LARYNGEAL TUBERCULOSIS
2AİBU. İzzet Baysal Faculty of Medicine, Department of Otorhinolaryngology, Bolu, Turkey
Summary
Tuberculosis again became a major health problem in recent years. Extrapulmonary tuberculosis is gaining importance and it accounts for approximately 15% of all new cases. Laryngeal tuberculosis is one of the rarer forms of extrapulmonary tuberculosis, and today laryngeal involvement of the tuberculosis infection is less than 1% among tuberculosis patients. It may be confused with laryngeal malignancies, because it is usually seen in smoker male patients and it is generally accompanied by hoarseness and appereance of a mass at endoscopy. Usually, it is seen as a complication of pulmonary tuberculosis. When tuberculosis is as widespread as today, laryngeal tuberculosis should also be considered in differential diagnosis of patients presenting with sore throat, otalgia and hoarseness. In order to reach a definitive diagnosis microbiological and histopathological samples should be taken. We aimed in this paper, a laryngeal tuberculosis case was presented with relevant literature.Introduction
Tuberculosis remains a serious world health problem. Each year more than eight million people worldwide contact tuberculosis, and more than two million people die from the disease.[1] In Turkey, officially the number of people infected with tuberculosis yearly is about 22.000-27.000. [2] The incidence of tuberculosis varies greatly throughout the world; in general, tuberculosis is more common in developing countries than in developed countries. [3] Today laryngeal involvement of the tuberculosis infection is less than 1% among tuberculosis patients. [4] In this paper, we report a rare case of laryngeal tuberculosis, along with the review of literature relevant to the incidence, investigation, and therapy of this condition.Case Presentation
A 25-year-old male patient came to our clinic with symptoms of sore throat, otalgia, and hoarseness. He had been suffering from these symptoms for three weeks. In detailed medical history of the patient there was night sweats, weight loss of 11 kg in the last three months and hemoptysis with sputum at night. There was no smoking and alcohol history. Family history revealed a past occurrence of treated pulmonary tuberculosis in his brother and uncle's wife. During the endoscopic laryngeal examination of the patient, there were multiple hyperemic lesions covered with secretion located on the right vocal cord, interarythenoid region, and on laryngeal surface of the epiglottis. The epiglottis was destructed partially.Laryngeal mucosa was diffusely hyperemic and covered with exudas. Vocal cord movements were not affected. The laryngeal appearance prompted us to suspect of a carcinoma (Figure 1). Chest x-ray showed multiple cavities and fibrosis with nodular shadowing in the right upper lobe (Figure 2).
 Büyütmek İçin Tıklayın |
Figure 1: The macroscopic appearance of laryngeal lesion. |
 Büyütmek İçin Tıklayın |
Figure 2: Multiple cavities and fibrosis with nodular shadowing in the right upper lobe in chest x-ray. |
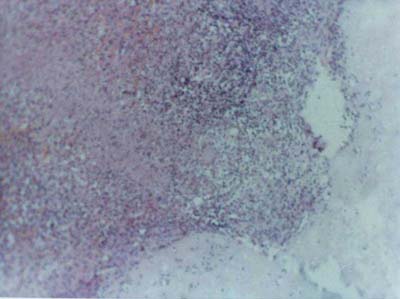
A complete blood count, biochemical parameters, and serologic tests for hepatitis B, HIV (Human Immune Deficiency Virus) and syphilis were normal or negative results. Erythrocyte sedimentation rate was high at 35 mm/hour. Acid-fast bacilli stains and Loewenstein-Jensen cultures of sputum yielded negative. Direct laryngoscopy was performed under local anesthesia. Multiple biopsies were taken from the lesions. The pathologic examination revealed caseating granulomatous lesion, inflammation with epithelioid cells, and lymphocytes and few giant cells suggesting laryngeal tuberculosis(Figure 3). Although it was not possible to show Mycobacterium tuberculosis on biopsy specimen cultures the patient was accepted as laryngeal tuberculosis on the ground of pathological findings. The patient was administered isoniasid (INH), rifampicine (RIF), pyrazinamid, and ethambutol for two months, which was followed by INH and RIF for four months. At the end of the treatment, the lesion completely disappeared.
 Büyütmek İçin Tıklayın |
Figure 3: The microscpic appearance of laryngeal lesion. |
Discussion
Laryngeal tuberculosis is an infrequent manifestation of infection by Mycobacterium tuberculosis. [1] Usually, it is seen as a complication of pulmonary tuberculosis, but sometimes only laryngeal involvement is possible.[1,2] Among the risk factors identified are the consumption of tobacco, alcohol, malnutrition and immunodeficiency.[1-4]The cases of tuberculosis had been on the decline in industrialized countries until two decades ago. The decline in tuberculosis was mostly due to the introduction of successful antituberculosis therapy, relatively high living standards, and widespread prevention programs. However, with the spread of HIV two decades ago, along with the increase in immigrants at risk, relatively poorer living standards, malnutrition -especially in the elderly- and the emergence of mycobacterial strains resistant to the common antitubercular agents, the downward trend in cases of tuberculosis was reversed and an increase in tuberculosis cases is being observed.[2-4] The increase in the incidences of tuberculosis was accompanied by an increase in the incidence of laryngeal tuberculosis. [5]
The most common symptom of laryngeal tuberculosis is dysphonia, which was present in 100% of patients in several studies. The other symptoms include dysphagia, odynophagia, stridor, cough, and hemoptysis.[4,5] Odynophagia is the most significant symptom in differential diagnosis of laryngeal tuberculosis from laryngeal carcinoma and chronic laryngittis. [6] In addition to these, family history of the patient with tuberculosis is also important.
The clinical presentation of laryngeal tuberculosis often mimics laryngeal carcinoma, chronic laryngitis, or other granulomatous diseases of the larynx. [4] Bull, Nedwicki, Bobrov and Delap et. al. presented cases in which laryngeal tuberculosis clinically mimicked laryngeal carcinoma. Therefore, these researchers stress the necessity of considering the possibility of tuberculosis in the differential diagnosis of laryngeal lesions.[2,4,7] The appearances of the lesions may vary. Whitish ulcerative lesions, non-specific inflammatory lesions, polipoid lesions, and ulcerofungative mass lesions are the most commonly observed lesions respectively. [6] Neoplastic and tubercular pathologies can sometimes coexist; however, it has been noted that coexistence of laryngeal tuberculosis and carcinoma is exceptional in patients with active pulmonary tuberculosis. [4]
The definitive diagnosis of tuberculosis is made by isolating Mycobacterium tuberculosis. However, we were unable to display the bacilli in culture. Nevertheless, the histopathological findings, such as caseation and granuloma, which are characteristics of tuberculosis, and the patient's response to the treatment proved the lesion to be tuberculosis.
The basic principles that underlie the treatment of pulmonary tuberculosis also apply to extra-pulmonary forms of the disease. However, extra-pulmonary foci usually respond to treatment more rapidly than does cavitary pulmonary tuberculosis. [8] In some studies, treatment consisting of three drugs was found to be effective against extrapulmonary tuberculosis. However, when the community rate of INH resistance is greater than 4%, empiric therapy for disease should consist of four-drug therapy. [9] In our country, drug resistant tuberculosis is a problem, [10] and since we couldn't isolate the bacilli and we could not have the susceptibility results, we added ethambutol to the first two-months of therapy.
Conclusion
Tuberculosis can involve virtually any organ and it manifests itself in various forms. When tuberculosis is as widespread as today, laryngeal tuberculosis should also be considered in differential diagnosis of patients presenting with sore throat, otalgia and hoarseness. In order to reach a definitive diagnosis microbiological and histopathological samples should be taken.We acknowledge the histopathological examination and diagnosis by Dr. Faruk Atay.
Reference
1) Palendira U, Spratt JM, Britton WJ, Triccas JA. Expanding the antigenic repertoire of BCG improves protective efficacy against aerosol Mycobacterium tuberculosis infection. Vaccine 2005;14:1680- 85. [ Özet ]
2) Egeli E, Oghan F, Alper M, Harputluoglu U, Bulut I. Epiglottic tuberculosis in a patient treated with steroids for Addison's disease. Tohoku J Exp Med 2003; 2:119-25. [ Özet ]
3) Konishi K, Yamane H, Iguchi H, Nakagawa T, Shibata S, Takayama M, Sunami K, Nakai Y. Study of tuberculosis in the field of otorhinolaryngology in the past 10 years. Acta Otolaryngol (Stockh) 1998; Suppl 538: 244– 9. [ Özet ]
4) Rizzo PB, Da Mosto MC, Clari M, Scotton PG, Vaglia A, Marchiori C. Laryngeal tuberculosis: an often forgotten diagnosis. Int J Infect Dis 2003; 2:129-31. [ Özet ]
5) Kenmochi M, Ohashi T, Nishino H, Sato S, Tanaka Y, Koizuka I, Shinagawa T. A case report of difficult diagnosis in the patient with advanced laryngeal tuberculosis. Auris Nasus Larynx 2003; l: 131-4. [ Özet ]
6) Shin JE, Nam SY, Yoo SJ, Kim SY. Changing trends in clinical manifestation of laryngeal tuberculosis. Laryngoscope 2000; 11:1950-3. [ Özet ]
7) Richter B, Fradis M, Kohler G, Ridder GJ. Epiglottic tuberculosis: differential diagnosis and treatment. Case report and review of the literature. Ann Otol Rhinol Laryngol 2001; 2:197-201. [ Özet ]
8) CDC. Treatment of tuberculosis. MMWR 522 RR 2003: 1-77.
9) CDC. From the Centers for Disease Control and Prevention. Initial therapy for tuberculosis in the era of multidrug resistance: Recommendations of the Advisory Council for the Elimination of Tuberculosis. JAMA 1993; 270: 694-8.
10) Karabay O, Otkun M, Akata F, Karlikaya C, Tuğrul M, Dündar V . Antituberculosis drug resistance and associated risk factors in the European section of Turkey. Indian J Chest Dis Allied Sci 2004; 46: 171-7. [ Özet ]




