EVALUATION OF POSTURAL STABILITY AND FALL RISK IN PATIENTS WITH OBSTRUCTIVE SLEEP APNEA SYNDROME
2Gaziosmanpaşa Üniversitesi Tıp Fakültesi, Göğüs Hastalıkları Anabilim Dalı, Tokat, Turkey
3Gaziosmanpaşa Üniversitesi Tıp Fakültesi, Kulak Burun Boğaz Anabilim Dalı, Tokat, Turkey
4Gaziosmanpaşa Üniversitesi Tıp Fakültesi, Fizik Tedavi ve Rehabilitasyon Anabilim Dalı, Tokat, Turkey
Summary
Objectives: To evaluate patients with obstructive sleep apnea syndrome (OSAS) for fall risk and postural stability using the Biodex Balance System.Methods: The study involved the examination of 95 individuals. Twenty-five of these individuals were healthy controls (13 male, 12 female) whose apnea hypopnea index (AHI) was below 5. In addition, 35 of them were patients with mild OSAS (17 male, 18 female); and 35 of them were patients with moderate-severe OSAS (19 male, 16 female). OSAS patients and healthy controls were examined for postural stability and fall risk using the Biodex Balance System.
Results: No statistically significant difference was observed between groups regarding sex, age, height, weight, Overall Stability Index, Antero-Posterior Stability Index, or Medio-Lateral Stability Index (p>0.05). The mean body mass index (BMI) in the control group did not show a significant difference in comparison to the mild OSAS or moderate-severe OSAS groups (p>0.05). Interestingly, the mean BMI of the mild OSAS group (27.11±2.35 kg/m2) was lower compared to the moderate-severe OSAS group (28.72±2.98 kg/m2) (p=0.039). Furthermore, a significant difference was observed between the groups for Fall Risk Index (FRI) (p<0.001). The moderate-severe OSAS group had a significantly higher FRI compared to both the mild OSAS group and the control group (p=0.044, p<0.001, respectively).
Conclusion: Postural instability and fall risk in patients with severe OSAS that engage in activities that require attention-balance can be assessed using the Biodex Balance System.
Introduction
Obstructive sleep apnea syndrome (OSAS), a sleep disorder that affects adults, has been described by sleep-associated collapse of the upper airway. OSAS has been linked to several symptoms such as snoring, fatigue, concentration or memory lapses, and excessive daytime sleepiness, and cardiopulmonary dysfunctions [1].OSAS has been demonstrated to impact free radical and oxidative stress factor levels as well as ischemic conditions, all of which alter normal central and peripheral nervous system function. Oxygen desaturation/resaturation in OSAS has been shown to elicit inflammatory components, oxidative damage, and endothelium dysregulation. Multiple reports have shown that vasa nervorum damage caused by insufficient oxygenation may result in damage peripheral nerves and the central nervous system [2,3].
Recent studies have reported an association between OSAS and idiopathic dizziness [4,5,6,7,8]. Interestingly, vestibular nuclei have been shown to be more sensitive to hypoxia than other cerebral nuclei [9]. Furthermore, the functional consequences associated with vestibular nuclei changes may be an important index of abnormal respiratory nuclei activity [8].
Postural balance control is a complex motor ability that requires flexibility in addition to organization of sensory inputs. Environmental components influencing balance include vestibular, somatosensorial and visual systems, and inputs, all of which are united in the central nervous system to determine numerous appropriate muscular responses for controlling body position and posture on a supporting base. Maintenance of postural stability requires an intact neuromuscular system, an effective motor response, and adequate supporting muscle power to restore balance when it is disturbed [10,11,12].
Weak muscles, vertigo-dizziness, visual problems, drug side effects, and environmental factors are the main causes for falls. Patients with OSAS, particularly with a moderate-severe degree, have significant risks in their daily life that require attention. For assessment of fall risk, dynamic tests are more efficient than static tests. Therefore, it has been advised that dynamic tests (Biodex Balance System) that are appropriate for locomotor tasks should also be performed during assessment of postural stability [13,14,15].
As a laboratory assessment method for postural stability, the Biodex Balance System (BBS) has been described for its reliability in assessing dynamic postural stability in healthy and visually-impaired individuals (Intraclass Correlation Coefficient (ICC) ranges from 0.59 to 0.95) [16,17].
The goal of this report was to evaluate the fall risk and postural stability OSAS patients diagnosed clinically and with polysomnography using the BBS.
Methods
1. SubjectsThe study included 95 individuals. Of these patients, 46 (48.4%) were female, and 49 (51.6%) were male. Twenty-five (13 males, 12 females) individuals with an apnea hypopnea index (AHI) below 5 constituted the healthy control group; 35 (17 males, 18 females) patients constituted mild OSAS group; and 35 (19 males, 16 females) patients constituted moderate-severe OSAS group.
Informed consent is in accordance with the study protocol, approved by the ethics committee of Gaziosmanpasa Medical Faculty (12-KAEK-126)
The study exclusion criteria were the presence of a disease that may cause central or peripheral vertigo such as chronic neurological disease, Meniere's disease, perilymph fistula, chronic middle ear infection and migraine, alcohol or substance abuse or use of any drugs that can impair balance, and presence of a chronic disease (rheumatic diseases, muscular diseases, malignancy, hepatitis, and hypertension).
2. Study design
Fall risk and postural stability was assessed using the Biodex Balance System [(BBS) Biodex Inc., New York]. The BBS comprises of a mobile balance platform controlled by a computer software that allows up to 20° tilt of the surface, which enables objective evaluation of balance. Overall Stability Index (OSI), Antero-Posterior Stability Index (APSI), Medio-Lateral Stability Index (MLSI), and Fall Risk Index (FRI) can be assessed by using this system. High scores from these tests mean impaired balance and increased fall risk. The tests were performed by identifying the coordination of subjects were standing on two bare feet on the platform, while knees were slightly flexed (10-15º), taking the most appropriate position for maintaining balance, and when eyes were open. All participants were informed about the tests and the rules that he/she must obey during the test. For postural stability and fall risk, three tests were performed, and each lasted for about 20 seconds. The participants' weight, height, GSI, APSI, MLSI, and FRI data were evaluated.
3. Statistical analysis
Data analysis was performed using SPSS 22.0 (IBM Corporation, New York, United States) software. Normality assessment was made using Shapiro-Wilk test, and a Levene test was used to test the variance homogeneity. Comparison of more than two groups for numerical data was made using a one-way ANOVA test for parametric data, and a Sidak test was used for post hoc analysis. For non-parametric data, the Kruskal Wallis H Test Monte Carlo simulation analysis was performed, while a Dun's test was used for post hoc analysis.
Statistical analyses were performed within 95% confidence level, and a p-value of less than 0.05 was accepted as significant.
Results
The mean patient age was 43.71±9.00 years, the maximum age was 62 years, and the minimum age was 21 years.The mean body mass index (BMI) of the control group was not significantly different from the mild OSAS group and severe OSAS group (p>0.05). However, the mean BMI of the mild OSAS group (27.11±2.35 kg/m2) was significantly lower in comparison to the severe OSAS group (28.72±2.98 kg/m2) (p=0.039).
There was no statistically significant difference between the groups regarding distribution of sex, age, height, weight, Overall Stability Index (OSI), Antero-Posterior Stability Index (APSI), and Medio-Lateral Stability Index (MLSI) (p>0.05) (Table 1).
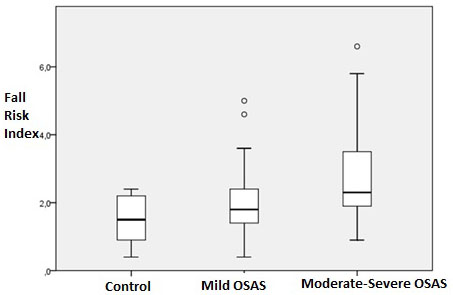
There was a statistically significant difference between the groups when compared for Fall Risk Index (FRI) (p<0.001) (Figure 1). The mean FRI of moderate-severe OSAS group was significantly higher compared to both the mild OSAS group and the control group (p=0.044 and p<0.001, respectively).
 Büyütmek İçin Tıklayın |
Figure 1: Comparison of control, mild OSAS, and moderate-severe OSAS groups based on their fall risk. |
Discussion
In patients with OSAS, hypoxia-induced impairment of peripheral and central vestibular has been documented for its association with dizziness and vertigo. The cardiovascular and neurological complications caused by hypoxia in OSAS has been well characterized. However, the consequences that arise from neurological damage have not been clearly defined [8].The functional consequences associated with vestibular nuclei changes may be an important index of abnormal respiratory nuclei activity. Interestingly, vestibular nuclei damage has been revealed previously by observing any changes in the slow and rapid eye movements [8].
Experimental OSAS studies in rats have shown that severe OSAS may affect the nervous system by inducing neural loss in the nucleus ambiguus [4].
Periodic ischemia/reperfusion that is associated with OSAS results causes many complications including inflammation, endothelial dysfunction, and oxidative stress. These complications can further affect the sympathetic and parasympathetic nervous systems, hematopoiesis, and coagulation. Early in ischemia damage, mechanisms to protect peripheral neuropathy are triggered, but become inadequate and neuropathy prevails in chronic hypoxemia [18,19].
It is reported that the postural instability causes the impaired balance and this condition is also related to the increased risk of falling. Although there are many factors affecting fall risk such as walking problems, loss of muscular activity, and drugs, there is a strong relation between postural instability and increased risk of falls. Falling phobia restricts many activities. This condition can lead to a decrease in quality of life [20,21,22].
The BBS was introduced in 1999, and is a reliable method for the assessment of fall risk and postural stability in various diseases. Several studies have used BBS to evaluate fall risk and postural stability in ankylosing spondylitis and rheumatoid arthritis patients [20,21,22]. These patients have been shown to have increased fall risk. In our study, Although postural stability indexes of moderate-severe OSAS group, OSI, APSI, and MLSI were higher than the control group, we did not detect any statistically significant impairment in the postural stability tests of patients with OSAS. However, we found that The FRI was statistically significant.increased in patients with moderate-severe OSAS. It can be said that it indicates there is a predisposition to a impairment balance.
Multiple reports have evaluated the relationship between vertigo-dizziness and OSAS with contradicting results [4,5,8,23,24,25]. It was shown that sleep deprivation in humans can cause disturbances in the posterior parietal cortex, which is known for its role in the processing of vestibular information and mediation of vestibulo-ocular reflex (VOR) [25].
Vestibular dysfunction has been shown to be more pronounced in moderate-severe OSAS patients in comparison to patients with mild OSAS [8,23].
Sensitivity of the posterior labyrinth to a hypoxic state was proven with caloric stimulation tests and showed changes in the vestibular reflex. Patients with severe OSAS had worse results in this test. Considering the sensitivity of the posterior labyrinth to a hypoxic state and the anatomical proximity of these two centers, it has been proposed that functional disturbances in the vestibular nucleus is an indicator of abnormal activity in the respiratory nucleus [8].
On the other hand, Gallina et al. [8] reported that the peripheral vestibular system became asymmetric due to hypoxic injury and the peripheral vestibular imbalance was corrected because central vestibular system was more resistant to hypoxic states.
Hypoxic injury in brain stem centers can lead to neurophysiological changes and further deterioration in sleep apnea due to injury in the respiratory centers [4].
In order to assess brain stem injury in experimental OSAS studies, data from immunohistochemical techniques, magnetic resonance spectroscopy, and audiological tests such as auditory brain stem responses (ABR) have been used [7,26].
Miceralli et al. [5] showed important impairments in VOR and classical posturographic parameters in patients with OSAS. The mean oxygen saturation has been proposed as a reliable clinical parameter, which indicates progressive disturbance in VOR and vestibulo-spinal reflex.
Mutlu et al. [4] detected abnormalities in brain stem pathways via VEMP recordings in patients with OSAS, and reported that cervical VEMP recordings can be used to detect brain stem damage in severe OSAS.
To our knowledge, no study in the literature has used the BBS to examine fall risk and postural stability in patients with OSAS. In this research, An important limitation was the absence of other vestibular tests (posturography, videonistagmography, VEMP, etc).
In the present study, we detected increased fall risk using BBS in patients with severe OSAS. Further studies investigating postural instability and fall risk in patients with OSAS using the BBS together with other vestibular tests are needed. In conclusion, it can be concluded that the BBS can contribute in preventing falls (occupational accidents) caused by dizziness in patients with severe OSAS.
Declaration of interest
Conflicts of interest: none
Role of the funding source
Source of financial support or funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Reference
1) Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am Journal Epidemiol 2013;177:10061014. [ Özet ]
2) Budhiraja R, Parthasarathy S, Quan SF. Endothelial dysfunction in obstructive sleep apnea. J Clin Sleep Med 2007;3:409415. [ Özet ]
3) Zhang JH, Fung SJ, Xi M, Sampogna S, Chase MH. Apnea produces neuronal degeneration in the pons and medulla of guinea pigs. Neurobiol Dis 2010;40:251264. [ Özet ]
4) Mutlu M, Bayır Ö, Yüceege MB, Karagöz T, Fırat H, Özdek A, Akın İ, Korkmaz H. Vestibular evoked myogenic potential responses in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol 2015;272:3137-3141. [ Özet ]
5) Micarelli A, Liguori C, Viziano A, Izzi F, Placidi F, Alessandrini M. Integrating postural and vestibular dimensions to depict impairment in moderate-to-severe obstructive sleep apnea syndrome patients. J Sleep Res 2017;26:487-494. [ Özet ]
6) Casale M, Vesperini E, Potena M, Pappacena M, Bressi F, Baptista PJ, Salvinelli F. Is obstructive sleep apnea syndrome a risk factor for auditory pathway? Sleep Breath 2012;16:413417. [ Özet ]
7) O'Donoghue FJ, Wellard RM, Rochford PD, Dawson A, Barnes M, Ruehland WR, Jackson ML, Howard ME, Pierce RJ, Jackson GD. Magnetic resonance spectroscopy and neurocognitive dysfunction in obstructive sleep apnea before and after CPAP treatment. Sleep 2012;35:4148. [ Özet ]
8) Gallina S, Dispenza F, Kulamarva G, Riggio F, Speciale R. Obstructive sleep apnea syndrome (OSAS): effects on the vestibular system. Acta Otorhinolaryngol Ital 2010;30:281284. [ Özet ]
9) Yoshida S, Sasa M, Takaori S. Different sensitivity to hypoxia in neuronal activities of lateral vestibular and spinal trigeminal nuclei. Stroke 1988;19:357-364. [ Özet ]
10) Ferdjallah M, Harris GF, Smith P, Wertsch JJ. Analysis of postural control synergies during quiet standing in healthy children and children with cerebral palsy. Clin Biomech 2002;17:203-210. [ Özet ]
11) Nashner LM, Black FO, Wall C 3rd. Adaptation to altered support and visual conditions during stance: patients with vestibular deficits. J Neurosci 1982;2:536-544. [ Özet ]
12) Shumway-Cook A, Horak FB. Assessing the ınfluence of sensory ınteraction of balance. Phys Ther 1986;66:1548-1550. [ Özet ]
13) Briggs RC, Gossman MR, Birch R, Drews JE, Shaddeau SA. Balance performance among noninstitutionalized elderly women. Phys Ther 1989;69:748756. [ Özet ]
14) Hinman RS, Bennell KL, Metcalf BR, Crossley KM. Balance impairments in individuals with symptomatic knee osteoarthritis: a comparison with matched controls using clinical tests. Rheumatology 2002;41:1388-1394. [ Özet ]
15) Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the timed up and go test. Phys Ther 2000;80:896903. [ Özet ]
16) Baldwin SL, Van Arnam TW, Ploutz-Snyder LL. Reliability of dynamic bilateral postural stability on the Biodex Stability System in older adults, Med Sci Sport Exerc 2004;36:530.
17) Aydog ST, Aydog EC, Akci A. Reproducibility of postural stability score in blind athletes. Isokinetic Exerc Sci 2004;12:229232.
18) Gozal D, Kheirandish-Gozal L. Cardiovascular morbidity in obstructive sleep apnea: oxidative stress, inflammation, and much more. Am J Respir Crit Care Med 2008;177:369 -375. [ Özet ]
19) Fanfulla F, Grassi M, Taurino AE, D'Artavilla Lupo N, Trentin R. The relationship of daytime hypoxemia and nocturnal hypoxia in obstructive sleep apnea syndrome. Sleep 2008;31:249-255. [ Özet ]
20) Aydog E, Aydog ST, Cakci A. Dynamic postural stability in blind athletes using the biodex stability system. Int J Sports Med 2006;27:415-8. [ Özet ]
21) Inanır A, Okan S, Filiz B. Evaluation of Postural Stability and Fall Risk in Patients with Rheumatoid Arthritis. Cukurova Med J 2013; 38:72-77.
22) Inanır A, Okan S, Filiz B. Evaluation of Postural Stability and Fall Risk in Patients with with Ankylosing Spondylitis. Cukurova Med J 2013; 38:86-91.
23) Kayabasi S, Iriz A, Cayonu M, Cengiz B, Acar A, Boynuegri S, Mujdeci B, Eryilmaz A. Vestibular functions were found to be impaired in patients with moderate-to-severe obstructive sleep apnea. Laryngoscope 2015;125:12441248. [ Özet ]
24) Sowerby LJ, Rotenberg B, Brine M, George CF, Parnes LS. Sleep apnea,daytime somnolence, and idiopathic dizzinessa novel association. Laryngoscope 2010;120:12741278. [ Özet ]
25) Quarck G, Ventre J, Etard O, Denise P. Total sleep deprivation can increase vestibulo-ocular responses. J Sleep Res 2006;15:369-375. [ Özet ]




