WHITE BLOOD CELL COUNT TO MEAN PLATELET VOLUME RATIO: A NOVEL MARKER FOR OBSTRUCTIVE SLEEP APNEA
2Ankara Numune Eğitim ve Araştırma Hastanesi ve Hitit Üniversitesi, Kulak Burun Boğaz Hastalıkları, Ankara, Turkey
Summary
Objective: The aim of this study was to investigate the association between white blood cell count to mean platelet volume (MPV) ratio (WMR) and other complete blood count (CBC) parameters with obstructive sleep apnea syndrome (OSAS).Materials and Methods: This cross-sectional historical cohort study was performed on 244 patients who were diagnosed as OSAS and a control group consisted of 80 individuals with simple snoring. Patients with OSAS were also divided into 3 groups according to severity of the disease. The groups were compared for WMR and the other CBC parameters, and the correlations between WMR and polysomnography (PSG) findings were investigated as well.
Results: The mean WMR and mean neutrophil to lymphocyte ratio (NLR) were significantly higher in patient groups compared with the control group (p = 0.001, p = 0.001, respectively). There was statistically significant difference between the patients groups, when the WMR values were compared (p = 0.001). The mean WMR of mild OSAS group was significantly lower compared to the moderate and severe OSAS groups (p = 0.004 and p = 0.001, respectively). There was a significant positive correlation between WMR and AHI, as well as between WMR and severity of OSAS in patient group (p = 0.001 and p = 0.001, respectively). The WMR had the highest area under ROC curve thus it thought to be more capable of discriminating the diagnosis of OSAS than the other CBC parameters. We found that WMR showed better correlation with OSAS, compared to the other CBC parameters.
Conclusion: WMR might be used as a new and important marker in OSAS since it was found high in patients with OSAS and significantly correlated with AHI and severity of the disease.
Introduction
Obstructive Sleep Apnea Syndrome (OSAS) is a systemic disease characterized by a repetitive respiratory arrest due to repeated obstruction of upper airway and resultant decrease in blood oxygen saturation during sleep[1]. It is seen approximately in 1-5% of adults[2]. Polysomnography (PSG) is the gold standard for the diagnosis of OSAS[3]. It is considered that OSAS plays a role in pathogenesis of many systemic diseases, primarily of cardiovascular and neurologic diseases[4]. Etiopathogenesis of OSAS still remains a matter of debate but presence of local or generalized inflammation in upper airway is obvious[5].Complete blood count (CBC) is a simple and cheap laboratory method frequently used in clinical practice. It is possible to get information about many diseases with this test. CBC parameters, such as neutrophil to lymphocyte ratio (NLR), mean platelet volume (MPV), white blood cell count to MPV ratio, can be used alone or in any combination to diagnose many diseases or to determine the prognosis of a disease. Several studies so far have investigated CBC parameters to identify inflammation and thrombotic tendency and CBC parameters were reported to be useful[6-8].
Several CBC parameters, such as NLR, platelet to lymphocyte ratio (PLR), MPV, MPV to platelet count ratio, platelet count and white blood cell count, were evaluated in OSAS and suggested to provide valuable information about prognosis of the disease 1,6. Previous studies revealed that white blood cell count to MPV ratio (WMR) outperformed the other CBC parameters in identification of prognosis of cardiologic diseases[8].
The aim of this study was to investigate the association between WMR and other CBC parameters in patients with OSAS. To our knowledge of literature, this is the first study investigated the elevation of WMR in OSAS.
Methods
In this cross-sectional historical cohort study, we analyzed the medical records of 551 patients, who admitted to a tertiary referral center with complaints of witnessed apnea, excessive day time sleepiness and snoring, between January 2013 and May 2016. As a result of PSG, 244 patients with apnea-hypopnea index (AHI) over 5 were included, along with 80 individuals with simple snoring (AHI < 5) as control group. Patients with OSAS group were divided into three groups according to their AHI as Mild OSAS (5 ≤ AHI < 15), moderate OSAS (15 ≤ AHI < 30) and severe OSAS (AHI ≥ 30). A total of 227 patients were excluded from the study, 15 with active infection, 7 with history of autoimmune/rheumatologic diseases, 18 with history of myocardial infarction, 8 with history of chronic obstructive pulmonary disease, 22 with diabetes mellitus, 5 with diagnosis of malignancy and 152 patients with missing data.Beckman Coulter LH 750 automated complete blood analyzer device (Beckman Coulter, CA, United States) was used to analyze CBC parameters. Venous blood samples were obtained in the morning of the day which patients undergone PSG at the night of the same day, and blood samples were analyzed within 2 hours. WMR, PLR, NLR, lymphocyte to monocyte ratio (LMR) and eosinophil to lymphocyte count ratio (ELR) were simply calculated by dividing related values to each other.
Full-night PSG was performed under the supervision of a sleep technician during spontaneous sleep. Alice 5 Model PSG device (Philips Respironics, The Netherlands) was used in the study. Electroencephalogram (EEG), submental and bilateral tibialis anterior electromyograms (EMG), electrooculogram (EOG), nasal airflow, thoracic and abdominal respiratory efforts, blood oxygen saturation (pulse oximetry) and body positions were recorded. The PSG data were scored manually according to the standard criteria set by the American Academy of Sleep Medicine by an ENT physician who had a certificate of PSG and sleep disorders. Apnea was defined as a complete cessation of airflow for at least 10 seconds. Hypopnea was defined as a decrease in airflow of at least 50% accompanied by 3% desaturation and a reduction in chest wall movement and/or arousal. The apnea-hypopnea index (AHI) was defined as the number of apneas and hypopneas per hour of sleep[9].
The groups were compared for WMR and the other CBC parameters, and the correlations between WMR and polysomnography (PSG) findings were investigated as well.
The study was approved by the local ethics committee, and conducted in accordance with the ethical principles described by the Declaration of Helsinki. Informed consents of all participants were obtained before the study (Project No: 885-2016).
IBM-SPSS for Windows version 21.0 statistical software (IBM Corporation, Armonk, NY, USA) was used for statistical analyses. Distribution of data was analyzed using Kolmogorov-Smirnov test. Continuous variables were expressed as mean ± standard deviation in the analysis. Categorical variables were expressed in percentages. Students t-test was used to compare the groups with normal distribution of continuous variables, while Mann-Whitney U test was used to compare two groups without normal distribution. Kruskal-Wallis test was used to compare three or more groups without normal distribution, while One-Way ANOVA test was used for variables with normal distribution. Pearson correlation test was used to evaluate correlations of the data. To demonstrate whether CBC parameters are capable of discriminating the diagnosis of OSAS and grading OSAS (for AHI ≥ 15 and 30), receiver operating characteristic (ROC) analysis was performed, and area under curve (AUC) was calculated. P value less than < 0.01 and P value less than < 0.05 were considered significant.
Results
There were a total of 244 patients consisting of 89 (35.5%) females and 155 males (64.5%) in the OSAS group. The control group consisted of 80 people, 39 (48.8%) females and 41 (51.2%) males. The mean ages of patients and control groups were 49.37 ± 9.90 and 33.67 ± 9.09 years, respectively.
Comparisons of CBC parameters between the patient and control groups
Table 1 shows CBC data of patient group and control. The mean WMR, NLR, WBC, neutrophil, lymphocyte, monocyte and eosinophil counts were significantly higher in patient group compared with the control group (p = 0.001, p = 0.001, p = 0.001, p = 0.001, p = 0.001, p = 0.001 and p = 0.017, respectively). Other CBC parameters (ELR, LMR, PLR, platelet count, and MPV) did not differ significantly between the two groups (p > 0.05) (Table 1).
Table 1: Comparisons of the complete blood cell counts between the patient and control group.
Comparisons of CBC parameters between the patient subgroups according to AHI score
Table 2 shows CBC and PSG data of the groups by severity of OSAS. According to AHI score of patient group; 69 patients had mild OSAS, 47 patients had moderate OSAS, and 128 patients had severe OSAS (Table 2).
The mean WMR of these three groups were 0.77 ± 0.19, 0.86 ± 0.23 and 0.89 ± 0.23, respectively. WMR values did significantly differ between two groups (p = 0.001). Compared with moderate and severe OSAS groups, mild OSAS group had significantly lower WMR values in paired comparisons which preformed to determine the difference making group (p = 0.004 and p = 0.001, respectively). In addition, WMR values did not significantly differ between groups of patients with moderate and severe OSAS (p > 0.05) (Table 2).
There was a statistically significant and positive correlation between the WMR and AHI as well as WMR and severity of OSAS (p = 0.001; r = 0.263 and p = 0.001; r = 0.219, respectively) (Figure 1, Table 3).
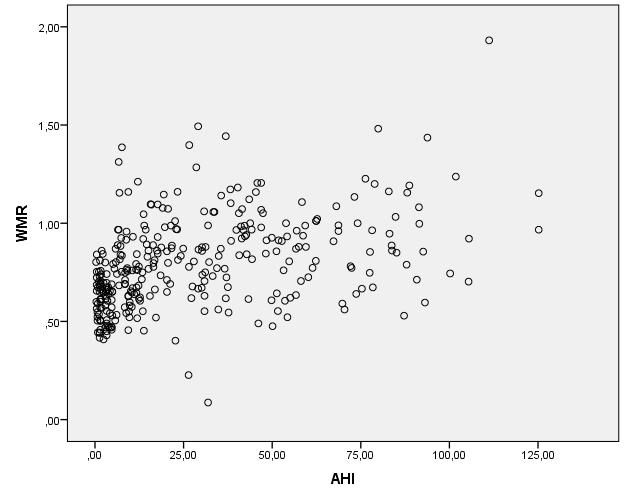 Büyütmek İçin Tıklayın |
Fig 1: Correlations between the apnea hypopnea index (AHI) and white blood cell-to-mean platelet volume ratio (WMR) among the groups. |
Table 3: The correlation coefficients and p values among the AHI, severity of OSAS and WMR.
The mean minimum oxygen saturation (Min O2) values for these 3 groups were 81.92 ± 9.32, 81.38 ± 6.64 and 70.52 ± 13.89, respectively. The mean sleep time with oxygen saturation below 90% (ST90) for these 3 groups were 19.55 ± 50.77, 15.14 ± 41.99 and 74.33 ± 104.4 minutes, respectively. There was statistically significant difference between groups, when Min O2 and ST90 values were compared (p = 0.001). According to paired comparisons to determine the group that made difference, Min O2 and ST90 values of patients with severe OSAS were statistically significantly different from values of patients with mild and moderate OSAS; there was a negative correlation between severity of OSAS and Min O2, and positive correlation between severity of OSAS and ST90. Min O2 and ST90 values did not significantly differ between groups of patients with mild and moderate OSAS (p > 0.05) (Table 2).
No statistically significant difference was found in the patients group according to severity of OSAS in terms of mean NLR, ELR, LMR, PLR, platelet count, and MPV values (p > 0.05) (Table 2).
Mean WBC, neutrophil, lymphocyte, monocyte and eosinophil counts did significantly differ between groups regarding severity of OSAS (p = 0.002, p = 0.044, p = 0.046, p = 0.018, and p = 0.014, respectively) (Table 2).
The WMR had the highest area under ROC curve thus it thought to be more capable of discriminating the diagnosis of OSAS (AUC for AHI ≥ 15 = 0.631 and AHI ≥ 30 = 0.719) than WBC, MPV, PLR and NLR (Figure 2).
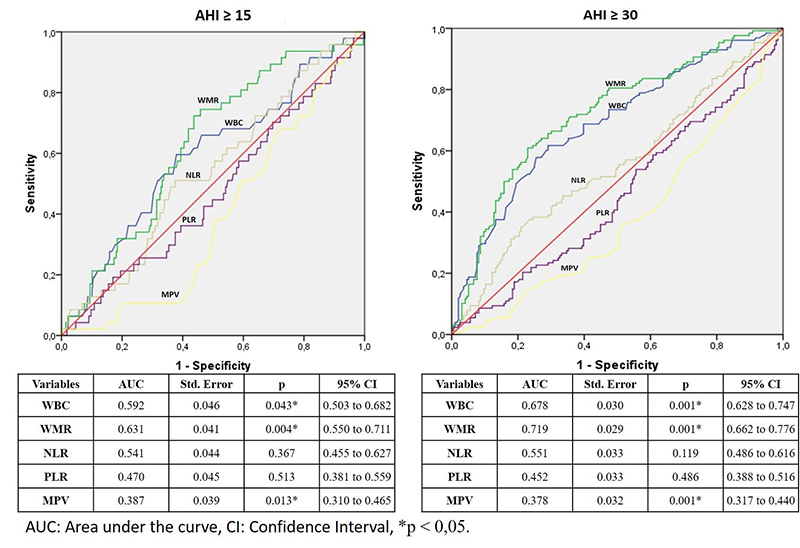 Büyütmek İçin Tıklayın |
Fig 2: Receiver operating characteristic curves of the white blood cell (WBC), mean platelet volume (MPV), white blood cell count to mean platelet volume ratio (WMR), platelet to lymphocyte ratio (PLR) and neutrophil to lymphocyte ratio (NLR) according to the apnea hypopnea index (AHI) thresholds. |
Discussion
In this study, we demonstrated WMR first in literature as an indicator shows better correlation with OSAS, compared to other CBC parameters (NLR, MPV, PLR, LMR, ELR, WBC, neutrophil, lymphocyte, and platelet counts).The etiopathogenesis of OSAS is still unclear and it may cause various morbidities like cardiovascular and neurologic diseases[10]. In OSAS, there is an increased systemic inflammation. It is thought that inflammation is triggered by repeated obstruction of upper airway, vascular endothelial injury and other accompanying comorbid diseases, and a resultant vicious cycle is created to aggravate OSAS[5]. Furthermore, hypoxia and re-oxygenation generated by repeated obstructions of upper airways were reported to increase in systemic inflammation, sympathetic activation and oxidative stress[11].
In a rat model, Nacher et al. reported that, recurrent obstructive apneas cause endothelial cell activation, suggesting the onset of an inflammatory response[12]. Another study, reported that the up-regulation of inflammatory mediators induced by recurrent obstructive apneas may lead cardiovascular disease[13].
Inflammation begins with the release of various proinflammatory cytokines (TNF-α, VEGF, IL-1, IL-6 and etc.) from relevant blood cells. Various cells, such as white blood cells, neutrophils, lymphocytes, platelets, monocytes and eosinophils, play a specific role in this process[5].
Several studies conducted using OSAS and CBC parameters are present in the literature. In those studies, associations of both severity of the disease and comorbid diseases like accompanying cardiovascular diseases, were investigated[4,5,14,15]. However, those studies have conflicting results.
Koseoglu et al. investigated the association of NLR and PLR with OSAS and they reported that there was no significant difference between patient and control groups for NLR value; however, PLR value was significantly lower in patient group compared to the control group[1].
Gunbatar et al. reported that, there was no significant difference for NLR values between the patient and control group, and when compared according to severity of OSAS, but there was a strong relation between PLR and OSAS[16]. In a similar study, PLR value was reported to associate with OSAS[4].
On the other hand, Sunbul et al. reported that there was an association between NLR and OSAS[17]. Also, Altıntas et al. reported that patients with severe OSAS have higher value of NLR compared to the patients with mild and moderate OSAS and control group as well; however, there was no difference between NLR values of patients with mild and moderate OSAS and control group[18].
In our study, despite mean NLR was significantly higher in patients with OSAS compared to the control group, mean NLR of OSAS subgroups did not significantly differ each other. Additionally, no statistically significant difference was found between PLR and OSAS. Presence of undiagnosed cardiovascular diseases like hypertension and atherosclerosis in control group and in patient groups of mild and moderate OSAS might have played a role in this result.
Yenigun et al. reported that ELR values of patients with allergic rhinitis and nasal polyposis were related to the disease[19]. Although we have found significant association between OSAS and eosinophil, monocyte, and lymphocyte counts, we could not find any relation between OSAS and ELR and LMP values. We thought that increases of those at similar rates might be the underlying reason of unchanged cellular ratios of eosinophils, monocytes and lymphocytes.
Platelets produce various substances that cause inflammation, thrombosis and atherosclerosis. Large platelets are generally indicative of increased platelet activation. Therefore, simplest parameters demonstrating the increased platelet activation are platelet count and MPV. MPV increases in some diseases, physiopathology of which inflammation, hypoxia, and vascular endothelial damage play role, such as cardiovascular diseases, pulmonary embolism and chronic obstructive pulmonary disease[20,21].
Varol et al. reported that MPV was an indicator, which demonstrates platelet activation and function, and its increase was related to increased platelet activity and OSAS[22]. On the other hand, studies which shows no significant relation between MPV and OSAS can also be seen in the literature[14,23]. In our study, we could not find any correlation between MPV and OSAS. Like previous publications, the presence of undiagnosed cardiovascular diseases like hypertension and atherosclerosis, might have played a role in this result both in control and patient groups[23]. Moreover, mean MPV, was within normal limits in all groups and this finding supports the result as well. This result may show us the need for defining diseases, which increase thrombotic tendency and cardiovascular diseases in patient and control groups, while association of MPV and OSAS is evaluated.
White blood cell count is a useful inflammatory marker in clinical practices. It is demonstrated that the values derived from WBC like NLR have prognostic value in many diseases, despite white blood cell count is within normal limits[7]. Similarly, WMR is an inflammatory marker, which has proven in prediction of morbidity and mortality and identification of prognosis in cardiovascular diseases, and it can easily be calculated using CBC; a simple and cheap routine examination, and it also has a superiority over other CBC parameters (e.g., WBC, MPV, PLR and NLR)[8]. This superiority might be due to the higher stability of WMR compared to the other CBC parameters that could be affected by various pathological and physiological conditions. As these factors can alter every single CBC parameter, the WMR might remain more stable than the others. Moreover, the WMR might represent the both inflammatory and thrombotic pathways which may exist together in the patients. Therefore, this study investigates whether WMR could be used as an inflammatory marker to differentiate OSAS patients from simple snoring and determine the severity of OSAS first time in the literature as well as the association of other CBC parameters like previous publications.
We found that WMR had the highest relation with OSAS. Moreover, we found a statistically significant and positive correlation between WMR value and AHI as well as WMR value and severity of disease. Thus the WMR might be better than the other parameters to demonstrate the severity of OSAS in the non-homogeneous groups. Another interesting result of our study is different correlation rates of values like NLR, PLR, and MPV which were previously found to be mostly related to OSAS. These findings may also show that WMR can be a more valuable indicator in OSAS than other CBC parameters such as NLR, MPV, and PLR.
Limitations of this study are as follows; it is a single-center, retrospective study and changes in parameters according to the response were not evaluated. Effects of patient depending factors on CBC parameters such as age, smoking, presence of co-morbid diseases (e.g., hypertension, stroke and hematological disorders), past received corticosteroid therapy and chronic renal insufficiency were not investigated. Prospective, multi-center, controlled studies with a larger study population are required, since this indicator is quite new in the field of OSAS.
In our study, according to our knowledge of literature, we examined the relation between WMR and OSAS first time, along with other CBC parameters. We found that WMR showed better correlation with OSAS, compared to the other CBC parameters. We hypothesize that WMR can be used as a new and important marker in OSAS since it is high in OSAS patients and significantly correlated with AHI and severity of the disease.
This article was presented at 5th Sleep Disorders Congress, May 2529, 2016, Trabzon, Turkey.
Acknowledgments: None.
Ethical approval: Our study was approved by the Ethics Committee of the Ankara Numune Education and Research Hospital, and conducted in accordance with the ethical principles described by the Declaration of Helsinki (Project No: 885-2016). Informed consent was obtained from all individual participants included in the study.
Conflict of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Reference
1) Koseoglu S, Ozcan KM, Ikinciogullari A, Cetin MA, Yildirim E, Dere H. Relationship Between Neutrophil to Lymphocyte Ratio, Platelet to Lymphocyte Ratio and Obstructive Sleep Apnea Syndrome. Adv Clin Exp Med 2015; 24: 623-627. [ Özet ]
2) Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. The New England journal of medicine 1993; 328: 1230-1235. [ Özet ]
3) Yilmaz YF, Kum RO, Ozcan M, Gungor V, Unal A. Drug-induced sleep endoscopy versus Muller maneuver in patients with retropalatal obstruction. Laryngoscope 2015; 125: 2220-2225. [ Özet ]
4) Koseoglu HI, Altunkas F, Kanbay A, Doruk S, Etikan I, Demir O. Platelet-lymphocyte ratio is an independent predictor for cardiovascular disease in obstructive sleep apnea syndrome. J Thromb Thrombolysis 2015; 39: 179-185. [ Özet ]
5) Hatipoglu U, Rubinstein I. Inflammation and obstructive sleep apnea syndrome pathogenesis: a working hypothesis. Respiration 2003; 70: 665-671. [ Özet ]
6) Kum RO, Ozcan M, Baklaci D, Yurtsever Kum N, Yilmaz YF, Unal A, Avci Y. Investigation of neutrophil-to-lymphocyte ratio and mean platelet volume in sudden hearing loss. Braz J Otorhinolaryngol 2015; 81: 636-641. [ Özet ]
7) Kum RO, Yurtsever Kum N, Ozcan M, Yilmaz YF, Gungor V, Unal A, Ciliz DS. Elevated neutrophil-to-lymphocyte ratio in Bell's palsy and its correlation with facial nerve enhancement on MRI. Otolaryngol Head Neck Surg 2015; 152: 130-135. [ Özet ]
8) Cicek G, Acikgoz SK, Yayla C, Kundi H, Ileri M. White blood cell count to mean platelet volume ratio: A novel and promising prognostic marker for st-segment elevation myocardial infarction. Cardiol J 2016. [ Özet ]
9) Berry RB, Brooks R, Gamaldo CE, Hardling S, Marcus C, Vaughn B. The AASM Manual for the Scoring of Sleep and Associated Events. Rules, Terminology and Technical Specifications, Darien, Illinois, American Academy of Sleep Medicine 2012.
10) Kiely JL, McNicholas WT. Cardiovascular risk factors in patients with obstructive sleep apnoea syndrome. Eur Respir J 2000; 16: 128-133. [ Özet ]
11) McNicholas WT. Obstructive sleep apnea and inflammation. Prog Cardiovasc Dis 2009; 51: 392-399. [ Özet ]
12) Nacher M, Serrano-Mollar A, Farre R, Panes J, Segui J, Montserrat JM. Recurrent obstructive apneas trigger early systemic inflammation in a rat model of sleep apnea. Respir Physiol Neurobiol 2007; 155: 93-96. [ Özet ]
13) Lavie L. Obstructive sleep apnoea syndrome--an oxidative stress disorder. Sleep Med Rev 2003; 7: 35-51. [ Özet ]
14) Atan D, Sazak Kundi FC, Ozcan KM, Dere H. [The relationship between platelet count and mean platelet volume with obstructive sleep apnea syndrome]. Kulak Burun Bogaz Ihtis Derg 2015; 25: 289-294. [ Özet ]
15) Hizli O, Ozcan M, Unal A. Evaluation of comorbidities in patients with OSAS and simple snoring. ScientificWorldJournal 2013; 2013: 709292. [ Özet ]
16) Günbatar H, Ekin S, Sünnetçioğlu A, Arısoy A, Çilingir BM, Aşker S, Sertoğullarından B. The relationship between neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in patients with obstructive sleep apnea syndrome. Dicle Tıp Dergisi 2015; 42.
17) Sunbul M, Sunbul EA, Kanar B, Yanartas O, Aydin S, Bacak A, Gulec H, Sari I. The association of neutrophil to lymphocyte ratio with presence and severity of obstructive sleep apnea. Bratisl Lek Listy 2015; 116: 654-658. [ Özet ]
18) Altintas N, Çetinoğlu E, Yuceege M, Acet A, Ursavas A, Firat H, Karadag M. Neutrophil-to-lymphocyte ratio in obstructive sleep apnea; a multi center, retrospective study. European review for medical and pharmacological sciences 2015; 19: 3234-3240.
19) Yenigun A, Sezen S, Calim OF, Ozturan O. Evaluation of the eosinophil-to-lymphocyte ratio in pediatric patients with allergic rhinitis. Am J Rhinol Allergy 2016; 30: 21-25. [ Özet ]
20) Ozkan B, Uysal OK, Duran M, Sahin DY, Elbasan Z, Tekin K, Cagliyan CE, Cayli M. Relationship between mean platelet volume and atherosclerosis in young patients with ST elevation myocardial infarction. Angiology 2013; 64: 371-374. [ Özet ]
21) Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des 2011; 17: 47-58. [ Özet ]
22) Varol E, Ozturk O, Gonca T, Has M, Ozaydin M, Erdogan D, Akkaya A. Mean platelet volume is increased in patients with severe obstructive sleep apnea. Scand J Clin Lab Invest 2010; 70: 497-502. [ Özet ]
23) Sokucu SN, Ozdemir C, Dalar L, Karasulu L, Aydin S, Altin S. Is mean platelet volume really a severity marker for obstructive sleep apnea syndrome without comorbidities? Pulm Med 2014; 2014: 754839. [ Özet ]




