microscopic techniques from the outset or intraoperatively, and patients whose audiological and demographic data were lacking.
Demographic information on the patients, preoperative and postoperative audiological examination results, operation notes and postoperative clinical information and findings were accessed from the medical records of patients meeting the above criteria. All patients were informed of the study and gave their informed consent before the analysis.
Surgical method
All operations were performed under general anesthesia. All surgical procedures were carried out transcanally by the same surgeon endoscopically using a 3 mm diameter and 14 cm long 0° and 30° rigid Hopkins II Telescope (Karl Storz, Tuttlingen, Germany).
After lidocaine 2% with epinephrine 1.25:100.000 was infiltrated locally to the external ear canal, the tympanomeatal flap was elevated to reach the middle ear cavity. If the visibility of structures was poor, the posterior superior part of the external ear canal was excised using a micro drill or curette for adequate visualization. With the help of a blunt pick, it was confirmed that the stapes was immobile and there was no movement in the round window membrane with pressure. The mobility of the malleus, incus and incudomalleolar joint were checked. The stapes tendon was dissected and the incudostapedial joint was separated. The posterior and anterior crura of the stapes were fractured and the stapes suprastructure was removed. Then the footplate was perforated with a manual perforator and microfenestration was performed with a thin curved pick. Fluoroplastic Causse loop piston (Medtronic Xomed Jacksonville, FL) was used in all cases. The size of the teflon-piston prosthesis was 0.6 mm in diameter and the length of the teflon-piston was calculated 0.25 mm longer than the distance from underside of incus to footplate, resulted in 3.75 to 4.75 mm. The piston movement was checked and confirmed. It was supported by gelfoam, and then the tympanomeatal flap was replaced.
Audiological evaluation
For the analyses in this study, the results of patients" audiometric investigations done prior to and 6 months after the operation were used.
The mean air conduction (AC) thresholds and bone conduction (BC) thresholds were calculated by averaging the values at four frequencies: 500 Hz, 1000 Hz, 2000 Hz and 4000 Hz. Air-bone gap (ABG) was calculated as the mean difference between the AC and BC thresholds at these frequencies.
A successful hearing outcome was defined as a postoperative ABG ≤10 dB [5,8,9].
Patients were divided into two groups according to postoperative functional success. Group 1 included patients whose postoperative ABG was ≤10 dB, while Group 2 included patients whose postoperative ABG was >10 dB.
The sex and age of patients, side of the operated ear (right/left), laterality of otosclerosis (bilateral or unilateral), preoperative AC thresholds, BC thresholds, ABG values and floating footplate complication occurring during the operation were investigated as probable predictive factors that could influence the functional success of the operation.
Statistical analysis
Data analysis was performed with IBM SPSS Statistics software version 17.0 (IBM Corporation, Armonk, NY, USA). The Shapiro-Wilk test was used to determine if the continuous variables followed normal distributions. The Levene test was used to examine the assumption of homogeneity of variances. Descriptive statistics for continuous variables were expressed as mean ± SD. The number of cases and percentages were used for categorical data. For the differences in continuous variables where the parametrical test assumptions were met, groups were compared with a Student's t test; otherwise the Mann Whitney U test was performed. Categorical data were analyzed with Fisher's exact or Continuity corrected χ2 test where applicable. The Wilcoxon sign rank test was used to determine if differences between pre- and post-operative clinical measurements within groups were statistically significant or not. The optimal cut-off points of pre-operative clinical measurements (i.e., AC and ABG) to determine functional success were tested with receiver operating characteristic (ROC) analysis for the maximum sum of sensitivity and specificity for the significance test. Sensitivity, specificity, and positive and negative predicted values for AC and ABG were also calculated. Univariate logistic regression analyses were used to determine the associations between clinical measurements and functional success. Odds ratios and 95% confidence intervals for each independent variable were also calculated. Whether the statistically significant effects of clinical measurements on functional success remained or not was investigated by multiple logistic regression analyses after adjustment for age and sex. A p value less than 0.05 was considered as statistically significant.
Results
Thirty-six patients were included in the study. The demographic and clinical features of the patients are shown in Table 1.Table 1: Demographic and clinical characteristics of groups
Among the 36 patients, the postoperative mean AC thresholds (30.40 ± 16.77 dB) and the postoperative mean ABG values (13.20 ± 9.03dB) were significantly better than preoperative mean AC thresholds (48.20 ± 8.49 dB, p < 0.001) and the preoperative mean ABG values (31.90 ± 8.11dB, p < 0.001), respectively.
There was no significant difference between mean preoperative and postoperative BC thresholds of the patients included in this study (17.1 ± 4.18 dB vs. 17.0 ± 9.99 dB, p = 0.105).
The mean hearing gain of the patients included in this study was 18.7 ± 7.79 dB. Of the 36 patients included in the study, 23 (63.8%) had a postoperative ABG value ≤10 dB and they were included in Group 1, while 13 (36.2%) had a postoperative ABG of >10 dB so they were included in Group 2.
There were no statistically significant differences between the two groups in terms of age, sex, affected side and localization (p > 0.05). As seen in Table 1, floating footplate complication was significantly higher in Group 2 than Group 1.
Table 2 lists preoperative and postoperative mean AC and BC thresholds and ABG values.
Table 2: Preoperative and postoperative audiometric measurements of groups
As seen in Table 2, statistically significant improvement in mean AC threshold and mean ABG values was observed in both groups after surgery.
Table 2 also shows that when the two groups were compared with each other with respect to preoperative audiological values, Group 1's mean preoperative ABG and preoperative AC thresholds were significantly lower than those of Group 2.
When univariate analyses were performed to determine if the possible factors thought to be influential on operation success had statistically significant effects, significant differences were found between the two groups in terms of preoperative AC thresholds, preoperative ABG and floating footplate complication rates, respectively: p < 0.001, p < 0.001, p = 0.040 (Table 1, Table 2).
We investigated if preoperative AC threshold and preoperative ABG were significant predictors of functional success by calculating the area under the receiver operating characteristics (ROC) curve (AUC) and 95% confidence intervals (CI); they were indeed found to be statistically significant predictors, as shown in Table 3. (Figure 1)
 Büyütmek İçin Tıklayın |
Fig 1: ROC curve for preoperative air bone gap (ABG) values and air conduction (AC) thresholds |
The best cut-off value in predicting functional success of surgery was investigated with ROC analysis and this value was found to be 47.5 dB for preoperative AC and 32.0 dB for preoperative ABG. (Table 3)
The effect of preoperative AC threshold and preoperative ABG on the functional success of the operation was evaluated with univariate logistic regression analysis:
As seen in Table 4, each 1 dB increase in the AC threshold and ABG before surgery was found to increase the likelihood of functional failure of the operation.
The effects of preoperative AC and preoperative ABG on sucess remained after adjustment for age and sex in multiple logistic regression analyses.
According to the results of univariate logistic regression analysis shown in Table 4, the probability of functional failure after the operation was significantly higher in patients whose preoperative AC value was over 47.5 dB than those whose AC value was below this figure. The statistically significant effect continued after adjustment for age and sex.
According to the results of the univariate logistic regression analysis, the probability of functional failure after surgery was significantly higher in cases where the patient's preoperative ABG value was over 32.0 dB than those whose ABG value was below 32.0 dB. After controlling for age and sex, the statistically significant effect remained.
At their 6-month follow up, 1 patient had total SNHL and vertigo. This patient had another surgery to remove the piston and obliterate the oval window with fat. No other patients had major complications. In three patients, perforation occurred in the tympanic membrane and it was repaired intraoperatively.
Discussion
Otosclerosis is the second leading cause of conductive hearing loss (CHL) after chronic otitis media [5]. In otosclerosis-associated CHL, stapes surgery provides favorable hearing results. Stapes surgery was introduced in 1956 by Shea with a stapedectomy, and over time the surgical technique changed. In this developmental process, stapedotomy became a preferred alternative to stapedectomy due to findings that the risk of complications is lower and the high frequency hearing results are better [13]. Both techniques are standard surgical procedures with demonstrated success documented in the literature [13].Traditionally, stapes surgery was carried out microscopically. However, endoscopic stapes surgery has become frequently used due to similar hearing results, fewer complications and being less invasive [6].
To determine which method may be preferred for a patient, evaluation of preoperative factors influencing success in endoscopic stapes surgery is important.
While there are studies on postoperative hearing outcomes for microscopic stapes surgery, to our knowledge there is no previous study in the literature on these factors for endoscopic stapedotomy. In the present study aiming to fill this gap, using logistic regression analysis, lower preoperative ABG and AC thresholds were found to be predictors of a successful hearing outcome in endoscopic stapedotomy surgery.
Similar to our results, Bittermann et al.[10], Kishimoto et al.[14], Mohammad Khorsandi et al.[9], Chien-Fu Yeha et al.[8] and Baklacı et al. [5] reported that smaller preoperative ABG was predictive of a postoperative successful hearing outcome (postoperative ABG of less than 10 dB). However, in all of these studies, stapes surgery was carried out microscopically.
Marchese et al.[11] carried out microscopic stapes surgery and found preoperative ABG to be a predictive factor. Yet, contrary to our results and the general literature [5,8-10] Marchese et al.[11] reported that preoperative high ABG was a predictive factor for successful hearing outcomes. The success criterion used in our study and recommended in literature is that postoperative ABG is less than 10 dB [5,7-9]. However, in the aforementioned study, the researchers used an improvement of 10 dB in ABG as a success criterion [11]. However, an improvement of 10 dB in ABG can not indicate whether postoperative mean ABG is less than 10 dB, and this may be why our results are different.
Two views have been put forward in the literature to explain the mechanisms leading to better outcomes for patients with lower preoperative ABGs. One hypothesis suggests that as thickness of the otosclerotic footplate increases, as in patients with higher ABGs, sound transmission is reduced owing to bony contact with the piston [4,15].
However, the more common and accepted view is that otosclerosis with multifocal involvement may negatively affect the hearing physiology due to other otosclerotic foci in the temporal bone [8]. Schuknecht and Barber stated that as a result of the examination of temporal bone specimens with clinical otosclerosis, more than 30% of the specimens had multiple otosclerotic foci including in the oval window and round window [14,16]. Mansour et al.[17] reported that 13% of patients with otosclerosis had an otosclerotic focus in the round window and also reported a higher postoperative ABG in patients with progressive round window involvement. In cases of otosclerosis with multifocal involvement, the desired ABG closure can not be obtained because of the continuation of negative effects of other foci on hearing physiology and function [8].
There is no definitive consensus in the literature on the most appropriate level of preoperative ABG at which stapes surgery can be recommended. In recent decades, Salmon et al. [18], Lavy et al.[19] and other surgeons reported that operations performed with preoperative ABG values lower than 25 dB yielded the same or better postoperative results as those carried out with higher preoperative ABG values. In addition, these authors proposed that surgical treatment in early periods is also beneficial for stopping the progress of disease[18-21]. In contrast, Alberti et al.[22] reported that surgical procedures performed at ABG values below 20 dB did not obtain successful hearing results in the long term. De Sata et al.[23] suggested that the ideal ABG threshold value for surgery is 30 dB. Cherukupally et al.[24] and Baklacı et al.[5] asserted that surgeries performed on ABGs of 30 dB and above are less likely to have a floating footplate complication due to more bony fixation in the footplate, so they suggested this value as the ideal ABG threshold for surgical intervention.
In the present study, the best preoperative ABG cut-off threshold for obtaining successful hearing outcome was found to be 32.0 dB (84.6% sensitivity, 95.7% specifity) with ROC analysis. This value may be used to inform patients about treatment options and the possible benefit they may derive from endoscopic stapedotomy. Patients can be informed that those with a preoperative ABG value below 32 dB may experience improvements in their hearing from the surgery, while those with a preoperative ABG above 32 dB may have a lower chance of hearing gain.
In the present study, the preoperative AC threshold was determined to be another predictive factor for successful hearing outcome and the best preoperative AC cut-off threshold for successful hearing outcomes was found to be 47.5 dB. This value is important too, in that it can be used when informing patients about treatment options. This value is especially important in helping the patients with a high preoperative BC threshold and low preoperative ABG to make decisions on treatment options such as surgery, follow up or hearing device.
In previous studies on floating footplate complication it was demonstrated that in patients whose preoperative ABG value was over 30 dB, the risk of a floating footplate complication was lower due to bony fixation in the footplate [5,24]. In the present study, a statistically significant difference was found between the two groups of patients related to floating footplate complications. However, as there was no case of floating footplate complication in our Group 1, it could not be included in the logistic regression analysis, and whether the development of floating footplate complication was an independent predictor of surgery success could not be determined.
Studies examining weather age, gender, side of the operated ear and laterality are predictors of outcomes of otosclerosis surgery were reviewed. In general, it is reported that the age is not a predictive factor for successful hearing outcome [4,5,8,9]. Although Marchese et al.[11] reported that an age less than 50 years was a predictor of hearing success and Bittermann et al.[10] reported that an age of more than 40 years was a predictor of hearing success, they were unable to explain the mechanism of this result. In our study, the age was not found to be a predictor of successful hearing outcome.
Similarly, gender is generally not found to be related to successful hearing outcomes in the literature [4,5,8]. Mohammad Khorsandi et al.[9] reported female gender as the predictor of excellent outcome, however, the possible mechanism of this was not explained in his study. In our study gender was not found to be a predictor in accordance with the literature.
Regarding the laterality and side of the operated ear; Mohammad Khorsandi et al.[9] found that bilateral otosclerosis and involvement of the right ear are predictors of excellent outcome. However, similar to Xie J et al.[4], Chien-Fu Yeha et al.[8] and Baklacı et al.[5], we didn't found the laterality of the disease and the side of the operated ear as a predictive factor.
The value of our study is the analysis of independent predictors of successful hearing outcomes specifically for endoscopic stapedotomy surgery and our findings show that lower preoperative ABG and AC thresholds are independent predictors of successful hearing outcomes.
Although we had a sufficient number of patients for our statistical analyses, the retrospective design and small number of patients are limitations of the present study. Therefore, further studies with larger patient groups and investigation of different parameters could contribute to our knowledge of predictive factors in the success of endoscopic stapedotomy.
Conclusion
We found that the results of endoscopic stapedotomy surgery are generally good. Furthermore, using multivariate logistic regression analysis we determined that lower preoperative ABG and AC thresholds were independent predictors of successful hearing outcomes for this endoscopic stapes surgery.
Declarations
Funding: This study did not receive funding.
Conflict of interest: The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank Enago (www.enago.com) for the English language review
Reference
1) Thomas J, Minovi A, Dazert S. Current aspects of etiology, diagnosis and therapy of otosclerosis. Otolaryngol Pol. 2011; 65:162-170. [ Özet ]
2) Ealy M, Smith RJ. The genetics of otosclerosis. Hear Res. 2010; 266:70-74. [ Özet ]
3) Stankovic KM, McKenna MJ. Current research in otosclerosis. Curr Opin Otolaryngol Head Neck Surg. 2006; 14:347-351. [ Özet ]
4) Xie J, Zhang LJ, Zeng N, Liu Y, Gong SS. The Clinical Characteristics of Otosclerosis and Benefit From Stapedotomy: Our Experience of 48 Patients (58 Ears). Acta Otolaryngol. 2019; 139:843-848. [ Özet ]
5) Baklacı D, Kuzucu I, Guler I, Kum RO, Ozcan M. Analysis of Factors Affecting Postoperative Functional Outcome in Patients With Otosclerosis. Auris Nasus Larynx. 2020; 47:203-208. [ Özet ]
6) Bianconi L, Gazzini L, Laura E, De Rossi S, Conti A, Marchioni D. Endoscopic Stapedotomy: Safety and Audiological Results in 150 Patients. Eur Arch Otorhinolaryngol. 2020; 277:85-92. [ Özet ]
7) Dhooge I, Desmedt S, Maly T, Loose D, Van Hoecke H. Long-term hearing results of stapedotomy: analysis of factors affecting outcome. Eur Arch Otorhinolaryngol. 2018; 275:1111-1119. [ Özet ]
8) Yeh CF, Wang MC, Chu CH, Shiao AS. Predictors of hearing outcomes after stapes surgery in otosclerosis. Acta Otolaryngol. 2019; 139:1058-1062. [ Özet ]
9) Mohammad T Khorsandi A, Mir M Jalali, Vahideh Shoshi D. Predictive Factors in 995 Stapes Surgeries for Primary Otosclerosis. Laryngoscope. 2018; 128:2403-2407. [ Özet ]
10) Bittermann AJ, Rovers MM, Tange RA, Vincent R, Dreschler WA, Grolman W. Primary stapes surgery in patients with otosclerosis: prediction of postoperative outcome. Arch Otolaryngol Head Neck Surg. 2011; 137:780-784. [ Özet ]
11) Marchese MR, Conti G, Cianfrone F, Scorpecci A, Fetoni AR, Paludetti G . Predictive role of audiological and clinical features for functional results after stapedotomy. Audiol Neurootol. 2009; 14:279-285. [ Özet ]
12) Gerard JM, Serry P, Gersdorff MC. Outcome and lack of prognostic factors in stapes surgery. Otol Neurotol. 2008; 29:290-294. [ Özet ]
13) Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy versus stapedotomy. Otolaryngol Clin North Am. 2018; 51:375-392. [ Özet ]
14) Kishimoto M, Ueda H, Uchida Y, Sone M. Factors Affecting Postoperative Outcome in Otosclerosis Patients: Predictive Role of Audiological and Clinical Features. Auris Nasus Larynx 2015;42:369-373. [ Özet ]
15) Hüttenbrink KB. Biomechanics of Stapesplasty: A Review. Otol Neurotol. 2003; 24:548-557. [ Özet ]
16) Schuknecht HF, Barber W. Histologic variants in otosclerosis. Laryngoscope. 1985; 95:1307-1317. [ Özet ]
17) Mansour S, Nicolas K, Ahmad HH. Round window otosclerosis: radiologic classification and clinical correlations. Otol Neurotol. 2011; 32:384-392. [ Özet ]
18) Salmon C, Barriat S, Demanez L, Magis D, Lefebvre P. Audiometric results after stapedotomy operations in patients with otosclerosis and preoperative small air-bone gaps. Audiol Neurotol. 2015; 20:330-3366. [ Özet ]
19) Lavy J, McClenaghan F. Stapes surgery in patients with a small air bone gap. Ear Nose Throat J. 2018; 97:198-212. [ Özet ]
20) Lippy WH, Burkey JM, Schuring AG, Rizer FM. Stapedectomy in patients with small air-bone gaps. Laryngoscope. 1997;107:919-922. [ Özet ]
21) Salvinelli F, Casale M, Di Peco V, Greco F, Trivelliet M. Stapedoplasty in patients with small air-bone gap: why not? Med Hypotheses. 2003; 60:535-537. [ Özet ]
22) Alberti A, Figuerola E, Romero-Farina G, Quer M, Larrosa F. Long-term hearing outcomes following stapedotomy in patients with otosclerosis and preoperative small air-bone gap. Audiol Neurotol. 2017; 22:350-355. [ Özet ]
23) De Seta E, Rispoli G, Balsamo G, Covelli E, De Seta D, Filipoet R. Indication for surgery in otosclerotic patients with unilateral hearing loss. Otol Neurotol. 2009;30:1116-1121. [ Özet ]
24) Cherukupally SR, Merchant SN, Rosowski JJ. Correlations between pathologic changes in the stapes and conductive hearing loss in otosclerosis. Ann Otol Rhinol Laryngol. 1998;107:319-26. [ Özet ]




