THE EFFECTS OF LATERAL OSTEOTOMY ON THE AESTHETIC, PSYCHOLOGICAL, AND FUNCTIONAL OUTCOMES OF RHINOPLASTY
Summary
Introduction: We explored the effects of lateral osteotomy on ecchymosis and edema, as well as the psychosocial, functional and aesthetic outcomes of rhinoplasty.Materials and Methods: Patients were divided into two groups by nasal width. Patients with a narrow nasal dorsum and short nasal bones underwent rhinoplasty without lateral osteotomy (n = 32) (Group 1); patients with a wide nasal dorsum underwent rhinoplasty with lateral osteotomy (n = 48) (Group 2). The pre- and post-operative dorsal and ventral nasal widths were measured. Pre- and post-operative functional and aesthetic status were evaluated using the Nasal Obstruction Symptom Evaluation (NOSE), Rhinoplasty Outcome Evaluation (ROE), and Derriford Appearance Scale 24 (DAS24) questionnaires. Postoperative edema and ecchymosis were compared between the groups.
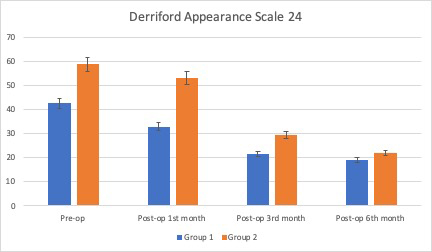
Results: Age and sex were similar between the groups (both p>0.05). The preoperative dorsal and ventral widths were greater in Group 2. The preoperative NOSE and ROE scores were similar between the two groups (both p>0.05) and the DAS24 score was lower in Group 1. Significant improvements in the NOSE, ROE, and DAS24 scores were observed postoperatively in both groups (all p<0.05). The NOSE and DAS24 scores improved more in Group 1 (both p<0.05), whereas the ROE score improvements were similar between the groups. The postoperative edema and ecchymosis scores were significantly lower in Group 1 (both p<0.05).
Conclusions: For certain patients, rhinoplasty without lateral osteotomy may be a good choice, being associated with less postoperative edema and ecchymosis, better nasal breathing, and reduced psychosocial stress.
Introduction
Rhinoplasty reshapes the nose and improves nasal function. The functional and aesthetic outcomes of rhinoplasty are equally important. Unintentional nasal shrinkage may reduce the passage of air between the nasal septum and the turbinates[1]. During rhinoplasty, cartilage and the bony hump are first removed, and the nasal vault is then repaired using grafts and/or flaps, along with osteotomy. Inadequate vault repair may cause deformities such as an open roof and an inverted V. Narrowing of the bony vault via lateral osteotomy may negatively affect the nasal valve[2]. Also, nasal mucosal damage and medialisation of the inferior turbinates caused by lateral osteotomy may decrease nasal air flow during the early postoperative period[1,3].Rhinoplasty without lateral osteotomy has been suggested for patients with narrow, straight noses[4]. For certain patients, this may yield good functional and aesthetic outcomes[4]. Here, we evaluate the effects of lateral osteotomy on ecchymosis and edema, as well as the psychosocial, functional and aesthetic outcomes of rhinoplasty.
Methods
PatientsWe retrospectively analysed 80 patients who underwent rhinoplasty between September 2017 and January 2019; two groups were defined based on lateral osteotomy status. Group 1 included 32 patients (13 males and 19 females) who did not undergo lateral osteotomy, and Group 2 consisted of 48 patients (19 males and 29 female) who did undergo lateral osteotomy. We performed low to high osteotomy in 19 patients with moderate wide nasal dorsum and small open roof, and low to low osteoethomy in 29 patients with large nasal dorsum and advanced open roof. The mean age was 28.5 ± 7.8 years in Group 1 and 28.4 ± 4.6 years in Group 2. In all cases, the follow-up period was at least 6 months.
We included all patients admitted to our otorhinolaryngology unit with nasal breathing problems or aesthetic concerns. We excluded patients undergoing revision surgery, and those with chronic sinusitis, conchal hypertrophy, or axis deviation. Noses with a ventral distance greater than 80% of the intercanthal distance were considered large (Fig. 1). The nasal bone was classified as short or long1. The midpoint of the line between the medial canthus and the nasal base served as the reference point. A nasal bone extending 3 mm caudal to the reference point was considered long and a nasal bone extending 3 mm cephalic to the reference point was classified as short. We used lateral osteotomy to treat patients with long nasal bones and a large nasal dorsum (Group 2) and, performed rhinoplasty (without lateral osteotomy) on patients with a narrow nasal dorsum and short nasal bones (Group 1). All patients were fully informed regarding our strategy prior to surgery. Written informed consent was obtained from all patients after a detailed explanation of the study objectives and protocol, delivered in accordance with the ethical principles of the Declaration of Helsinki; the study was approved by our institutional ethics committee.
 Büyütmek İçin Tıklayın |
Fig 1: Classification of nasal width (intercanthal distance). |
Study parameters
The nasal dorsum width was the preoperative distance between the dorsal nasal bones, as measured on photographs. Dorsal and ventral widths were determined as described by Kortbus et al.[5] We obtained pre- and post-operative (at months 1, 3, and 6) Nasal Obstruction Symptom Evaluation (NOSE), Rhinoplasty Outcome Evaluation (ROE), and Derriford Appearance Scale 24 (DAS24) scores. Patients rated their nasal breathing symptoms, on a scale ranging from 0 (best) to 4 (worst), on five validated questions[6]. The scores were multiplied by 5, giving a maximum possible score of 100. The ROE questionnaire evaluates physical, emotional, and social factors[7] via six questions, each scored from 0 to 4. The total score (0?24) is divided by 24 and multiplied by 100, yielding a score between 0 and 100; the higher the score, the greater the satisfaction with the surgical outcome. The DAS24 is a 24-item questionnaire measuring psychological distress associated with physical appearance[8]. Each question is scored on a 4-point scale; the total score ranges from 10 to 96, with higher scores indicating higher psychosocial distress[8]. Periorbital edema and ecchymosis ratings were obtained on postoperative days 3 and 7, respectively. The scores ranged from 0 to 5. Patients with no edema or ecchymosis scored 0; maximal edema and ecchymosis of the upper and lower eyelids was scored as 5[9]. Ecchymosis and edema were evaluated by the same surgeon, who was blinded to the group assignments.
Surgery
Rhinoplasty was performed under general anaesthesia in all patients; the nose was under local anaesthesia to prevent microbleeding. All patients underwent open septorhinoplasty. Bony and cartilaginous humps were removed using a surgical knife and a rasp. The dorsal cartilage was repaired by placing spreader grafts, and the bony dorsum was closed via lateral osteotomy in Group 2 and placement of bone dust in Group 1, as described by Tas[10]. Nasal packing was removed 10 days after surgery.
Statistical analysis
All data are presented as means with standard deviations. The normality of the data distribution was assessed using the Shapiro-Wilk test. Independent variables were analysed using Fisher"s exact test and the chi-squared test. The preoperative nasal dorsum width was compared between the two groups using the independent t-test. The Mann-Whitney U test was used to compare the ecchymosis, edema, NOSE, ROE, and DAS24 scores between the two groups. A p-value >0.05 was considered statistically significant. SPSS for Windows software (ver. 17.0; IBM Corp., Armonk, NY, USA) was used for all statistical calculations.
Results
The groups did not differ in terms of age or gender (both p>0.05), and the functional and aesthetic indications were also similar (p>0.05) (Table 1). The dorsal and ventral nasal widths were significantly greater in Group 2 than Group 1 (both p<0.05); however, the postoperative widths were similar between the groups (p>0.05) (Table 2). The preoperative NOSE scores were also similar between the groups, and improved significantly after surgery. The improvement was greater in patients who underwent rhinoplasty without, rather than with, lateral osteotomy (p<0.05) (Table 3) (Fig. 2). The postoperative rhinoplasty outcomes were similar between the two groups (p>0.05) (Figs. 3?5) (Table 3). The pre- and early post-operative DAS24 scores were higher in Group 2, although significant improvements were evident in both groups (p<0.05) (Table 3) (Fig. 6). At the 6-month visit, the DAS24 scores were similar between the two groups (p>0.05). The ecchymosis and edema scores were significantly lower in Group 1 than Group 2 (p<0.05) (Table 2).Table 1: Preoperative demographic informations and indications of the patients
Table 2: Nasal width of the patients
Table 3: Evaluation of the NOSE, ROE scores, DAS24, ecchymosis, and edema
 Büyütmek İçin Tıklayın |
Fig 2: Nasal Obstruction Symptom Evaluation (NOSE) scores of the patients. |
 Büyütmek İçin Tıklayın |
Fig 3: Pre- and post-operative appearance of a Group 1 patient. |
 Büyütmek İçin Tıklayın |
Fig 4: Pre- and post-operative appearance of a Group 2 patient. |
 Büyütmek İçin Tıklayın |
Fig 5: Rhinoplasty Outcome Evaluation (ROE) scores of the patients. |
 Büyütmek İçin Tıklayın |
Fig 6: Derriford Appearance Scale 24 (DAS24) scores of the patients. |
Discussion
We investigated lateral osteotomy on the functional, aesthetic, and psychosocial outcomes of rhinoplasty. The preoperative nasal dorsum width, age, gender, and NOSE and ROE scores were similar between the groups, but the DAS24 scores were higher in Group 2. Rhinoplasty improved the NOSE, ROE, and DAS24 scores in both groups, but the NOSE score improved more in Group 1 than Group 2. The 1- and 3-month postoperative DAS24 scores were higher in Group 2, but the 6-month scores were similar between the groups.Lateral osteotomy is traumatic and difficult to perform. Early complications may include ecchymosis and edema. Also, deformities caused by inadequate or unsuccessful osteotomy may compromise the aesthetic outcomes[11]. Mucosal injury and nasal bone collapse are possible serious complications[2]. Various techniques increasing the safety of osteotomy have been described[12,13].
Spreader flaps and grafts are commonly used to reconstruct the cartilaginous roof, support the keystone area, and reshape the dorsal aesthetic lines[14]. Sometimes, both a flap and graft are placed[14,15]. Recently, dorsum preservation rhinoplasty has increased in popularity; surgeons believe that the natural dorsum should be preserved[16]. We are of the view that the nasal bones should not be broken; reshaping of a bony dorsum with bone dust affords a natural appearance to the nose if there is no axis deviation.
Questionnaires on nasal obstruction are useful, albeit subjective; they are used to evaluate the functional outcomes of nasal surgery[17]. Previous studies reported significant improvements in NOSE scores after rhinoplasty[18,19]. A systematic review of 16 studies found that the NOSE scores varied markedly after rhinoplasty[17]. One prospective study investigated the functional outcomes of 26 patients after rhinoplasty with and without osteotomy, for patients with a large dorsum, and short nasal bones with a narrow dorsum, respectively. Rhinoplasty without lateral osteotomy afforded better nasal breathing, fewer bony vault complications, and better long-term outcomes[20]. Changes in nasal breathing were evaluated using a visual analogue scale in patients with both narrow and wide dorsa. Çakır et al. reported better functional outcomes in patients who underwent rhinoplasty with osteotomy rather than conventional osteotomy. The former technique was associated with good control of the width of the nasal base, less trauma, and fewer complications[21]. Similarly, we suggest that the basal nasal bone should not be narrowed via lateral osteotomy, to preserve respiratory function.
Rhinoplasty outcome questionnaires are useful for assessing functional and aesthetic outcomes[7]. Significant improvements in ROE scores have been reported in various studies[19,22-24]. In this study, the preoperative ROE scores were similar between the groups, and improved significantly postoperatively. Rhinoplasty with versus without lateral osteotomy showed similar functional and aesthetic outcomes. In our view, lateral osteotomy is not required if the nose is narrow. The functional and aesthetic qualities of narrow noses have previously been enhanced by placement of spreader, conchal butterfly, and alar batten flaps, as well as by cartilage injections[25]. In the absence of osteotomy, functional outcomes may be better, without any need for grafting.
Self-consciousness regarding physical appearance is greater in rhinoplasty candidates than the general population[26], and higher preoperative DAS24 scores in candidates for rhinoplasty with lateral osteotomy may reflect greater psychosocial distress. Patients with a narrow dorsum may readily accept no-osteotomy rhinoplasty, to avoid nasal bone fracture. Lower preoperative DAS24 scores correlated positively with better postoperative outcomes and patient satisfaction[26]. In this study, the pre- and early post-operative DAS24 scores were lower in Group 1 than Group 2.
Rhinoplasty patients are very concerned about early postoperative ecchymosis and edema; these conditions are minimised when lateral osteotomy is not performed. Microsaws and piezoelectric instruments have also been used to reduce postoperative ecchymosis and edema[12,13,27]. A no-osteotomy group experienced less ecchymosis and edema than an osteotomy group, as well as less pain, and shorter and better-controlled surgery; it was suggested that osteotomy was not required in patients with narrow noses[28].
Lateral osteotomy is very difficult to perform. Early career surgeons may be unable to control the surgery and any error can compromise the aesthetic outcomes. In patients with narrow noses, lateral osteotomy is not required to ensure good functional and aesthetic outcomes. We created an open roof, which was then closed using a spreader graft and bone dust. The aesthetic outcomes were similar between the groups, but nasal breathing improved more in the no-osteotomy group.
Although we included relatively few patients, the power of our study exceeded 0.80. However, we did not objectively evaluate nasal breathing.
Conclusion
Prior to rhinoplasty, the intercanthal distance and width of the nasal dorsum should be measured. Osteotomy creates pre- and post-operative stress, can trigger edema and ecchymosis, and may also adversely affect nasal breathing. Moreover, omitting osteotomy does not affect the aesthetic results. Patients with narrow noses should not undergo osteotomy. Studies with longer follow-up periods are required to evaluate the advantages and disadvantages of no-osteotomy rhinoplasty.Reference
1) Guyuron B. Nasal osteotomy and airway changes. Plast Reconstr Surg 1998;102:856-60; discussion 61-3. [ Özet ]
2) Helal MZ, El-Tarabishi M, Magdy Sabry S, et al. Effects of rhinoplasty on the internal nasal valve: a comparison between internal continuous and external perforating osteotomy. Ann Plast Surg 2010;64:649-57. [ Özet ]
3) Rohrich RJ, Janis JE, Adams WP, et al. An update on the lateral nasal osteotomy in rhinoplasty: an anatomic endoscopic comparison of the external versus the internal approach. Plast Reconstr Surg 2003;111:2461-2; discussion 3. [ Özet ]
4) Arslan E. No osteotomy rhinoplasty: indications and surgical details. Aesthetic Plast Surg 2014;38:57-62. [ Özet ]
5) Kortbus MJ, Ham J, Fechner F, et al. Quantitative analysis of lateral osteotomies in rhinoplasty. Arch Facial Plast Surg 2006;8:369-73. [ Özet ]
6) Karahatay S, Tasli H, Karakoc O, et al. Reliability and validity of the Turkish Nose Obstruction Symptom Evaluation (NOSE) scale. Turk J Med Sci 2018;48:212-6. [ Özet ]
7) Celik M, Altintas A. The Turkish Version of the Rhinoplasty Outcomes Evaluation Questionnaire: Validation and Clinical Application. Balkan Med J 2019;36:129-33. [ Özet ]
8) Carr T, Moss T, Harris D. The DAS24: a short form of the Derriford Appearance Scale DAS59 to measure individual responses to living with problems of appearance. Br J Health Psychol 2005;10:285-98. [ Özet ]
9) Higuera S, Lee EI, Cole P, et al. Nasal trauma and the deviated nose. Plast Reconstr Surg 2007;120:64S-75S. [ Özet ]
10) Tas S. The Use of Bone Dust to Correct the Open Roof Deformity in Rhinoplasty. Plast Reconstr Surg 2018;142:629-38. [ Özet ]
11) Nassif P, Kulbersh J. Rhinoplasty and bony vault complications. Facial Plast Surg 2012;28:303-9. [ Özet ]
12) Ilhan AE, Cengiz B, Caypinar Eser B. Double-Blind Comparison of Ultrasonic and Conventional Osteotomy in Terms of Early Postoperative Edema and Ecchymosis. Aesthet Surg J 2016;36:390-401. [ Özet ]
13) Avsar Y. The oscillating micro-saw: a safe and pliable instrument for transverse osteotomy in rhinoplasty. Aesthet Surg J 2012;32:700-8. [ Özet ]
14) Apaydin F. Rebuilding the Middle Vault in Rhinoplasty: A New Classification of Spreader Flaps/Grafts. Facial Plast Surg 2016;32:638-45. [ Özet ]
15) Kocak OF, Duzenli U. Assessment of Vertical Triangular Spreader Graft Technique for Reconstruction of Middle Vault and Internal Nasal Valve Angle. J Craniofac Surg 2018;29:2096-100. [ Özet ]
16) Kosins AM, Daniel RK. Decision Making in Preservation Rhinoplasty: A 100 Case Series With One-Year Follow-Up.Aesthetic Surgery Journal, 08 Apr 2019, DOI: 10.1093/asj/sjz107 [ Özet ]
17) Floyd EM, Ho S, Patel P, et al. Systematic Review and Meta-analysis of Studies Evaluating Functional Rhinoplasty Outcomes with the NOSE Score. Otolaryngol Head Neck Surg 2017;156:809-15. [ Özet ]
18) Zahedi FD, Husain S, Gendeh BS. Functional Outcome Evaluation of Septorhinoplasty for Nasal Obstruction. Indian J Otolaryngol Head Neck Surg 2016;68:218-23. [ Özet ]
19) Gunel C, Omurlu IK. The effect of rhinoplasty on psychosocial distress level and quality of life. Eur Arch Otorhinolaryngol 2015;272:1931-5. [ Özet ]
20) Eser C, Gencel E, Tabakan I, et al. The Comparison of Open Septorhinoplasty Methods with or without Osteotomies Performed in Situations of Traumatic Nasal Deformation. Cukurova Medical Journal 2015;40:738-45.
21) Cakr B, Finocchi V, Tambasco D, et al. Osteoectomy in Rhinoplasty: A New Concept in Nasal Bones Repositioning. Ann Plast Surg 2016;76:622-8. [ Özet ]
22) Saleh AM, Younes A, Friedman O. Cosmetics and function: quality-of-life changes after rhinoplasty surgery. Laryngoscope 2012;122:254-9. [ Özet ]
23) Cingi C, Songu M, Bal C. Outcomes research in rhinoplasty: body image and quality of life. Am J Rhinol Allergy 2011;25:263-7. [ Özet ]
24) Sena Esteves S, Goncalves Ferreira M, Carvalho Almeida J, et al. Evaluation of aesthetic and functional outcomes in rhinoplasty surgery: a prospective study. Braz J Otorhinolaryngol 2017;83:552-7. [ Özet ]
25) Wallace H, Sood S, Rafferty A. Management of the narrow nose. J Laryngol Otol 2009;123:945-51. [ Özet ]
26) Herruer JM, Prins JB, van Heerbeek N, et al. Does self-consciousness of appearance influence postoperative satisfaction in rhinoplasty? J Plast Reconstr Aesthet Surg 2018;71:79-84. [ Özet ]
27) Kocak I, Dogan R, Gokler O. A comparison of piezosurgery with conventional techniques for internal osteotomy. Eur Arch Otorhinolaryngol 2017;274:2483-91. [ Özet ]
28) Simsek G, Demirtas E. Comparison of surgical outcomes and patient satisfaction after 2 different rhinoplasty techniques. J Craniofac Surg 2014;25:1284-6. [ Özet ]




