ASSOCIATION OF LOCAL ANESTHETIC INJECTION TECHNIQUE WITH POSTOPERATIVE EDEMA AND ECCHYMOSIS IN PATIENTS UNDERGOING UPPER BLEPHAROPLASTY: SHARP-TIPPED NEEDLE VERSUS BLUNT-TIPPED CANNULA
2Gaziosmanpaşa Taksim Eğitim Araştırma Hastanesi, Göz Bölümü, İstanbul, Turkey
3Gaziosmanpaşa Taksim Eğitim Araştırma Hastanesi, Plastik Cerrah Bölümü, İstanbul, Turkey
4Bezmialem Vakıf Üniversitesi, Biyoistatistik Bölümü, İstanbul, Turkey
Summary
Objective: Postoperative periorbital ecchymosis and edema following upper blepharoplasty is the most common morbidity that prolongs postoperative downtime and delays return to social life. Aim of this study was to evaluate the effect of local anesthetics injection technique on postoperative ecchymosis and edema. Local anesthetic injection with blunt-tipped cannula (BC) was compared with local anesthetic injection with sharp-tipped needle (SN).Materials and Methods: Study was designed as a prospective comparative cohort trial without randomization. Sixteen patients who required upper blepharoplasty were randomly assigned to have one upper eyelid local anesthetic injection via BC and the other via SN prior to surgery. Content of local anesthetic and surgical interventions were otherwise identical for both eyes. Standardized postoperative frontal photographs were taken on first and seventh postoperative day for each patient. These photographs were graded with side-by-side comparison for ecchymosis and edema by three blinded surgeons. Each side was graded to the contralateral side for edema and ecchymosis seperately by three choices 1) right more than left 2) left more than left 3) no difference between sides.
Results: Thirthy-two upper eyelids of sixteen patients were operated. Mean age was 59.3±6.6. Ecchymosis grading results were similar for both BC and SN side, both for postoperative day 1 and 7. Edema grading results were also similar for both BC and SN side, both for postoperative day 1 and 7. There was statistically no improvement in BC side in comparison to SN side.
Conclusion: The utilization of blunt-tipped cannulas does not reduce ecchymosis and edema in the early postoperative period.
Introduction
Upper blepharoplasty is an outpatient procedure that is widely performed in office settings under local-anesthesia. Minimal downtime and rapid return to work is the sine qua non in such facial plastic surgery procedures, following satisfactory results [1,2]. Although it is a straight forward procedure in technical perspective; extent and duration of ecchymosis and edema during especially in the first postoperative week is a disadvantage that prolongs downtime and delays rapid return to work. In line with this, studies in the literature that investigate efficiacy of solutions for this morbidity (Table 1) evaluate the first postoperative week [3-10]. Utilization of blunt-tipped cannulas (BC) has been proven useful for reducing ecchymosis for injection of fillers [11]; its utilization for local anesthetic injection during upper blepharoplasty has been previously introduced [12] but its benefit on reducing edema and ecchymosis during the early postoperative period remains to be investigated.Table 1: Investigated solutions for edema and ecchymosis
Aim of this study was to assess the effectiveness of using BC for local anesthetic injection in the reduction of ecchymosis after upper blepharoplasty in comparison to conventional sharp-tipped needle (SN). Presented study was designed as prospective and controlled study with side-by-side comparison and single-blinded evaluation with one week follow-up.
Methods
Local ethics committee approval was obtained prior to study, and all patients were informed individually about the procedures and written informed consent was obtained before the study Study was conducted in compliance with the ethical principles outlined in the Declaration of Helsinki as amended in 2013. This study was also HIPAA compliant.Undergoing skin-only upper blepharoplasty and absence of adjunctive procedures were the main inclusion criteria for the study. Adjunctive oculoplastic procedures were among criteria of exclusion from the study. All patients were monitored for history of abnormal bleeding and preoperative bleeding panel was checked before surgery. All patients were handled by the standard local anesthetic injection protocol and surgical technique.
Injection Protocol: Each individual upper eyelid was infiltrated with 1.5 cc of local anesthetic containing buffered 20mg/ml lidocaine and 0.0125 mg/ml epinephrine 27-gauge sharp-tipped needle was utilized for the sharp-tipped needle side and same-caliber (27G) blunt-tipped cannula was used for the contralateral side. Right side of the patient was injected first, and left side was injected later always. Right side was operated first, and left side was operated later always. Allocation of injection technique to either right or left side was randomly assigned. Injection technique was always similar: the skin was pierced laterally at a single site and local anesthetic was slowly infiltrated subcutaneously above orbicular muscle as the needle / cannula was advanced medially. Medial movement of the tip of the needle / cannula always supervened hydrodissection of the subcutaneous plane in order to avoid stinging vessels.
Surgical Technique: Skin-only incision was carried out with a no.15 blade in a medial-to-lateral direction. Superior and inferior skin-only incision was finalized. Dissection scissors were used to transect laterally and dissection scissors were inserted in a lateral-to-medial direction. Delicate blunt spreading action was used for subcutaneous dissection above orbicularis oculi muscle. Upper and lower holding skin was cut with scissors. Following skin resection, upper eyelids were cleaned with wet-gauze for detection of any bleeding-site and bleeding control was achieved with bipolar cautery. Skin was sutured in a continous manner with 6-0 Prolene which was removed on postoperative 7th day. Postoperative suggestions, orders and medications were identical for both groups.
Assessment of Postoperative Periorbital Ecchymosis and Edema: Standardized frontal photos were taken on postoperative day (POD) 1 and 7. Evaluation of postoperative periorbital ecchymosis and edema was carried out in a blinded fashion by three coauthors (BO, HY, OC) using the standardized patient photos taken at standardized times (Figure 1). The photos were cropped and flipped horizontally so the right and left side would swap to enable blinded evaluation by the surgeons themselves. The surgeons were given three grading options: Each side was graded to the contralateral side for edema and ecchymosis seperately by three choices 1) right more than left 2) left more than left 3) no difference between sides. The side with less edema and ecchymosis got 1 point, the side with more edema and ecchymosis got -1 point and when there was no difference both sides got 0 points.
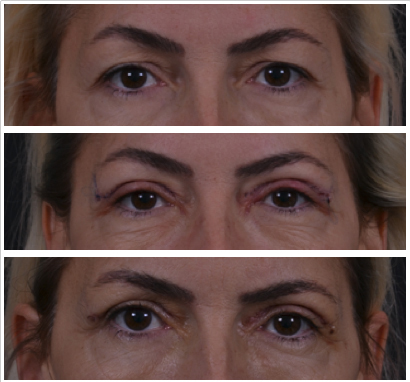 Büyütmek İçin Tıklayın |
Figure 1: Standardized postoperative photos Preoperative, Postoperative day 1, Postoperative day 7 |
Statistical Analysis: All statistical analyses were carried out by a biostatistician (OU). Descriptives were presented as median min max. Mann Whitney U test was used to compare between groups, Wilcoxon test was used to compare within groups. All statistical analysis was done with SPSS software (version 20.0; SPSS, Inc). P < .05 was considered statistically significant.
Results
Thirty-two (n=32) upper eyelids of sixteen patients were operated. Mean age was 59.3±6.6. No intraoperative or postoperative complication (0%) was observed. POD 1 and 7 ecchymosis grading scores were similar for both sided, p=0,379 and p=0,643, respectively. POD 1 and 7 edema grading scores were also similar for both sided p=0,643 and p=1,000, respectively. Postoperative edema and ecchymosis grading scores and descriptives are further detailed in (Table 2 and 3).
Table 2: Periorbital Ecchymosis grading scores
POD = Postoperative day
Table 3: Periorbital Edema grading scores
POD = Postoperative dayn
Discussion
Unlike surgery of the bodily parts of the body that can be easily covered; ecchymosis and edema of the periorbital region can only be partially camouflaged with glasses on the short term. It is the most important factor that prolongs postoperative downtime and delays rapid return to work in patients undergoing upper blepharoplasty. Many solutions with preoperative, intraoperative and postoperative solution targets were investigated in the literature to reduce postoperative ecchymosis and edema following upper blepharoplasty (Table 1). In line with the timing of morbidity, nearly all studies in the literature that investigate efficiacy of solutions for this morbidity evaluate the first postoperative week [3-10] (Table 1). This is the clinically relevant period that affects patients" surgery related quality of life. Table 1 shows the literature for most frequently used days for edema and ecchymosis studies are POD 1, 3 and 7.Utilization of BC for pain free infiltration during awake blepharoplasty has been reported before [13]. Utilization of BC for local anesthetic injection during upper blepharoplasty to reduce ecchymosis and edema immediately after injection and after skin incision was recently evaluated by Yu et al. [12]. Yet, its benefit on reducing edema and ecchymosis on first postoperative week ?which is the clinically relevant period- was not investigated and this was also reported as a limitation of the study. Utilization of BC have proven to be beneficiary in terms of ecchymosis and edema during procedures such as filler injections, but its effect on edema and ecchymosis in injection before upper blepharoplasty surgery seems statistically insignificant.
Vrcek et al commented throughly on the importance of the injection technique of bruise formation [14,15]. The injection technique utilized in this study might be speculated responsible for the contradictory results with Yu et al."s study. Medial movement of the tip of the needle always supervened hydrodissection of the subcutaneous plane in order to avoid stinging vessels with the sharp needle.
Intraoperative and peroperative measures such as utilization of electrocautery [3], postoperative electromagnetic energy [4], arnica montana application via capsules or cream[6,10], autologous platelet concentrate [8], melilotus extract [9], ice-packing [16] did not have a significant effect on the amount of edema and bruising in the postoperative period. Utilization of blunt cannula for infiltration, also, does not seem to be significant for postoperative morbidity.
Patient characteristics is another parameter that affects final edema and ecchymosis. Postoperative blood pressure, bed head elevation and cooling are parameters that clinically are known to affect the surgery-related morbidity. Further studies are required to find better solutions for postoperative morbidity following blepharoplasty procedure.
Limitations
Limited number of patients and limited number of postoperative evaluations are the sole limitation of the study. Yet, our results ?even with a limited sample size- clearly show that utilization of blunt-cannulas does not reduce postoperative edema and echymosis in the first postoperative week.
For practical reasons POD 1 and 7 were preffered in our study; which is in alignment with previous literature [3,7,16]. Nevertheless, additional evaluation of edema and ecchymosis on POD 3 would be an improvement.
Reference
1) Paik AM, Hoppe IC, Pastor CJ. An analysis of leading, lagging, and coincident economic indicators in the United States and its relationship to the volume of plastic surgery procedures performed: an update for 2012. Ann Plast Surg. 2013;71(3):316-319. doi:10.1097/SAP.0b013e31828b02d7. [ Özet ]
2) Minabe T, Momosawa A, Harii K. Endoscopic and ultrasonic removal of a lipoma on the forehead with no facial scarring: Practicality of patient's early return to work. Scand J Plast Reconstr Surg Hand Surg. 2009;43(1):22-28. doi:10.1080/02844310802514421. [ Özet ]
3) Arat YO, Sezenoz AS, Bernardini FP, Alford MA, Tepeoglu M, Allen RC. Comparison of Colorado Microdissection Needle Versus Scalpel Incision for Aesthetic Upper and Lower Eyelid Blepharoplasty. Ophthal Plast Reconstr Surg. 2016;33(6):430-433. doi:10.1097/IOP.0000000000000820. [ Özet ]
4) Czyz CN, Foster JA, Lam VB, et al. Efficacy of pulsed electromagnetic energy in postoperative recovery from blepharoplasty. Dermatol Surg. 2012;38(3):445-450. doi:10.1111/j.1524-4725.2011.02215.x. [ Özet ]
5) Kondapalli SSA, Czyz CN, Stacey AW, Cahill K V., Foster JA. Use of kaolin-impregnated gauze for improvement of intraoperative hemostasis and postoperative wound healing in blepharoplasty. J Clin Aesthet Dermatol. 2016;9(6):51-55. [ Özet ]
6) Kotlus BS, Heringer DM, Dryden RM. Evaluation of homeopathic arnica montana for ecchymosis after upper blepharoplasty: A placebo-controlled, randomized, double-blind study. Ophthal Plast Reconstr Surg. 2010;26(6):395-397. doi:10.1097/IOP.0b013e3181cd93be. [ Özet ]
7) Narváez J, Wessels I, Bacon G, Chin VR, Baqai WK, Zimmerman GJ. Prospective randomized evaluation of short-term complications when using buffered or unbuffered lidocaine 1% with epinephrine for blepharoplasty surgery. Ophthal Plast Reconstr Surg. 2010;26(1):33-35. doi:10.1097/IOP.0b013e3181b80c13. [ Özet ]
8) Vick VL, Holds JB, Hartstein ME, Rich RM, Davidson BR. Use of autologous platelet concentrate in blepharoplasty surgery. Ophthal Plast Reconstr Surg. 2006;22(2):102-104. doi:10.1097/01.iop.0000202092.73888.4c. [ Özet ]
9) Xu F, Zeng W, Mao X, Fan G-K. The Efficacy of Melilotus Extract in the Management of Postoperative Ecchymosis and Edema After Simultaneous Rhinoplasty and Blepharoplasty. Aesthetic Plast Surg. 2008;32(4):599-603. doi:10.1007/s00266-008-9149-3. [ Özet ]
10) Van Exsel DCE, Pool SMW, Van Uchelen JH, Edens MA, Van Der Lei B, Melenhorst WBWH. Arnica ointment 10% does not improve upper blepharoplasty outcome: A randomized, placebo-controlled trial. Plast Reconstr Surg. 2016;138(1):66-73. doi:10.1097/PRS.0000000000002249. [ Özet ]
11) Fulton J, Caperton C, Weinkle S, Dewandre L. Filler injections with the blunt-tip microcannula. J Drugs Dermatol. 2012;11(9):1098-1103. http://www.ncbi.nlm.nih.gov/pubmed/23135654. Accessed February 20, 2018. [ Özet ]
12) Yu W, Jin Y, Yang J, et al. Occurrence of Bruise, Hematoma, and Pain in Upper Blepharoplasty Using Blunt-Needle vs Sharp-Needle Anesthetic Injection in Upper Blepharoplasty. JAMA Facial Plast Surg. November 2016. doi:10.1001/jamafacial.2016.1376. [ Özet ]
13) Mckee D, Lalonde D. Minimal Pain Local Anesthetic Injection with Blunt Tipped Cannula for Wide Awake Upper Blepharoplasty. Plast Reconstr Surg - Glob Open. 2017;5(5):e1310. doi:10.1097/GOX.0000000000001310. [ Özet ]
14) Vrcek I, Somogyi M, Nakra T. Optimizing injection technique to minimize ecchymosis in upper blepharoplasty. JAMA Facial Plast Surg. 2017;19(4):339. doi:10.1001/jamafacial.2017.0617. [ Özet ]
15) Yu W, Jin Y, Lin X. Optimizing Injection Technique to Minimize Ecchymosis in Blepharoplasty-Reply. JAMA Facial Plast Surg. 2017;19(4):339. doi:10.1001/jamafacial.2017.0620. [ Özet ]
16) Pool SM, van Exsel DC, Melenhorst WB, Cromheecke M, van der Lei B.The effect of eyelid cooling on pain, edema, erythema, and hematoma after upper blepharoplasty: a randomized, controlled, observer-blinded evaluation study. Plast Reconstr Surg. 2015 Feb;135(2):277e-81e. doi: 10.1097/PRS.0000000000000919. [ Özet ]




